
MARKETPLACES FOR HEALTH APPLICATIONS
Assessment of Requirements in Case of the German Public Health System
Sebastian Dünnebeil
1
, Jan Marco Leimeister
2
and Helmut Krcmar
1
1
Department of Informatics, Technische Universität München, München, Germany
2
Department of Economics, Universität Kassel, Kassel, Germany
Keywords: Application store, Healthcare, e-Health, Telemedicine, Public health system, Treatment quality, Treatment
cost, Marketplace, SaaS.
Abstract: Multiple innovations in e-health have the proven potential to improve treatment success, reduce adverse
events and healthcare spending. Despite the promising potential, verified in various studies, the diffusion
speed of healthcare application is very low. A major challenge in healthcare is therefore not only the
research and development for improved treatment, but also the comprehensive and effective diffusion of
selected technologies to caregivers and patients. Hence the paper investigates the theoretical background
influencing the diffusion of innovations. It adopts the concept of application stores, which have shown high
potential as accelerators for extensive distribution of software applications, for the domain of e-health.
Requirements for such a marketplace are derived from the constraints of the public health system. The
involved actors are identified and linked in a high level model.
1 INTRODUCTION
Health systems around the world have seen multiple
innovations in the field of electronic health (e-
health). The benefits of these applications are proven
in many cases; however, the diffusion speed of such
applications is currently very low (European
Comission, 2007). Telemonitoring e.g. has strong
evidence to be beneficial in many aspects of
healthcare. Hospitalization, mortality rate, lack of
work, and the overall treatment costs can be reduced
partially tremendously by telemonitoring, up to 40%
(Helms et al., 2007, Kempf and Schulz, 2008);
however, the software based prevention method is
not commonly used yet. Also medical errors, which
are called adverse event and cause more death than
breast cancer, traffic accidents, and AIDS combined,
can be limited by the usage of e-health application.
Hence utilization of such supporting information
systems (IS) is urgently recommended by the
European Authorities (European Comission, 2007).
Applications managing the accurate discharge of
prescription show significant advantages, compared
to the traditional handling. These are able to
decrease the rate in unadjusted absolute death rate
by 27% for cardio-vascular patients after one year
(Lappé et al., 2004). Considering the fact that wrong
medication in the united States cost $4.4 Billion in
2006 (IOM, 2006) and 37.4% of all adverse events
are caused by wrong medication (Aranaz-Andrés et
al., 2008), the diffusion of such technologies should
be the subject of efforts across the whole society. As
the technology is theoretically available, the benefits
are proven; a method to organize and accelerate the
distribution is an important factor. Therefore the
paper investigates the reasons for slow adoption of
e-health and suggests a model to improve the
situation.
1.1 Diffusion of Innovations
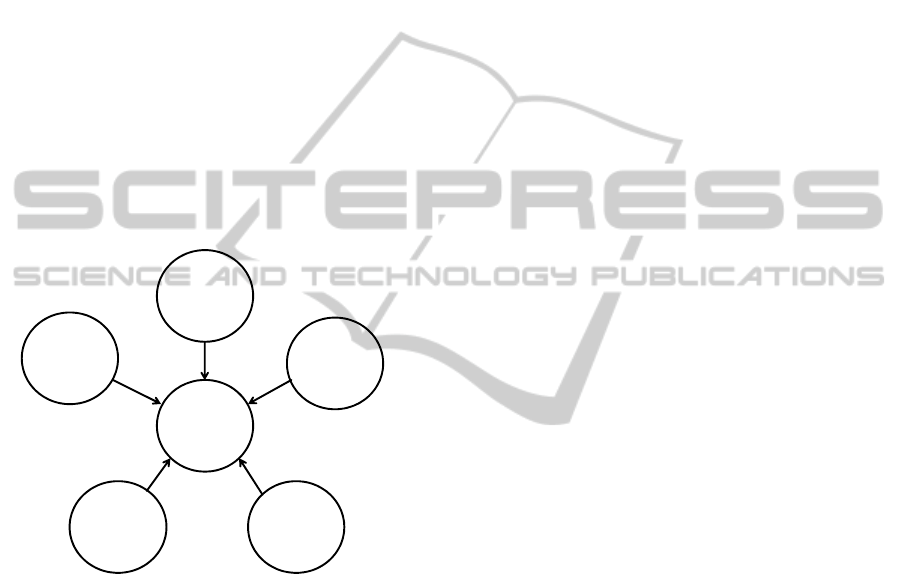
According to Rogers (Rogers, 1995) the diffusion
speed of innovations depends on five factors (figure
1). These factors are assumed to be valid for
healthcare innovations; they are therefore applied to
the area of e-health applications. Goal of this step is
to explain the unsatisfying situation, visible by now.
Relative Advantage: If the new treatment method
can achieve a relative avantage compared to the
current handling, it fosters the underlying
innovation. Main stakeholders involved in the
treatment are caregivers, patients, and the founders
(normally health insurances or tax payers). The
315
Dünnebeil S., Leimeister J. and Krcmar H..
MARKETPLACES FOR HEALTH APPLICATIONS - Assessment of Requirements in Case of the German Public Health System.
DOI: 10.5220/0003171703150322
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2011), pages 315-322
ISBN: 978-989-8425-34-8
Copyright
c
2011 SCITEPRESS (Science and Technology Publications, Lda.)
examples above show that the relative advantage is
obvious, at least in the case of patients and founders,
as treatment success improves and treatment cost
drops. The usage condition must therefore be
changed in a way that caregivers also benefit from
the relative advantage when using e-health
applications. This could be achieved by financial
incentives. Cases where expected efficiency
advantages resulting from the application of health
information technology (IT) are not, at least
partially, distributed to the caregivers are likely to
gain little acceptance within this group. In the case
of the German health card this problem caused a
tremendous cut back in functions offered by the
system, due to the resistance of the caregivers
(Tuffs, 2008). No insentive structures were planned
for this group, the reduction of overall treatment
spendings, resulting from better health care, raised
the fear of lower income for phyiscians without
adequate compensation (Bernnat, 2006).
Figure 1: Diffusion speed of innovations.
Complexity: Innovations must be easy to handle for
the involved actors. Considering the fact that a an
average physician-patient contact only lasts about
seven minutes (Kurt, 2001), complex applications
are difficult to handle for either side. Handling for
the patients must be especially easy, as they have
high variation in cognitive reaction and technical
background. Caregivers genarally do see themselves,
at least partially, responsible for the education and
support of their patients, when they use e-health
services. (Dünnebeil et al., 2010b) This raises a high
scepticism concerning the extra effort caused by the
support of patients and requires a comprehensive
program in order to distribute the education work to
various institutions.
Compatibility: Applications must be integrated into
the application landscape of the software that is
already deployed in the health institutions. The
exchange of data with existing applications is
essential in many cases. Missing data exchange
leads to the usage of multible software systems
during the treatment of one patient. In case of
multimorbidity several treatment processes have to
be combined. Hence software integration should
result in one interface instead of multible. In extreme
cases the divertion into seperated systems can even
cause patient’s death, caused by cognitive overload
of caregivers (Zuehlke et al., 2010). Compatibility
can be partially ensured by interoperability of
distinct IS. Several approaches exist to ensure
syntactic and semantic interoperability (Pedersen
and Hasselbring, 2004). However, the compatibility
is not fully insured for combinations of various
software modules yet.
Triability: Potential users must be able to try e-
health applications before their adoption decision.
The case of the German health card system, which
tried to establish mandatory software usage for e.g.
prescribing, has shown that voluntary usage has
advantages. Several systems should compete in
terms of user friendliness. The chance to try
different applications for the same purpose gives the
possibility to adopt the system which matches the
users’ individual requirements best.
Observability: Little of the advantages of e.g.
telemonitoring or prescription applications are
known to the public by now. If patients can observe
that other patients, who do use e-health applications
personally or who’s caregivers are supported by
such software, receive a better treatment, they will
likely request the services during medical treatment,
too. Same counts for caregivers who can observe
advantages in terms of earnings or quality achieved
by colleagues using e-health applications.
2 APPLICATION STORES
Marketplaces for applications have the potential to
deliver software from various developers distributed
all over the world to users. While mobile phones had
few applications installed in the past, by today a
mobile phone can host any combination of up to
225,000 applications (Holzer and Ondrus, 2009).
The revenue created with the App Store of apple
currently exceeds $ 1 Billion; more than 5 Billon
applications were downloaded and deployed on the
devices of the company so far. Considering the total
sales of the iPhone and the iPod Touch, which
reached 34 Million units by 2009, an average
Diffusion
Speed
Triability
Relative
Advantage
Complexity
Observability Compatibility
HEALTHINF 2011 - International Conference on Health Informatics
316

deployment of about 50 applications on one device
can be derived for the year 2009 (AppleInsider,
2010). This turns a modern Smartphone into a highly
customizable device, which can be adapted to fulfil
the user’s individual requirements. The criteria for
diffusion of innovations, which were discussed
earlier, can be easily observed in the case of the
iPhone and the App Store. The relative advantage
for customers is the availability of a huge number of
functionalities, offered for their device. It can
therewith be customized to a degree far beyond a
standardized product, as the development of
functionalities does not originate in a single
development entity. Also a mass customization, as in
case of the car industry, cannot reach such a
diversification as a huge distributed community of
developers. Financial advantages are possible for
both, developers, who can reach a broad audience
with their software, and for the distributing
company, which can earn a share of the revenue and
sells the pool of functionalities available for their
devices as a competitive advantage. The complexity
was also reduced, as a single installation method
allows the utilization of specialized applications. A
modern Smartphone is no longer a device for a small
group of people with high technical expertise; rather
it is usable for a broad spec of users. Compatibility
with e.g. common mail accounts, wireless access
points and the synchronization with home computers
allow the usage of personal data on various devices
and in several applications. The triability has
increased as the technology is nearly ubiquitously
offered; users can download free evaluation versions
of applications and evaluated them prior to the
adoption decision. Acquaintances and retailers offer
potential adopters the chance to get an inside, before
the individual decision whether to adopt the
technology or not is taken. The advantages of
applications distributed in this way are also
observable for the public by now. Many people use
the applications and advertisement tries to transport
the advantages to a broad target audience.
As e-health innovations can achieve advantages
for patients and reduce the public healthcare
expenses for chronic diseases, health authorities
should be keen pushing the deployment of these
technologies. If the potentials of application stores
for mobile phones can be transferred to the
healthcare sector, a broader distribution might be a
possible result. The paper will therefore investigate
if the concept of marketplaces for applications, as
described for mobile communication, can be
transferred to the healthcare sector. The concept
turns requirements and constraints into a high level
model, which can be implemented afterwards.
3 REQUIREMENTS
IN HEALTHCARE
Medical IS are currently mostly available in fixed
versions with few optional extension modules. Some
Personal Health Records (PHR), as HealthVault of
Microsoft, offer a data pool for patients, which can
be extended and used by additional applications as
heart rate watches or blood pressure monitors
(Microsoft, 2007). The security issues, HealthVault
is not conform to the Health Insurance Portability
and Accountability Act (HIPAA) and the German
privacy protection commissioner discourage patients
from usage (Sunyaev et al., 2010), turn the usage of
patient centred commercial health records into an
unlikely approach to overcome the described
diffusion problem. Especially since caregivers
harshly reject private companies to act as health
application providers and PHR operators (Dünnebeil
et al., 2010b), other methods must be evaluated to
encourage the distribution of e-health innovations.
The healthcare sector is not considered a normal
market. Only less than one third of all services
provided in healthcare are paid by the consumer of
these services directly. Most expenses are covered
by health insurances or authorities, financed by tax
money. Those must not take adoption decisions
based on subjective opinion; they must rather
establish a traceable method to decide whether an
application should be financed. A patient cantered
approach is therefore not sufficient. A method to bill
services to health insurances must be included.
Accordingly the approach used in the mobile phone
market is adopted and extended for healthcare in the
following section. When designing a marketplace for
e-health applications, several conditions have to be
fulfilled. The paper constructs a marketplace for
healthcare applications, considering the
requirements and constraints set in the German
public health system. The model is developed step-
by-step, starting with the software deployment
model, which is currently used for software
distribution in the German public health system to a
model, which includes all necessary aspects covered
in this work. Goal of software development on the
platform is to allow developers of medical software
and telemedicine applications to reach as many users
as possible. The best innovations ought to be used
MARKETPLACES FOR HEALTH APPLICATIONS - Assessment of Requirements in Case of the German Public Health
System
317

widely in healthcare, as they have positive medical
impact.
As an example for an e-health application we
look at an application for monitoring cardiac
insufficiency. A software developer has an
innovative concept for telemonitoring, which he
wants to sell to caregivers in ambulatory care. The
company is currently too small to approach a bigger
number of caregivers directly. Additionally the
caregivers show little interest, since they cannot bill
the telemonitoring to the health insurance. Patients
with a valid diagnosis for this chronic disease are
able record their blood pressure and weight once a
day with the system. The data from the blood
pressure meter and the scale is transferred and
recorded on the server of the software provider. The
data transfer from the devices to the server can be
automated or uploaded manually. Once the
parameters run out of normal range, the physician
receives a notification. The doctor’s medical IS
sends a request the service to see whether some of
the patients he monitors have vital parameters
showing impairment as indication for an infarct.
Action can be taken before the patient calls in
because of the symptoms. This normally saves
valuable time. According to the study the saving for
one patient can be expected to be as high as 6000
Euros in one year (Helms et al., 2007). A part of the
savings should go to the application provider and the
caregiver who performs additional extra work when
using the telemonitoring application. A further share
of the savings can be granted to patients with good
compliance.
3.1 Direct Distribution Model
Traditionally software is developed as a
personalized solution for one customer or released as
a product, which can be sold to multiple users
afterwards. Developers of the software can be either
internal IT departments or self-contained software
companies. The distribution channel mainly leads
from the developer to the user directly, reflects
therefore a 1:1 relation (figure 2). Mostly a sales
force is needed to distribute software this way.
Especially for non consumer products, as health IS
or e-health applications, traditional retailers are not
suitable.
Figure 2: Traditional Software development and
distribution model.
Development of customized software for normal
sized medical institutions is often not possible due to
the size. The average institution in German
ambulatory care counts about 2.1 physicians, with
86 patients visiting the practise per day (Dünnebeil
et al., 2010a). With 289k Euro average annual
revenue (Kassenärztliche Bundesvereinigung, 2008)
the development of a customized solution is hardly
affordable and not cost-effective. Most physicians in
ambulatory care are therefore using standardized
stand alone systems for their treatment support. The
market of German health IS for ambulatory care is
highly fragmented. In 2009 116.895 medical IS were
installed in physicians’ practices. In total more than
200 different systems are deployed in primary care
(KVB, 2009). For these solutions the availability of
functions or modules depends on the developments
of the product owner. The utilization of services is
obviously also coupled with the product life cycle,
as updates delivers new functions. For smaller
companies this approach raises the barrier for market
entry. They depend on the owners of the medical IS
to include and sell the application bundled with their
software. An individual market entry with stand-
alone solutions is difficult, taking into account that
nearly 170,000 physicians are practicing in German
ambulatory care. Small companies can neither
provide a sales force to approach a big number of
physicians, nor can they provide the overall
functionality of a self contained-system.
3.2 Application Platforms for Many
Developers
An alternative to the one-to-one distribution of
software is a marketplace for applications, accessible
to many developers as a service (figure 3). This
approach became hugely famous when Apple
released its application marketplace called “App
Store” for their devices. Apple did not intend to
develop the whole software set deployable on their
embedded devices any longer within their own
company. The devices were opened for developers
around the world to sell or donate their applications
via the application store. The operating system
running on such devices is usually not an open
platform. Installation of additional software is only
possible via the provider’s proprietary internet
platform. All applications are checked on conformity
with the company’s guidelines pervious to their
release, especially concerning compatibility and
content. The services provided by the platform are
financed by a certain share of the retail price, which
is retained by the store provider. The financial
User Developer
HEALTHINF 2011 - International Conference on Health Informatics
318

transactions are, at least in the case of the App Store,
carried out by the provider of the store.
Figure 3: SW-Distribution model via a centralized
provider.
The resulting model is a 1-to-n distribution
model, as all the devices running the applications are
of one kind. This approach can be adopted and
applied for the owners of the medical IS. They can
offer developer platforms to enrich their software
with external content. This concept, similar to the
one provided by apple, is hardly feasible,
considering that 200 different providers offer
platforms in ambulatory care. If a developer wants to
reach all patients, theoretically 200 different
versions have to be provided, which requires a high
administrative and technical effort. The providers of
medical IS would have to agree on a common
extension model, ensuring universal compatibility.
3.3 Application Platforms for Various
User Groups
In case of the German health system a high
fragmentation of target platforms is one constraint
that has to be taken into account as there is currently
no overall extension model. Most health IS in
hospital or practices are deployed on open platforms
as a personal computer (PC) or an application server.
Software which is offered by the provider can be
deployed directly to the target platforms. However
the compatibility with the main medical IS has to be
ensured.
Figure 4: Distribution model with multiple developers and
multiple user groups.
Hence it is important to enable the compatibility
with each platform the application is supposed to run
on. For the resulting n-to-n approach (figure 4) this
can be implemented when a) the application is
adapted to every single target platform b) uses an
adequate virtual machine model, which is available
for each target platform, or c) standards are
employed, which can be used by every target
platform.
Case A will deliver native applications to all
registered user platforms and systems. This will
require the applications to be compiled and adopted
to every target platform supported by the provider.
Similar deployment models can be seen for software
as e.g. browsers, which are available for a whole set
of operating systems (Mozilla, 2010). This is
primarily the operating system. Possibly the
caregivers’ IS must also be considered if the
application needs to be integrated with the main
system on the end user. Without common
communication interfaces, every version has to be
adjusted manually. This model is known for mobile
devices as well. Native software is adapted to each
operating system as the iPhone OS, Android of
Symbian.
Case B will require a virtual machine to run the
source code on the target device. Such software
implementations of computers are available for
multiple platforms and can execute applications
virtually. The Java Virtual Machine (JVM) is widely
known and used. A similar model is feasible for
medical IS when virtual machines are running on all
target platforms. The interface problems can
normally not be overcome, as only standard system
interfaces are implemented in the virtual machine.
Case C: The Provider offers the developers
applications via the standardized access, which is
nearly universally executable by computers. The
TCP/IP Stack can today be used with various
application stacks, as the HTTP or SOAP protocol
stack, on which distributed applications can be built.
Therewith the applications are nearly universally
accessible as internet browsers are broadly
distributed, on personal computers (PC), smart
phones and tablet devices. Software as a Service
(SaaS) is the corresponding software delivery model,
which provides access to business functionalities
remotely (usually over the internet) as a service
(Knorr, 2007). This approach can be integrated with
existing legacy systems (Sun et al., 2007) as medical
IS.
3.4 Application Platforms for Different
Groups of Patients
We suggested some rough methods to approach the
challenge of multiple target platforms and IS. A
User Provider
Developer1
Developern
…
Usergroup n
Provider
Usergroup 1
…
Developer 1
Developern
…
MARKETPLACES FOR HEALTH APPLICATIONS - Assessment of Requirements in Case of the German Public Health
System
319

provider of an e-health marketplace can offer
software with a certain standard or for a virtual
machine to manage the fragmentation issue. The
majority of healthcare spending is public funds.
Those are credited to the caregiver after the
treatment, mostly according to a fixed allowance
catalogue. If the user of e-health applications is a
caregiver, whose treatment is founded by his or her
patient’s health insurance, the software must be able
to deal with the billing modalities of several user
groups. Most insurance differ in terms of benefits
and administration. In Germany each citizen has
mandatory public health insurance. Currently 163
public health insurances are available (GKV, 2010),
which leads to at least 163 different groups of clients
to be handled.
Figure 5: Application Platform with certification entity.
Clients insured by private institutions have
different treatment conditions than clients who are
insured by a public health insurance company. This
can increase the diversity further. Considering the
telemonitoring example for patients with cardiac
insufficiency, the payment to patients, caregivers,
and patients has to be included into the application.
Each health insurance might pay different
allowances to caregivers and patients according to
their regulations. The provider of the application
platform could offer the service of financial
transactions as an additional feature if there is a link
to the health insurance and a payment standard
(figure 5).
3.5 Application Platforms with
Certification Entity
Taking into account that health information contains
very sensitive patient data, a single provider might
not be suitable to control and host the applications in
a self-contained way. The privacy concerns rose for
HealthVault are likely to come up for other
commercial providers that offer e-health
applications, too. Compliance with legal
requirements raises the necessity for a controlling
entity, which is independent from the provider and
separates commercial interests from those of the
public health authorities and the patients.
Applications might collect and interpret personalized
medical data in an illegitimate way. The certification
of a third party can eliminate such threats and
increase the trust in e-health applications, especially
if commercial interests of the controller can be
disqualified (figure 6).
Figure 6: Application Platform with certification entity.
The controlling entity is also suitable to set up
regulations that any medical application has to obey.
A reference model could be the HIPAA guideline or
the German book of social law (Bundesrepublik
Deutschland, 1988), which guarantees that e.g. every
medical data item needs to be authorized by the
owner, before it can be processes by a caregiver.
Also the usage of encryption and digital signature
are regulated in this legal framework.
3.6 Multi User Application Platforms
Customers buying e-health applications have to be
distributed into at least two different groups. The
telemonitoring example indicated that both,
caregivers and patients, need software tools to
ensure a proper monitoring of the patients’ vital
parameters. One group collects the data; the other
group is responsible for the analysis. The application
platform must therefore ensure access for patients
and various groups of caregivers. The resulting
model (figure 7) indicates that the provider has to
offer to at least two access channels.
Figure 7: Multi User-Application Platform Service.
The resulting model presents a comprehensive
approach. It addresses all actors and requirements
necessary to enable software-based cooperation
between patients and caregivers. Legal compliance
and an adequate security standard can be ensured by
a controller entity. Developers of different nature
User Provider
Developer1
Developern
…
Client1
Clientn
…
User Provider
Developer1
Developern
…
Controller
Client 1
Client n
…
UserGroup1
(Patient)
Provider
Developer1
Developern
…
Controller
Client1
(Patient)
Clientn
(Patient)
…
UserGroup2
(Caregiver)
…
UserGroupn
HEALTHINF 2011 - International Conference on Health Informatics
320

can use the provider to offer their services to the
users. Health insurances should be linked to the
provider with a unified billing model. A payment for
every transaction is more likely than a licence model
that requires investment prior to the actual usage of
the service. Each arrow in the model connects actors
involved in the marketplace. All actors but the
provider and the controller are currently very
heterogeneous. A standardization of these links must
therefore be pushed forward to avoid numerous
adoptions to individual characteristics.
4 CONCLUSIONS
Construction of application stores for the healthcare
domain is more complicated than for the mobile
phone market. While mobile phone manufactures
can rely on a unified target platform, the market for
health IS is highly fragmented. Not only the
diversity of end-user systems has to be targeted in an
appropriate manner, but also security standards, the
challenge of interoperability and the ability to bill
services to multiple health insurances or authorities
that operate with different treatment standards. A set
of standards is essential to unify the system and
organization landscape. Otherwise it is unlikely to
achieve a workable platform, allowing more players
to build up the market and pushing medical
innovations into practise. International marketplaces
are difficult to implement, as the health systems
differ enormously around the globe. Already the
number of requirements in the German public health
system is huge. Theoretically 200 primary care
systems are deployed; these have to interact with
value added applications. Each application must be
able to determine the treatment standard for at least
163 health insurances, which can result in very high
complexity. Frequent changes in the legal
regulations raise further barriers for a stable and
sustainable operation of an ecosystem for e-health
applications.
A marketplace for healthcare applications is
certainly desirable. A standardized platform would
ease the market access for more players and
accelerate the diffusion of the innovations seen in
the domain of e-health. Self-contained development
of e-health is very difficult by today, as many
requirements have to be converged to be fully
compliant with national security and administrative
standards. Authorities must set up adequate
standards to enable software development for the
healthcare market that is detached from the
regulations and focuses on the medical and technical
innovations, which are the core competence of the
developers. Chapter 3.3 has indicated how the
problems of platform diversity can be overcome in
software deployment. Health insurances will have to
develop similar methods to determine how e-health
applications can be included into the regular billing
model for healthcare services. A financial model
focused only on the direct payment of patients is
unlikely to be successful. Effectiveness of an
application can often not be judged by the patients,
an inclusion of caregivers seems therefore
inevitable. Hence a proper incentive structure for
this group is important. Health authorities can use
the results of the studies to judge the effectiveness of
e-health applications and include them as allowable
services within a regular time cycle if they perform
well. The paper worked out the actors involved in a
potential marketplace and described important
connections between them. The resulting model is a
high level framework of a comprehensive platform
for application distribution. A more detailed analysis
of the technical and organizational requirements
should be subject of further research.
REFERENCES
Appleinsider (2010) Apple Says App Store Has Made
Developers Over $1 Billion.
Aranaz-Andrés, J. M., Aibar-Remón, C. & Vitaller-
Murillo, J. (2008) Incidence Of Adverse Events
Related To Health Care In Spain: Results Of The
Spanish National Study Of Adverse Events. Journal
Of Epidemiology And Community Health, 62:, 1022-
1029.
Bernnat, R. (2006) Kosten-Nutzen-Analyse Der
Einrichtung Einer Telematik-Infrastruktur Im
Deutschen Gesundheitswesen. Booz Allen Hamilton
Gmbh.
Bundesrepublik Deutschland (1988) Sozialgesetzbuch
(Sgb) Fünftes Buch, Gesetzliche
Krankenversicherung.
Dünnebeil, S., Sunyaev, A., Blohm, I., Leimeister, J. &
Krcmar, H. (2010a) Do German Physicians Want
Electronic Health Services? A Characterization Of
Potential Adopters And Rejectors In German
Ambulatory Care. Third International Conference On
Health Informatics (Healthinf 2010). Valencia.
Dünnebeil, S., Sunyaev, A., Leimeister, J. M. & Krcmar,
H. (2010b) Strategies For Development And Adoption
Of Ehr In German Ambulatory Care. 4th International
Conference On Pervasive Computing Technologies
For Healthcare (Pervasivehealth). Munich, Ieee.
European Comission (2007) Europäischeunion (2007) -
Ehealth For Safety Report. In Communities, O. F. O.
P. O. T. E. (Ed.). Luxembourg.
MARKETPLACES FOR HEALTH APPLICATIONS - Assessment of Requirements in Case of the German Public Health
System
321

Gkv (2010) Alle Gesetzlichen Krankenkassen. In National
Association Of Statutory Health Insurance Physicians
(Ed.).
Helms, T., Pelleter, J. & Ronneberger, D. (2007)
Telemedizinische Betreuung Chronisch
Herzinsuffizienter Patienten Am Beispiel Des
Telemedizinischen Patientenbetreuungs- Und -
Schulungsprogramms „Telemedizin Fürs Herz“. Herz,
32, 623-629.
Holzer, A. & Ondrus, J. (2009) Trends In Mobile
Application Development. Mobile Wireless
Middleware, Operating Systems, And Applications -
Workshops.
Iom (2006) Identifying And Preventing Medication Errors
- Institute Of Medicine,. In Institute Of Medicine Of
The National Academies (Ed.). Washington D.C., The
National Academic Press.
Kassenärztliche Bundesvereinigung (2008) Grunddaten
Zur Vertragsärztlichen Versorgung In Deutschland.
Berlin.
Kempf, K. & Schulz, C. (2008) Telemedizin Bei Diabetes:
Höhere Therapiezufriedenheit, Verbesserte
Stoffwechselparameter. Diabetivar Studie Monika
Dienstle, Wdgz.
Knorr, E. (2007) Software As A Service: The Next Big
Thing.
Kurt, T. (2001) Großbritannien: Ärzte Enttäuscht Und
Desillusioniert. Deutsches Ärzteblatt, 98.
Kvb (2009) Installationsstatistik - Systeme. In
Bundesvereinigung, K. (Ed.). Berlin.
Lappé, J. M., Muhlestein, J. B. & Lappé, D. L. (2004)
Improvements In 1-Year Cardiovascular Clinical
Outcomes Associated With A Hospital-Based
Discharge Medication Program. Annals Of Internal
Medicine, 141, 446-453.
Microsoft (2007) Microsoft Healthvault - Archtiecture
Overview. Microsoft Corporation.
Mozilla (2010) Download A Firefox Version That Speaks
Your Language., The Mozilla Project.
Pedersen, S. & Hasselbring, W. (2004) Interoperabilität
Für Informationssysteme Im Gesundheitswesen Auf
Basis Medizinischer Standards. Informatik -
Forschung Und Entwicklung, 18, 174-188.
Rogers, E. M. (1995) Diffusion Of Innovations, New
York, Ny [U. A.], Free Press.
Sun, W., Zhang, W., Chen, S., Zhang, X. & Liang, H.
(2007) Software As A Service: An Integration
Perspective. In 4749, L. (Ed.) Icsoc 2007. Berlin
Heidelberg, Springer-Verlag 2007.
Sunyaev, A., Chornyi, D., Mauro, C. & Krcmar, H. (2010)
Evaluation Framework For Personal Health Records:
Microsoft Healthvault Vs. Google Health.
Proceedings Of The Hawaii International Conference
On System Sciences (Hicss 43). Kauai, Hawaii.
Tuffs, A. (2008) Germany Plans To Introduce Electronic
Health Card Bmj.Com Medical Publication Of The
Year.
Zuehlke, D., Meixner, G. & Klein, U. (2010) Smart
Medical Software Systems For Dummies? The Case
For A User-Centered Systems Design. Third
International Conference On Health Informatics
(Healthinf 2010). Valencia.
HEALTHINF 2011 - International Conference on Health Informatics
322
