
PERSONAL HEALTH BOOK
A Novel Tool for Patient Centered Healthcare
Juha Puustjärvi
University of Helsinki, Helsinki, Finland
Leena Puustjärvi
The Pharmacy of Kaivopuisto, Helsinki, Finland
Keywords: Patient centered healthcare, Personal health records, Information therapy, Drug therapy, Semantic web,
Ontologies, XML, RDF, OWL.
Abstract: Patient centered healthcare is based on the assumption that physicians, patients and their families have the
ability to obtain and understand health information and services, and make appropriate health decisions.
This in turn presumes that patient’s personal health information is presented according to individuals
understanding and abilities. Based on this argument our research has focused on analysing whether the
existing PHRs (Personal Health Records) support patient centered healthcare in an appropriate way. The
analysis of these questions led to the introduction of the Personal Health Book (PHB). It is an extension of
PHR in that all healthcare providers, who are involved in patient’s healthcare, augment the PHB by links to
relevant information entities. In this paper we consider two approaches for maintaining PHBs: one extends
XML based PHRs while the other exploits semantic web technologies in PHBs’ implementation. In
particular, we present the advantages that can be achieved in using semantic web technologies such as RDF
and OWL.
1 INTRODUCTION
“Patient centered healthcare” is the term that is used
to describe healthcare that is designed and practiced
with the patient at the centre (Bauman et al., 2003).
It is based on the assumption that physicians,
patients and their families have the ability to obtain
and understand health information and services, and
make appropriate health decisions (Gillespie et al.,
2004). This in turn presumes that patient’s personal
health information is presented according to
individuals understanding and abilities.
Based on this argument our research has focused
on analysing whether the existing PHRs (Personal
Health Records) (Agarwal et al., 2006; Kaelber et al,
2008; Lewis et al., 2005; Tuil et al, 2006) support
patient centered healthcare in an appropriate way.
As far as we know, this viewpoint is not addressed
in scientific articles though patient centered
healthcare is widely studied in literature, e.g., in
(Little et al., 2001; Michie et al., 2003; Stewart,
2004; Thompson, 2004; Puustjärvi and Puustjärvi,
2010).
In particular, we have analyzed the following
questions:
• What are the shortcomings of XML-
based PHRs in supporting individuals
understanding and abilities?
• What health information an ideal PHR
should contain?
• What functionalities a PHR system
should provide?
The analysis of these questions led to the
introduction of the Personal Health Book (PHB). It
is an extension of PHR in that all healthcare
providers, who are involved in patient’s healthcare,
provide appropriate content for the PHB. For
example, the extra work required from physicians is
just to augment their diagnosis by appropriate links
to relevant medical information entities, e.g., on an
information entity dealing blood pressure.
Correspondingly, in dispensing a drug a pharmacist
386
Puustjärvi J. and Puustjärvi L..
PERSONAL HEALTH BOOK - A Novel Tool for Patient Centered Healthcare.
DOI: 10.5220/0003271303860393
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2011), pages 386-393
ISBN: 978-989-8425-34-8
Copyright
c
2011 SCITEPRESS (Science and Technology Publications, Lda.)

augments the prescription by appropriate links, e.g.,
by a link to Diovan (a drug for reducing blood
pressure).
In such a PHB-based healthcare model, patient’s
physicians are responsible of patient’s information
therapy and pharmacists who dispense drugs for
patient are responsible of patient’s drug therapy.
Correspondingly all sources, such as a trainer in
patient’s gym, that are involved in patient’s
healthcare and generate data into PHB should also
augment the PHB by appropriate information.
The PHB-based healthcare model presumes that
the information entities that are used in the therapy
are accessible in the web, i.e., each entity should be
stored in the PHB or have a url (uniform resource
locator) in the PHB. This, however, does not require
the creation of new content as relevant information
entities already exist in digital form, and which can
be accessed by the systems used by the healthcare
providers. For example, in most countries such
medical information entities are maintained by
medical authorities.
From technology point of view the PHB-based
healthcare model presumes that PHBs are internet
based meaning that the PHBs are stored at a remote
server. So PHBs can be shared with healthcare
providers that are authorized by the patient. They
also have the capacity to import data from other
information sources such as from a pharmacy, a
hospital laboratory and physician office.
In this paper, we restrict ourselves on analyzing
how modern ICT-technology can be exploited in
implementing PHBs. First, in section 2, we motivate
the introduction of PHBs by considering the
problems encountered in using standard PHRs in
patient centered healthcare. By the term “standard
PHR” we refer to PHRs, which are based on a
standardized XML schema such as the schemas
presented in CCR- (CCR, 2009) and CCD-standards
(CCD, 2009). As we will illustrate, the drawback of
these standard PHRs is that they are focused on
storing health oriented data instead of supporting
health oriented information that is required in patient
centered healthcare.
In Section 3, we consider the development of
PHBs by extending standard PHR by information
therapy (Ix) (Trevena et al., 2006) and drug therapy
(Metler and Kempler, 2004). Then, in Section 4, we
consider the advantages that can be achieved in
implementing the PHB by exploiting semantic web
technologies. In particular, we present the
advantages that can be achieved in using RDF (RDF,
2004) and OWL (OWL, 2006) in developing an
ontology (Davies et al., 2007) for the PHB. Finally,
Section 5 concludes the paper by considering the
drawbacks and advantages of PHBs as well as our
future research.
2 STANDARD PHR AND PATIENT
CENTERED HEALTHCARE
2.1 Standard PHRs
PHRs allow individuals to access and coordinate
their lifelong health information and make
appropriate parts of it available to those that are
authorized by the individual (Puustjärvi and
Puustjärvi, 2009). The commonly accepted goal of a
PHR is to provide a complete and accurate summary
of the health and medical history of a consumer
(Angst et al., 2008). A PHR typically includes
information about medications, allergies,
vaccinations, illnesses, laboratory and other test
results, and surgeries and other procedures.
PHRs can be classified according to the platform
by which they are delivered, and so the distinction
between paper-based, portable-storage based, PC-
based and Internet–based PHRs can be made.
However, in this paper by the acronym PHR we
refer only to Internet-based PHRs.
PHRs have the potential to dramatically change
healthcare in the near future as they enable patients
to become more involved and engaged in their care
and allow other authorized stakeholders to access
information about patients that was previously not
available. The changes effected by PHR systems
could have a significant, positive impact on the
efficiency of healthcare sector and thus resulting
considerable cost savings to the healthcare systems.
However, many barriers exist to widespread PHR
installation, adoption, and use, foremost among them
the lack of the compatibility of the systems within
healthcare sector (Puustjärvi and Puustjärvi, 2008).
In order to avoid the compatibility problems in
importing data to PHRs various standardization
efforts on PHRs have been done. In particular, the
use of the Continuity of Care Record (CCR
standard) of ASTM and HL7’s Continuity of Care
Document (CCD standard) has been proposed for
using in standardizing the structure PHRs. From
technology’s point of view CCR and CCD-standards
represent two different XML schemas designed to
store patient clinical summaries. On the other hand,
both schemas are identical in their scope in the sense
that they contain the same data elements.
PERSONAL HEALTH BOOK - A Novel Tool for Patient Centered Healthcare
387

The sections of the CCR compliant XML-
document include for example patient insurance
information, immunizations, allergies, diagnoses,
procedures and medication list. Each section
contains elements that can represent free text or
structured XML-coded text. The content of each
CCR file is captured from various sources such as
from hospital information system, a clinical
laboratory, from a pharmacy or from the patient him
or herself. In order to know who or what
organization is the source of each element in a CCR
file each data element is time and source stamped.
In order to illustrate CCR compliant documents
let us consider the XML-document of Figure 1.
<ContinityOfCareRecord>
<Patient> <ActorID>AB-12345></ActorID></Patient>
<Medications>
<Medication>
<Source>
<ActorID>Pharmacy of Kaivopuisto</ActorID>
<ActorRole>Pharmacy</ActorRole>
</Source>
<Description>
<Text>One tablet ones a day</Text>
</Description>
<Product>
<ProductName>Valsartan</ProductName>
</Product>
<Strenght>
<Value>50</Value>
<Unit>milligram</Unit>
</Strenght>
<Quantity>
<Value>30</Value>
<Unit>Tabs</Unit>
</Quantity>
</Medication>
</Medications>
</ContinityOfCareRecord>
Figure 1: A CCR compliant XML-document.
Figure 1 represents a CCR file that has a
medication list (element Medications), which is
comprised of one medication (element Medication)
that is source stamped by the Pharmacy of
Kaivopuisto.
The use of XML assures that the data contained
in CCR or CCD documents can be expressed in
multiple media formats (e.g., in HTML that can be
accessed by a browser) that are friendly to both
consumers and providers. However, the problem lies
in that the data included in CCR file is not relevant
for patient’s abilities or understanding. To see this
let us next consider the imaginary scenario behind
the CCR file of Figure 1.
2.2 Motivating Scenario
Assume that patient, named Susan Taylor, having ID
AB-12345, visits a physician for a diagnosis. After
the diagnosis the physician sends (through the
electronic prescription writer) the prescription to an
electronic prescription holding store and gives the
prescription in a paper form to Susan. It includes
two barcodes: the first identifies the address of the
prescription in the holding store, and the second is
the encryption key which allows the pharmacist to
decrypt the prescription.
At the pharmacy Susan gives the prescription to
a pharmacist. The pharmacist scans both barcodes
by the dispensing application, which then loads the
electronic prescription from the prescription holding
store. Then the pharmacist delivers the prescription
into pricing system, which checks whether some of
the drugs could be changed to a cheaper one. The
pricing system notifies that Diovan should be
changed to Valsartan as it is substitutable and
cheaper, and so only Valsartan is repayable. Then
by the permission of Susan the pharmacist replaces
Diovan by Valsartan in Susan’s prescription. Finally
the pharmacist dispenses the drug to Susan and
generates the CCR-file of Figure 1 and sends it into
Susan’s PHR.
Later on at home Susan opens her PHR and
looks at the prescription received from the
physician. She is worried about the change in the
prescription as she does not have Diovan though her
trusted physician prescribed it for her. She hesitates
whether she should contact her physician before
taking her new medicine.
This kind of scenario where a patient is unaware
about the principles of her medication should not
happen. Instead, according to the goals of patient-
centered healthcare all relevant health information
should be delivered to patient and presented
according to patient’s understanding and abilities.
The problem here is that by just storing the
prescription in PHR is not the key point but rather
Susan should be informed about:
• What is the relationship between
Diovan and blood presssure?
• What is the relationship between
Diovan and Valsartan?
• What does generic substitution mean?
In our PHB the key idea is that within each
action that generates an input to a PHB also an
appropriate information entity or entities (or their
links) are also stored in the PHB. With respect to
the previous scenario it means that the physician
HEALTHINF 2011 - International Conference on Health Informatics
388
should have stored two information entities: one
focusing on blood pressure and the other focusing on
Diovan. Further the pharmacist should have stored
two information entities: one focusing on general
substitution and one focusing on Valsartan. We next
present how such additional functions can be
technically performed.
3 TECHNICAL ASPECTS OF THE
PHB
We use the term PHB system of the software
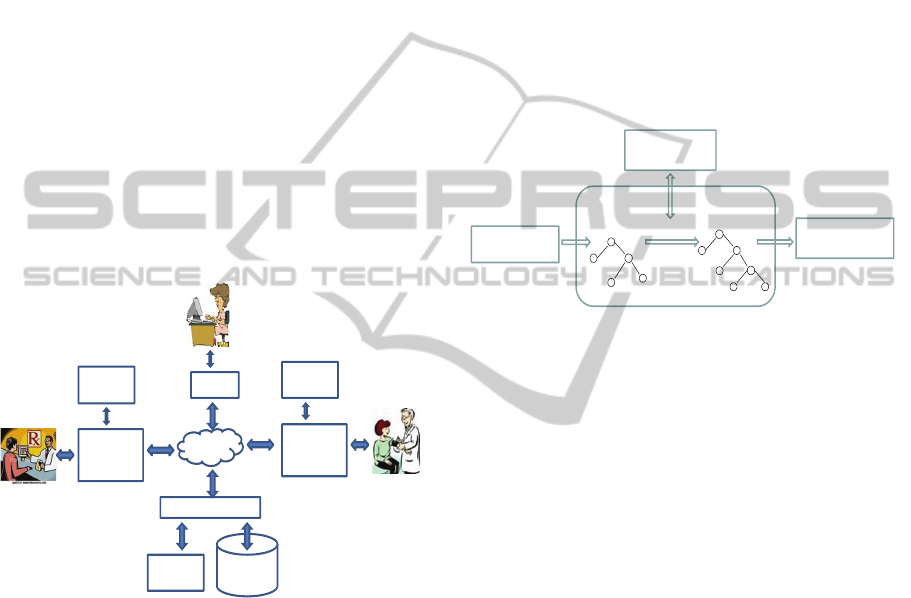
application that manages PHBs. The connections of
PHB system to other components are illustrated in
Figure 2. In the figure, there are only three parties
(patient, pharmacist and physician) that
communicate with the PHB system, but in reality,
similar to PHR systems there may be many more
parties that are authorized by the patient.
Figure 2: The components of the PHB-based healthcare
model.
In the emergence of many new technologies
based on Web services and Semantic Web, there are
many chances for modelling PHB’s content as well
as implementing PHBs and the message exchange
between the communicating parties. Each chance
has its limitations and opportunities.
We have developed two alternative ways for
importing data into PHBs and modelling the content
of the PHBs. However both alternatives are similar
in that they are able receive CCR (or CCD) files
(XML-documents), which are then transformed in
the format that contains links into relevant
information entities. After the transformations the
documents are then inserted in the PHB.
The transformations are carried out through a
stylesheet engine (Daconta et al., 2003) (also called
XSLT engine). It takes an original XML document,
loads into a DOM source tree (Daconta et al., 2008)
and transforms that document with the instructions
given in the style sheet. The instructions use XPath
(XPath, 2008) expressions in referencing to the
source tree and in placing it into the result tree. The
result tree is then formatted, and the resulting
element is returned.
Our used two alternatives are different with
respect to the used stylesheets: one transforms the
document into an XML document and the other into
RDF/XML document. These two alternatives and
the transformation process are illustrated in Figure 3.
Figure 3: Augmenting a document by relevant links by
using a stylesheet engine.
We next consider the limitations and
opportunities of these two alternatives.
3.1 XML-based PHB
In order to illustrate the transformation into an XML
document let us consider the CCR-file presented in
Figure 1. The figure includes Susan Taylor’s
prescription in XML format. As we presented in the
imaginary scenario the final prescription was
developed as a result of generic substitution, i.e.,
Diovan was replace by Valsartan. So, according to
the PHB-based healthcare model the prescription
should be augmented by two links: one link to the
information entity that deals generic substitution,
and the other link to information entity that deals
Valsartan.
In order to produce such an augmentation the
pharmacist activates (through the prescription
management system) the stylesheet engine that
returns the XML document presented in Figure 4.
Note that in this resulted XML-document the link to
Valsartan is included in the element ProductInfo,
and the link to generic substitution is included in the
element GenericSubstitutionInfo.
Prescription
Management
System
Pharmacist
Physician
Patient
Browser
Electronic
Prescription
Writer
Internet
PHB
(datastore)
PHBsystem
Stylesheet
Engine
Stylesheet
Engine
Stylesheet
Engine
XML tree
Transformed
XML tree
Stylesheet Engine
Transformation
Resulting document
in XML or RDF/XML
Stylesheet
(XSLT document)
Original CCR
document in XML
PERSONAL HEALTH BOOK - A Novel Tool for Patient Centered Healthcare
389

<ContinityOfCareRecord>
<Patient> <ActorID>AB-12345></ActorID></Patient>
<Medications>
<Medication>
<Source>
<ActorID>Pharmacy of Kaivopuisto</ActorID>
<ActorRole>Pharmacy</ActorRole>
</Source>
<Description>
<Text>One tablet ones a day</Text>
<GenericSubstitutionInfo>
http://www.../medicalinfo/SubstitutionInfo
</GenericSubstitutionInfo>
</Description>
<Product>
<ProductName>Valsartan</ProductName>
<ProductInfo>
http://www.../medicalinfo/ValsartanInfo
</ProductInfo>
</Product>
<Strenght>
<Value>50</Value>
<Unit>milligram</Unit>
</Strenght>
<Quantity>
<Value>30</Value><Unit>Tabs</Unit>
</Quantity>
</Medication>
</Medications>
</ContinityOfCareRecord>
Figure 4: An XML-coded prescription including links to
relevant information entities.
3.2 Ontology-based PHB
Using the XML-based PHB we can solve the
problems that Susan Taylor encountered in the
scenario presented in Section 2. However, we still
have a problem; namely in retrieving XML data we
cannot use the expression power of the query
languages developed for retrieving data that are
organized according to an ontology. Instead we have
to use query languages that access tree-structured
data such as XPath and XQuery, which expression
power is too limited for our purposes.
In order to illustrate this we will continue our
scenario. Let us assume that Susan Taylor has
stored daily her blood pressure in her PHB as her
medication (Diovan and Valsartan) should decrease
her blood pressure. After using Valsartan a couple of
weeks Susan still suspects whether Valsartan is
equally effective as Diovan. So she would like to
make the following queries:
“What is my average blood pressure during the
time when I have been using Diovan ?” and
“What is my average blood pressure during the
time when I have been using Valsartan ?”
Unfortunately these queries are outside of the
expression power of XPath and XQuery that can be
processed on XML-documents, and so Susan’s
XML-based PHB fails in retrieving this important
information.
In order to allow this kind of data-centric queries
(i.e., queries where data is extracted from various
documents and then integrated according to certain
criteria) on PHBs, we have also developed an
ontology based PHB. Its content is structured
according to an ontology, called PHB-ontology.
We have specified the PHB-ontology by Web
Ontology Language (OWL), and Resource
Description Language (RDF) is used for
representing the actual PHBs, i.e., the instances of
the PHB-ontology.
In developing the PHB-ontology we have
exploited the XML-schema of the CCR-standard. In
transforming its XML Schema to OWL-ontology we
have used on the whole the following rules:
1. The complex elements are transformed to
OWL classes.
2. Simple elements are transformed to OWL
data properties.
3. Element-attribute relationships are
transformed to OWL data properties.
4. The relationships between complex
elements are transformed to class-to-class
relationships (object properties).
However, as the OWL does not support
structured attributes we have not transformed all
complex elements to classes but rather the complex
elements that do not have identification have been
transformed to a set of properties. For example the
following complex element:
<Strenght>
<Value>50</Value>
<Unit>milligram</Unit>
</Strenght>
of the CCR-file of Figure 1 is first transformed into
data properties StrenghtValue and StrenghtUnit, and
then connected to the OWL class Medication. To
illustrate this kind of transformation, a subset of
PHB-ontology is presented in Figure 5. In this
graphical representation ellipses represent classes
and subclasses, and rectangles represent data
properties and object properties.
HEALTHINF 2011 - International Conference on Health Informatics
390

Figure 5: A subset of the PHB-ontology in a graphical
form.
The graphical ontology of Figure 5 is presented
in OWL in Figure 6. Due to the space limits, we
have omitted the specifications of the data properties
such as PatientName and BrandName.
<rdf:RDF
xmlns:rdf=http://www.w3.org/1999/02/22-rdf-syntax-nsl#
xmlns:rdfs=http://www.w3.org/2000/01/rdf-schema#
xmlns:owl=http://www.w3.org/2002/07/owl#>
<owl:Ontology rdf:about=“PHR”/>
<owl:Class rdf:ID=“Patient/”>
<owl:Class rdf:ID=“Medication/”>
<owl:Class rdf:ID=“Source/”>
<owl:Class rdf:ID=“Product/”>
<owl:Class rdf:ID=“LabTest/”>
<owl:Class rdf:ID=“BloodPressureTest”>
<rdfs:subClassOf rdf:resource=“#LabTest”/>
</owl:Class>
<owl:Class rdf:ID=“ColesterolTest”>
<rdfs:subClassOf rdf:resource=“#LabTest”/>
</owl:Class>
<owl:ObjectProperty rdf:ID=“Uses”>
<rdfs:domain rdf:resource=“#Patient”/>
<rdfs:range rdf:resource=“#Medication”/>
</owl:ObjectProperty>
<owl:ObjectProperty rdf:ID=“Contains”>
<rdfs:domain rdf:resource=“#Medication”/>
<rdfs:range rdf:resource=“#Product”/>
</owl:ObjectProperty>
<owl:ObjectProperty rdf:ID=“Originates”>
<rdfs:domain rdf:resource=“#Medication”/>
<rdfs:range rdf:resource=“#Source”/>
</owl:ObjectProperty>
<owl:ObjectProperty rdf:ID=“Performed”>
<rdfs:domain rdf:resource=“#Patient”/>
<rdfs:range rdf:resource=“#LabTest”/>
</owl:ObjectProperty>
.
.
.
</rdf:RDF>
Figure 6: A subset of the PHB-ontology in OWL.
In data storage (knowledge base) the instances of
the PHB-ontology are presented by RDF-elements.
To illustrate this, Susan’s augmented prescription in
RDF/XML format is presented in Figure. 7.
<rdf:RDF
xmlns : rdf=http://www.w3.org/1999/02/22-rdf-syntax-ns#
xmlns : info=http://www.lut.fi/ontologies/PHB-infoentities#
xmlns : po=http://www.lut.fi/ontologies/PHB-ontology#>
<rdf:Description rdf:about=”AB-12345”>
<rdf:type rdf:resource=“&po;Patient”/>
<po : PatientName>Susan Taylor</po:PatientName>
<po:Uses rdf:resource=“&po;Med-07092010”/>
</rdf : Description>
<rdf:Description rdf:about=” Med-07092010”>
<rdf:type rdf:resource=“&po;Medication”/>
<po:Contains rdf:resource=“&po;Valsartan”/>
<po : StrenghtValue rdf:datatype=
”&xsd;integer”>30</po : StrenghtValue>
<po : StrenghtUnit>Tabs</po : StrenghtUnit>
</rdf : Description>
<rdf:Description rdf:about=”Valsartan”>
<rdf:type rdf:resource=“&po;Product”/>
<po:Deals rdf:resource=“&info;ValsartanInfo”/>
</rdf : Description>
< rdf:Description rdf:about=” Pharmacy of Kaivopuisto”>
<rdf:type rdf:resource=“&po;Source/>
<po : ActorRole>Pharmacy</po : ActorRole>
</rdf : Description>
</rdf:RDF>
Figure 7: Augmented prescription in RDF/XML format.
RDF is a language for representing information
about resources in the World Wide Web. It is
intended for situations in which this information
needs to be processed by applications, rather than
being only displayed to people. RDF provides a
common framework for expressing this information,
and so it can be exchanged between applications
without loss of meaning. The ability to exchange
information between different applications means
that the information represented in RDF may be
made available to applications other than those for
which it was originally created.
RDF itself is a data model. Its modeling
primitive is an object-attribute-value triple, which is
called a statement. A description may contain one or
more statements about an object. For example, in
Figure 7, the description concerning “Valsartan”
contains two statements: the first states that its type
is Product in the PHB-ontology, and the second
states that Valsartan is dealed in ValsartanInfo.
Note that OWL ontologies are also represented
by RDF (i.e., they are RDF-elements such as the
OWL ontology of Figure 6), and thus we can query
PHBs by query languages developed for RDF, e.g.,
by SPARQL (SPARQL, 2008), which is
standardized by the RDF Data Access Working
Group (DAWG) of the World Wide Web
Patient
Medication
LabTest
BloodPressureTest
ProductProductName
BrandName
StrenghtUnit
Source
ActorID
ActorRole
ColesterolTest
Value Unit
Value UnitSSN
PatientName
SubclassOf
SubclassOf
Uses
Performed
ContainsStrenghtValue
Originates
MedicationId
InformationEntity
SubclassOfSubclassOf SubclassOf
Disease
Name
RelatesTo
DiseaseIE
Deals
SubclassOf
ProductIE
Deals
ColesterolTestIE
Deals
BloodPressureTestIE
Deals
Date Source
URL
Mother
Father
Hobby
SuffersFrom
PERSONAL HEALTH BOOK - A Novel Tool for Patient Centered Healthcare
391

Consortium, and is considered a component of the
semantic web. On January 2008, SPARQL became
an official W3C Recommendation.
4 CONCLUSIONS
The sophistication of information technology and
communications is changing our society. In the
ongoing healthcare reform, there is an increasing
need to control the cost of medical care. In this
context the significance of patient centered
healthcare care is extensively recognized as it can
help by providing information to the patients, their
families and physicians, not only for illnesses, but
also for prevention and wellness. This, however,
requires that patient’s health information as well as
other relevant medical information is presented in
appropriate format according to individuals
understanding and abilities.
PHRs have the potential to dramatically
contribute to patient centered healthcare as they
enable patient to become more involved and
engaged in their care, and allow other authorized
stakeholders to access information about patient that
has not been previously been available or difficult to
access electronically. Hence, the change that can be
caused by the deployment of PHR systems could
also have a significant impact on the efficiency of
administrative and clinical process in healthcare
sector, and thus will give rise for considerable cost
savings.
However there are many obstacles to the
widespread use of patient centered healthcare. For
example, it is turned out that most patients are not
satisfied with the medical treatment information on
the Web instead they trust on the medical
information that are managed by medical authorities.
A problem however is that how this information can
be targeted for patients.
The analysis of this problem led to the
introduction of the notion of the PHB, which is an
extension of PHR in that all healthcare providers,
who are involved in patient’s healthcare, augment
the PHB by links to relevant information entities.
This PHB based healthcare models presumes that
the information entities used in a therapy are
accessible from the web, i.e., each entity should
have a url (uniform resource locator). This,
however, does not require the creation of new
content as relevant information entities already exist
in digital form, and which can be accessed by the
systems used by the healthcare providers.
An interesting arising question is also that how
we can get patients involved in maintaining and
using a PHB (or PHR in general). Obviously, at least
by providing them by incentives we can increase the
amount of patients that keep PHBs, e.g., by
providing a discount for the patients who keep a
PHB faithfully. Also by showing that using a PHB
will help them to get better medical care would
increase their use.
In our future work we will extend the PHB
system by active elements. By an active element we
refer to an expression or statement that is stored in
PHB, and expect the element to execute at
appropriate times. The times of action might be
when a certain event occurs such as an insertion of a
blood test result. Then depending on the inserted
values an action can be taken such as generating an
email to patient’s personal physician.
REFERENCES
Agarwal R, Angst C. M., 2006. Technology-enabled
transformations in U.S. health care: early findings on
personal health records and individual use, In Galletta
G, Zhang P, (Eds.), Human-Computer Interaction and
Management Information Systems: Applications (Vol.
5). Armonk, NY: M.E. Sharpe, Inc., pp. 357-378.
Angst, C. M., Agarwal, R, Downing, J., 2008. An
empirical examination of the importance of defining
the PHR for research and for practice, Proceedings of
the 41st Annual Hawaii International Conference on
System Sciences.
Bauman, A., Fardy, H., and Harris, H.,“Getting it right;
why bother with patient centred care?,” Medical
Journal of Australia, 179(5), pp. 253-256, 2003.
CCD, 2009. What Is the HL7 Continuity of Care
Document? Available at: http://www.neotool.com/
blog/2007/02/15/what-is-hl7-continuity-of-care-
document/
CCR, 2009. Continuity of Care Record (CCR) Standard.
Available at: http://www.ccrstandard.com/
Daconta, M., Obrst, L.and Smith, K. 2003. The semantic
web. Indianapolis: John Wiley & Sons.
Davies, J., Fensel, D., and Harmelen, F., 2002. Towards
the semantic web: ontology driven knowledge
management. John Wiley & Sons.
Gillespie, R., Florin, D., and Gillam, S., “How is patient-
centred care understood by the clinical, managerial
and lay stakeholders responsible for promoting this
agenda?,”Health Expectations, vol 7 No 2, pp. 142-
148, 2004.
Kaelber, D. Jha, A. Johnston, D. Middleton, B. and Bates,
D., 2008.A Research Agenda for Personal Health
Records (PHRs), J. Am. Med. Inform. Assoc.,
November 1,15(6). pp. 729 - 736.
Little, P., Everitt, H., and Williamson, I., “ Observational
HEALTHINF 2011 - International Conference on Health Informatics
392

study of effect of patient centredness and positive
approach on outcomes of general practice
consultations,” British Medical Journal,” pp. 908-
911, 2001.
Lewis, D, Eysenbach. G., Kukafka, R., Stavri P.Z., and
Jimison, H., 2005. Consumer health informatics:
informing consumers and improving health care. New
York: Springer.
Mettler, M., and Kemper D., Information Therapy:
Health Education One Person at a Time. Health
Promotion Practice 2004 4(3) 214-217.
Michie, S., Miles, J., and Weinman, J., “ Patient-
centredness in chronic illness: what is it and does it
matter?,” Patient Education and Counselling, pp. 197-
206, 2003.
Puustjärvi, J., and Puustjärvi, L., Using semantic web
technologies in visualizing medicinal vocabularies. In
the proc of the IEEE 8th International Conference on
Computer and Information Technology (CIT 2008).
2008.
Puustjärvi, J., and Puustjärvi, L.,The role of medicinal
ontologies in querying and exchanging pharmaceutical
information. International Journal of Electronic
Healthcare, Vol. 5, No.1 pp. 1 – 13. 2009.
Puustjärvi, J., and Puustjärvi, L., Providing Relevant
Health Information to Patient-Centered Healthcare. In
Proc. of the 12th International Conference on e-
Health, Networking Applications and Services (IEEE
HealthCom2010), Pages 215-220.2010.
OWL, 2006. Web OntologyLanguage. Available at:
http://www.w3.org/TR/owl-ref/
RDF, 2004. Resource Description Framework (RDF).
Available at: http://www.w3.org/RDF/
SPARQL, 2008. SPARQL Query Language for RDF.
Available at: http://www.w3.org/TR/rdf-sparql-query/.
Stewart, M., “Towards a global definition of patient
centred care: The patient should be the judge of patient
centred care,” British Medical Journal, 322, pp. 444-
445, 2004.
Trevena, L., Davey H., Barratt A., Butow P., and Caldwell
P., A systematic review on communicating with
patients about evidence. Journal of Evaluation in
Clinical Practice 2006; 12,(1): 13-23.
Thompson, A., “Moving beyond the rhetoric of citizen
involvement: Strategies for enablement,” Eurohealth,
9(4), pp. 5-8, 2004.
Tuil, W. S., Hoopen, A. J., Braat, D. D. M., Vries Robbe,
P.F., and Kremer J. A. M., 2006. Patient-centred care:
using online personal medical records in IVF practice,
Hum. Reprod., November 1, 21(11). pp. 2955 - 2959.
XPath, 2008. XML Path Language (XPath). Available at:
http://www.w3.org/TR/xpath.
PERSONAL HEALTH BOOK - A Novel Tool for Patient Centered Healthcare
393
