
A PROTOCOL FOR DYNAMICALLY MAINTAINING AN
INTEGRATED MEDICAL RECORD DATABASE FROM A SET OF
DIFFERENT MEDICAL RECORD DATABASES
Emilio Hern´andez and Mireya Morales
Department of Computing, Sim´on Bol´ıvar University, Caracas, Venezuela
Keywords:
Health information systems, Medical record databases, Interoperability.
Abstract:
Merging distributed medical record databases into an integrated database is an alternative approach for the
implementation of the unified medical record concept. One of the main advantages of this approach is that
the integrated database could be a backup for medical record databases. Additionally, the integrated database
may be useful for medical research and may help improve the decisions on public policies related to health
care. We propose a protocol for dynamically maintaining an integrated database that is the merge of different
medical record databases, under some limitations related to security and control of the medical record.
1 INTRODUCTION
Hospital Information Systems are usually imple-
mented as client-server or web applications (Morrison
et al., 2010). These applications are suitable as a so-
lution for single administrative domains. A National
Health Service face the problem of fragmentation of
the health-related information among many Hospital
Information Systems. Fragmentation leads to lack of
coordination, information inconsistencies and many
other problems that make it difficult to define appro-
priate public policies. In addition, information inte-
gration is one of the keys for the improvement of the
consumers health care experience.
Interoperability has been pointed out as a key for
the success of a national or regional Health Informa-
tion Service (Brailer, 2005; Walker et al., 2005). The
efforts have mainly been focused on the definition of
information exchange standards (HL7, 2010; ANSI,
2010). It is frequently assumed that cooperating data
sources exchange information horizontally, probably
with the help of data discovery services (Zhang and
W. Xu, 2007). There are also some proposals that
additionally consider the semantic level for data asso-
ciation (Lopez and Blobel, 2009; Hovenga, 2008).
We propose a specific scheme for interoperabil-
ity, based on the integration of databases into a sin-
gle medical record database, with replication of the
information. This approach needs the definition of a
data exchange protocol that ensures some control on
the replicated information, in order to avoid inconsis-
tencies and provide reasonable security. This inter-
operability scheme resembles a memory hierarchy in
which an upper level integrates the databases of sev-
eral institutions. In the context of a country, for exam-
ple, the number of integrated databases could be much
lower than the number of health centre databases (in
fact, there could be a single integrated database). At
this integration level the horizontal interoperability
between large database systems becomes easier be-
cause there is a lower number of databases and fewer
data formats.
Along with the memory hierarchy scheme, we
propose a protocol for dynamically maintaining a
medical record database that is actually the merge of
different medical record databases, under some limi-
tations related to security and control of the medical
record ”ownership”.
In this paper we describe the proposed interop-
erability scheme and the associated synchronization
protocols. Section 2 presents the components of the
interoperability scheme, section 3 describes the pro-
tocols and section 5 shows the conclusions.
2 HEALTH INFORMATION
SYSTEMS AS MEMORY
HIERARCHIES
At the heart of a Health Information System is the
medical record database. In our model, this database
592
Hernández E. and Morales M..
A PROTOCOL FOR DYNAMICALLY MAINTAINING AN INTEGRATED MEDICAL RECORD DATABASE FROM A SET OF DIFFERENT MEDICAL
RECORD DATABASES.
DOI: 10.5220/0003173705920595
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2011), pages 592-595
ISBN: 978-989-8425-34-8
Copyright
c
2011 SCITEPRESS (Science and Technology Publications, Lda.)

is defined as the union of the databases located at the
Local DB Level (Local Database Level). These lo-
cal databases can be deployed, for example, at the
computer departments of large hospitals. The local
databases are integrated in a single database at the
Integrated DB Level (Integrated Database Level) by
providing a copy of each medical record, probably ac-
cording to strict security policies. The database of the
Integrated DB Level could be, in turn, a distributed
database with the possibility of offering a single view.
In this sense the whole system resembles a mem-
ory hierarchy. The main difference with a computer
memory hierarchy would be that the control of the
original version is not at the upper level. Local DB
Servers have the ”ownership” of the medical records,
in such a way that they could even decide whether to
prevent some medical records from being uploaded to
the integrated database.
We define three levels in which synchronization
software must be implemented for moving data up-
wards and backwards in the memory hierarchy. These
levels are:
• Access Level. Basically the access level is com-
posed of the end-user systems that allow medi-
cal staff to interact with the system, as well as
monitoring systems that send patient information
from home or from mobile devices. If the com-
puters at the Access Level can work standalone
during some periods of connectivity failure, data
collected locally must be synchronized later with
the Local DB Level.
• Local DB Level. This level is composed of the
basic data centres where the data are actually
stored. The combination of the Access Level and
Local DB Level basically conforms to a client-
server model with fault tolerance features. Lo-
cal DB Servers may be located within the health
centres, if they have the capacity for administer-
ing a small data centre. The data formats or the
client-server software used by different Local DB
Servers may vary from site to site.
• Integrated DB Level. This level contains, as a
basic unit, a database with the information of sev-
eral Local DB Servers. Local DB Servers must
periodically synchronize their databases with the
Integrated DB Level, using a synchronization pro-
tocol that performs data format transformations if
necessary. Several Integrated DB Servers may in-
teroperate under a secure platform, for instance a
Grid Platform (Foster and Kesselman, 1999), if a
higher degree of integration has to be achieved.
Between the health centres at the Access Level
and the Local DB Level the data will usually flow
through an on-line web application. Between the Lo-
cal DB Level and the Integrated DB Level the data
will flow through synchronization protocols.
We are not defining interoperability protocols be-
tween Local DB Servers. This means that if a patient
must be attended at a health centre far from home,
the assigned Local DB Server must obtain the infor-
mation related to the patient (i.e. the medical record)
from the Integrated DB Level.
The Access Level includes all systems related to
home or mobile monitoring of outpatients. In this
case, the Local DB Level must provide the services
for receiving data from the devices that collect the
monitoring information.
3 THE SYNCHRONIZATION
PROTOCOLS
In this section we describe the protocol for dynami-
cally maintaining the medical record database of the
Integrated DB Level by merging different medical
record databases at the Local DB Level. Such a pro-
tocol needs to be defined and executed under some
limitations related to security and control of the med-
ical record ”ownership”.
In the proposed protocol there are only two al-
lowed operations.
1. Synchronization of a Local DB Server with the
Integrated DB Server.
2. Query of a single medical record to the Integrated
DB from the Local DB Server. This query should
be used only in those cases in which a patient is
attended at a health centre located away from that
in which he/she is registered, for instance, during
an emergency.
3.1 Synchronization Protocol
The database synchronization protocol is inspired by
well known file synchronization protocols. In our
case, the protocol synchronizes records rather than
files.
The synchronization protocol, depicted in Fig-
ure 1, works under the following conditions:
• Patients must be identified according to universal
identity keys. This restriction may prevent the im-
plementation of an Integrated DB Level beyond
the limits of a single country or region.
• The patients must be registered just in one Local
DB Server. Conflicts between different versions
of a patient’s medical record could be solved with
the assistance of authorized users.
A PROTOCOL FOR DYNAMICALLY MAINTAINING AN INTEGRATED MEDICAL RECORD DATABASE FROM
A SET OF DIFFERENT MEDICAL RECORD DATABASES
593
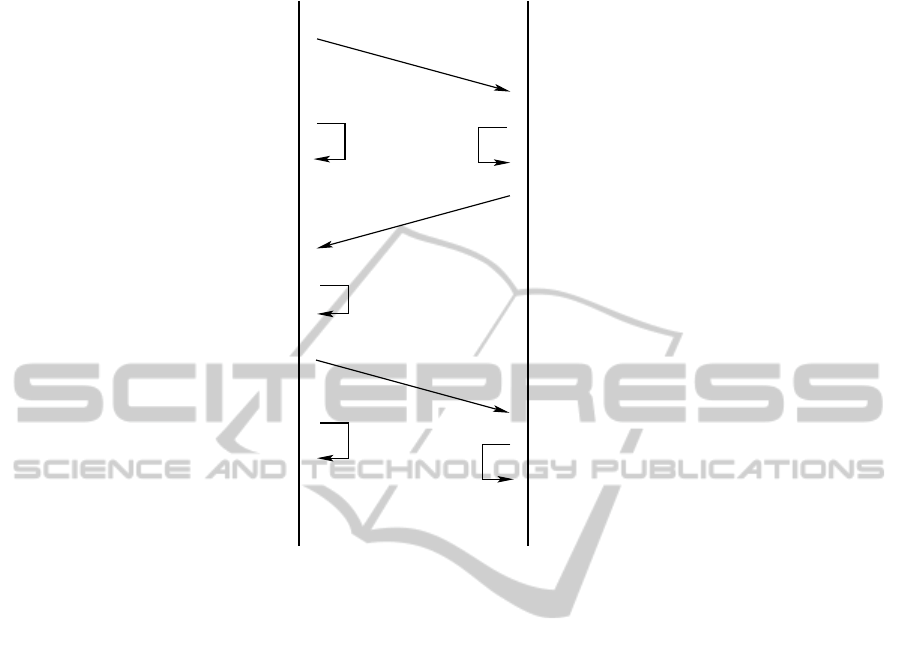
Receive keys of local records
records
changed since last sync
Select local records that Check backup records by received
keys and select those that changed
since last sync
Send the keys of all local
Messages
backup copy was preferred
and conflicting records whose
that do not have conflicts
local copy was preferred
and conflicting records whose
Send changed local records
by the authorized user
by the authorized user
with received records
from Local DB Server
Receive modified records
Ask authorized user
Send backup records that changed
since last sync
Receive backup records
with backup records
Update local database
about conflicts, if any
LOCAL DB SERVER INTEGRATED DB SERVER
Update integrated database
from Integrated DB Server
that do not have conflicts
Figure 1: Synchronization protocol between a Local DB Server and the Integrated DB Server.
• The medical record is stored in the Local DB
Server. The copy of the medical record at the In-
tegrated DB Server is considered a backup.
• Different Local DB Servers may potentially have
different DB formats.
• The Integrated DB records should be designed
with an inclusive criteria, i.e. ideally they must
contain all of the fields that could be present in
any of the Local DB records.
A key consideration for the protocol implementa-
tion is that it needs a database subsystem that keeps
track of the record versions. Every time that a medi-
cal record is modified, an associated version number
field must be increased. Fortunately this requirement
can be easily implemented with the help of triggers,
which most Database Management Systems offer. A
separate table indexed by the medical record key may
contain the version number field and can be added
to both the Local DB Server and the Integrated DB
Server. A trigger must increases the version number
on every record update.
The synchronization protocol is periodically
launched by the Local DB Server. It starts by send-
ing the keys of the patients locally registered to the
Integrated DB Server. Only these records are going
to be synchronized with the Local DB Server. Once
both parts find out which of these medical records
have new versions, they proceed to the information
exchange. If a medical record has new versions in
both sides (probably because the patient was attended
in more than one Health Centre within a short period
of time), an authorized user must decide what infor-
mation should be stored in both the Local DB Server
and the Integrated DB Server.
3.2 Querying the Integrated DB Level
If a patient is attended in the health centre where
he/she is registered, the medical record is available lo-
cally and there is no need to query the Integrated DB
Server. This query is needed if the patient is attended
in a health centre whose Local DB Server is differ-
ent from that in which he/she is registered. This may
happen, for instance, in an emergency far from home.
The query from a Local DB Server to the Integrated
DB must meet the data acces policies defined for the
Health Information System. The medical record is
downloaded and a temporal medical record is cre-
ated in the Local DB while the patient is attended.
This record may be modified in the Local DB. Dur-
ing the next synchronization of this Local DB Server,
HEALTHINF 2011 - International Conference on Health Informatics
594

the modified temporal record is uploaded to the In-
tegrated DB Server and deleted from the Local DB.
Later on, the new version of the medical record will
be downloaded from the Integrated DB to the Local
DB where the patient is registered, keeping a copy at
the Integrated DB Level.
4 IMPLEMENTATION
The synchronization protocol must be implemented
for each Hospital Information Systems, because they
may have different Database Management Systems,
of different database definitions. An analysis at the
semantic level must be carried out in order to define
table and field mappings between the Local DB and
the Integrated DB. The implementation of the syn-
chronization protocol must include the version track-
ing subsystem described in section 3.1. The synchro-
nizer itself follows a client-server model in which
both parts must authenticate each other, for instance
by means of digital certificates.
In practice, the execution of a the synchronization
protocol with several Local DB Servers could unveils
the presence of many medical records for the same pa-
tient, loaded from different health centres. Once the
patients are assigned their Local DB Servers, multiple
medical records associated to them should progres-
sively be removed. However, in principle, the risk of
having duplicate medical records for the same patient
is independent of the interoperability approach.
4.1 Prototype
As a proof of concept, a prototype of a Hospital Infor-
mation System and a Synchronization Tool have been
developed. The Medical Record and Interconsultation
subsystems are tightly coupled. The interconsultation
subsystem does not work at real-time. It is a store-
and-forward telemedicine subsystem that allows aux-
iliary physicians in remote health centres to make in-
terconsultations with other physicians or medical spe-
cialists, usually located in large hospitals. A database
synchronizer is provided, developed with an ad hoc
data exchange protocol. However, other database syn-
chronizers could be developed following a standars
data exchange protocol such as HL7 (HL7, 2010).
5 CONCLUSIONS
In this article we describe an interoperability scheme
for Health Information Systems, based on the inte-
gration of databases into a single database. The data
is actually replicated in the integrated database. This
approach needs the definition of data exchange proto-
cols that ensure the control on the replicated informa-
tion, in order to avoid inconsistencies and provide rea-
sonable security. This interoperability scheme resem-
bles a memory hierarchy in which an upper level inte-
grates the databases of several local database servers.
An integrated database centre located at the top
level of the memory hierarchy will serve as backup
level for local data centres. Additionally, this upper
level will provide the services needed for policy mak-
ing at the health authority level, and will be used for
building data sets for scientific research.
REFERENCES
ANSI (2010). The ANSI ASC X12. http://www.x12.org/,
accessed on July 2010.
Brailer, D. J. (2005). Interoperability: The key to the future
health care system. Health Affairs, 10(1377).
Foster, I. and Kesselman, C. (1999). The Grid: Blueprint
for a New Computing Infrastructure, chapter Compu-
tational Grids, pages 15–51. Morgan Kaufmann Pub-
lishers, Inc.
HL7 (2010). Health Level Seven. http://www.hl7.org/, ac-
cessed on July 2010.
Hovenga, E. (2008). Importance of achieving semantic in-
teroperability for national health information systems.
Texto & Contexto Enfermagem, 17(1):158–167.
Lopez, D. M. and Blobel, B. G. (2009). A development
framework for semantically interoperable health in-
formation systems. International Journal of Medical
Informatics, 78(2):83–103.
Morrison, C., Iosif, A., and Danka, M. (2010). Report
on existing open-source electronic medical records.
Technical Report UCAM-CL-TR-768, University of
Cambridge, Computer Laboratory.
Walker, J., Pan, E., Johnston, D., Adler-Milstein, J., Bates,
D. W., and Middleton, B. (2005). The value of
health care information exchange and interoperability.
Health Affairs, 10(1377).
Zhang, J. and W. Xu, D. E. (2007). System interoperabil-
ity study for healthcare information system with web
services. Journal of Computer Science, 3(7):515–522.
A PROTOCOL FOR DYNAMICALLY MAINTAINING AN INTEGRATED MEDICAL RECORD DATABASE FROM
A SET OF DIFFERENT MEDICAL RECORD DATABASES
595
