
HEALTHCARE IS INTEROPERABILITY
Challenges and Solutions
Vasiliki Mantzana
1
, Konstantinos Koumaditis
1
and Marinos Themistocleous
1,2
1
University of Piraeus, Department of Digital Systems, 150 Androutsou Street, Piraeus, 18534, Greece
2
University of Coimbra, CISUC, Coimbra, Portugal
Keywords: Healthcare information systems, Healthcare organisations, Challenges, Solutions.
Abstract: Healthcare systems seek to provide services of high quality and profound safety through Healthcare
Information Systems (HIS). Despite the potential benefits of HIS and the significant efforts that have been
made, it has been reported that healthcare systems have a low success rate. It has been reported that the lack
of interoperability still affects the services provided to patients and citizens. In this paper we (a) propose a
novel healthcare processes and services classification, (b) present the HIS challenges and (c) suggest a
solution based on Service Oriented Architecture (SOA), which can increase the interoperability among
systems and hence the quality of provided healthcare services.
1 INTRODUCTION
Improving patients’ safety implies a complex
system-wide effort, which involves all stakeholders
and includes a broad range of actions, such as
paying attention to medication errors, which are the
cause of almost half of all preventable adverse
events and optimizing the use of new technologies.
Nowadays, the development of Healthcare
Information Systems (HIS) that will result in
enhanced services and will save and improve human
lives is the main priority for the healthcare sector
worldwide. In support of this, the economic stimulus
bill signed by the USA Congress included about $19
billion promotes the use of healthcare information
technology, including Electronic Prescribing
(ePrescribing), which can help prevent medication
errors from sloppy hand writing and harmful drug
interactions.
Information Technology (IT) applications such
as Internet-based telemedicine, personal health
records, asynchronous healthcare communication
systems, and picture archiving communication
systems have been applied in healthcare to improve
the capabilities of physicians and clinical staff and
provided increased services to patients, caregivers,
and citizens in general. It appears that HIS play an
increasingly crucial role in the healthcare sector
advancement, by providing an infrastructure to
integrate people, processes and technologies.
In this paper, the authors analyse and propose a
novel classification of healthcare processes and
services, present the HIS challenges and finally
suggest a solution based on Service Oriented
Architecture.
2 HEALTHCARE INFORMATION
SYSTEMS
HIS have been defined as computerized systems
designed to facilitate the management and operation
of all technical (biomedical) and administrative data
for the entire healthcare system, for a number of its
functional units, for a single healthcare institution, or
even for an institutional department or unit
(Rodrigues et al., 1999). HIS are a key enabler, as
they have the potential to improve healthcare
services, by providing rapid and widespread access
to information at the point of care. A plethora of IS,
ranging from order entry and administrative HIS to
laboratory and operation theatre HIS, have been
implemented in the healthcare sector. In shedding
some light on the underlined services that exist in
healthcare organizations, we reviewed the normative
on HIS classification. Based on the processes that
HIS support, Mantzana (Mantzana, 2006)
categorized them into: (a) clinical, (b) non-clinical,
(c) pharmaceutical and (d) laboratory. The authors
559
Mantzana V., Koumaditis K. and Themistocleous M..
HEALTHCARE IS INTEROPERABILITY - Challenges and Solutions.
DOI: 10.5220/0003164505590562
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2011), pages 559-562
ISBN: 978-989-8425-34-8
Copyright
c
2011 SCITEPRESS (Science and Technology Publications, Lda.)
adopt this classification and extend it, by proposing
that the patient record category should be added, as
it refers to medical records that can be maintained by
the citizen or the health professional. This category
can be further broken down into services (a)
Electronic Patient Records Systems (EPR), which
are detailed records of encounters between patients
and their healthcare providers and (b) Electronic
Personal Health Records (ePHR) that are citizen
self-maintained health and healthcare records
(Gaunt, 2009). For each service category, we
identify and describe related Information Systems,
as this is illustrated in Table 1.
Table 1: Healthcare processes and services.
P
roc Service Ref
Clinical
Clinical
Provides electronic charting and
documentation to flow sheets, forms,
notes, work lists, care plans, etc.
(Manjoney,
2004)
Telemedicine
Delivery of healthcare services and
information exchange across
distance.
(Wootton,
2006)
Pharmaceutical
Pharmacy
Keep records about drugs’ ordering,
stocking and distribution
(Anderson P.,
2009)
ePrescribing
Support medicines orders,
administration, use and supply.
(NHS CFH,
2009)
Laboratory
Laboratory
Manage laboratory information, flag
abnormal values or provide possible
explanations for those abnormalities.
(Pantanowitz,
2007)
Non- Clinical
Support
HRM services manage information
about personnel and management
(Kabene, 2006)
CPOE services allow physicians to
enter and send orders.
(Metzger,
2010)
e-Learning increases the
opportunities to learning and
research.
(Land Lesley
Pek Wee,
2007)
Administrative
CRM services are built upon the HIS
as to integrate information generated
from medical acts to sustain the
relationship between hospitals and
customer.
(Hung, 2010)
Financial and accounting
Financial and accounting transactions
with patients, employees etc
(Mantzana,
2006)
Patient
Recor
d
Electronic Patient Records (EPR)
Detailed healthcare records
(Gaunt, 2009)
Electronic Personal Health
Records
Citizen self-maintained records.
(Gaunt, 2009)
The countless amount of hours and money spent
on HIS and services advancement aim at the
healthcare sector modernization and the
enhancement of services provided to citizens and
patients. However, these efforts have resulted in HIS
that have evolved in a haphazard and fragmented
way, and include data in crude formats without any
attempt to synthesize or analyze them, as required by
proper day-to-day management (Mantzana, 2006).
The need to provide an interoperable environment
has become imperative, as the non-integrated nature
of the healthcare systems is strongly associated
among others with the medical errors that occur. For
instance: (a) hard copy films are constantly
lost/unavailable and (b) information needed for
diagnosing is often missing (Cowan, 2004). Thus, as
the information needed is not available on time,
errors usually occur in prescribing, administering
and dispensing drugs services to patients.
3 HIS CHALLENGES
Despite the potential benefits of HIS, it has been
reported that healthcare systems have a low success
rate. In UK, hundreds of millions of pounds and
countless hours of peoples’ time have been spent on
Information Systems implementations. However, the
quality of the healthcare systems suffers as a result
of medical errors, clinical employees’ resistance to
change and fragmented care (Leape et al., 1995).
Medical errors are the failure of a planned action to
be completed as intended (error of execution) or the
use of a wrong plan (including failure to use a plan)
to achieve an aim (error of planning). Several types
of medical errors, such as failure to the
administration of treatment, error to employ
indicated tests, and avoidable delays in treatment
have been reported. The Institute of Medicine (IOM)
of USA determined medical errors as a problem of
big magnitude reporting that the number of
Americans that die each year from medical mistakes
to resume to 98,000 approximately (Kohn et al.,
2000).
Although the aforementioned findings date back
a decade the problem is not eliminated. The medical
error rate used to calculate the IOM’s national
estimate has also been supported by most recent
studies in Canada, Australia, and other developed
countries. Based on the current state of knowledge
of medical harm, it has been estimated that 5% of
hospital admissions experience some type of adverse
error, 30% of which cause consequential harm
(Wachter, 2008). This implies that more than half-a-
HEALTHINF 2011 - International Conference on Health Informatics
560
million people in the U.S. were affected by
preventable medical errors last year. The countless
amount of hours and money spent on HIS and
services advancement aim at the healthcare sector
modernization and the enhancement of services
provided to citizens and patients. However, these
efforts have resulted in HIS that have evolved in a
haphazard and fragmented way, and include data in
crude formats without any attempt to synthesize or
analyze them, as required by proper day-to-day
management (Mantzana, 2006). The need to provide
an interoperable environment has become
imperative, as the non-integrated nature of the
healthcare systems is strongly associated among
others with the medical errors that occur. For
instance: (a) hard copy films are constantly
lost/unavailable and (b) information needed for
diagnosing is often missing (Cowan, 2004). Thus, as
the information needed is not available on time,
errors usually occur in prescribing, administering
and dispensing drugs services to patients.
4 HIS SOLUTION
Interoperability is becoming a central issue in the
healthcare agenda and researchers and vendors are
focusing on ways to address it. According to IEEE,
interoperability is the ability of two or more systems
that is used to exchange information and to use this
information that has been exchanged (IEEE, 1990).
In the field of healthcare interoperability means that
the ability to communicate and exchange data
accurately, effectively, securely and consistently
with different information technology systems,
software applications, and networks in various
settings and exchange data such that clinical or
operational purpose and meaning of the data are
preserved and unaltered (Patricia and Noam, 2007).
Healthcare interoperability is linked with a variety of
both technical and organizational issues such as the
diversity of applications and systems across
departments and the different attitudes and
perceptions between stakeholders. Moreover, even
thought healthcare organizations invest in
integration technologies, in many cases perform
point-to-point integration between solutions adding
to the lack of interoperability (Jay, 2009). The
different aspects of interoperability are addressed by
various initiatives. The aim of these initiatives is not
only to support data/information exchange, but also
to include meaning in them (Lopez, 2009). These
peculiarities of HIS make SOA an adequate
candidate to solve the problem. Despite the
significant benefits that SOA has provided to other
sectors, healthcare systems remain laggards, thus,
leaving scope for timeliness and novel research.
SOA provides a framework for an infrastructure
to facilitate the interactions and communications
between services (Papazoglou M. , 2007a). SOAs
are more of a paradigm, or a style of design that
concludes to architecture. In other words, SOA is a
way of thinking about building software than a
software development technique (Boersma, 2005).
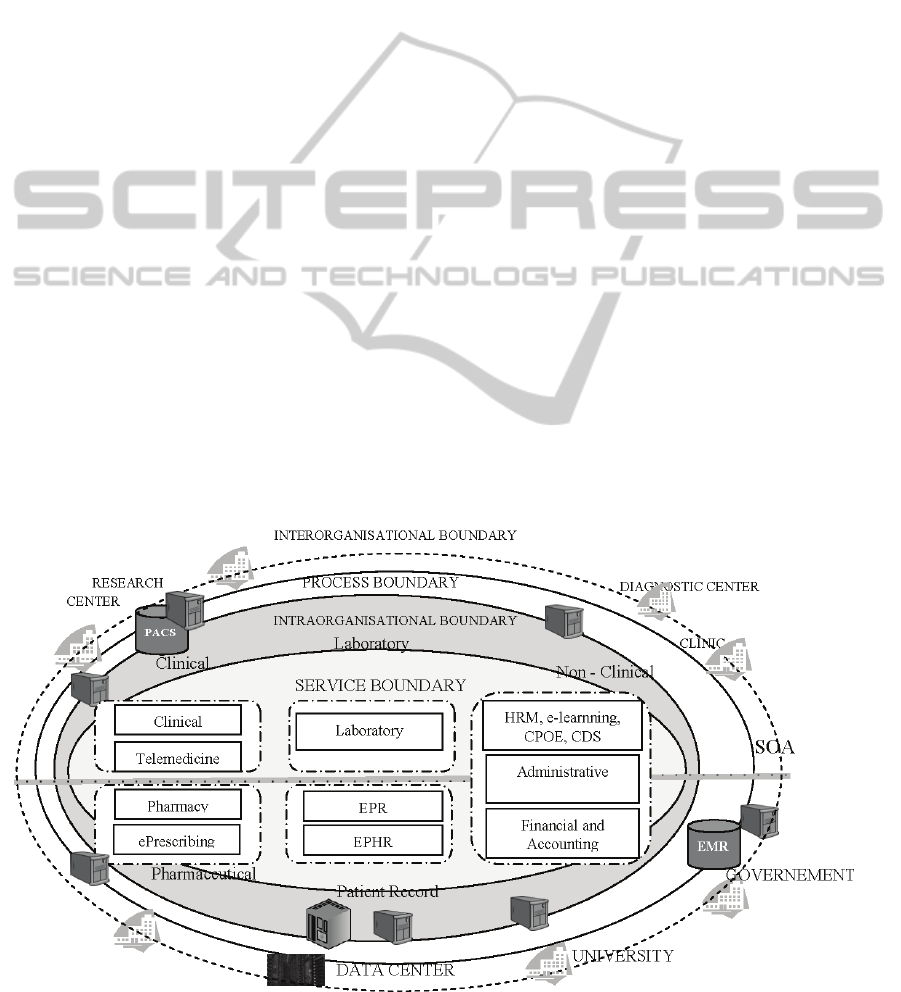
Figure 1: Proposed solution for healthcare systems interoperability.
HEALTHCARE IS INTEROPERABILITY - Challenges and Solutions
561

As SOA is being adopted by the healthcare
industry, the collections of processes that each
consists of specific services will be available for use,
such as pharmaceuticals, labs and patients as seen in
Figure 1. In SOA services aid integration of
applications that were not written with the intent to
be easily integrated, as is the case in most HIS
environments. In more detail, service-based
applications are developed as independent sets of
interacting services offering well-defined interfaces
to their potential users (Papazoglou M. ). This is
achieved by employing loosely coupled distributed
applications between transacting partners and it does
not involve fixed agreements before the use of an
offered service is permitted. Thus, adding to the
flexibility that is required in an interoperable HIS
environment. Since the location of a system
providing services is transparent, these acquired
services may be hosted outside the organization,
thus increasing the integration between systems.
5 CONCLUSIONS
Despite the amount of hours and money spent on IS
implementations and the technological advancement,
healthcare systems still face several challenges.
Problems, with great magnitude such as medical
errors to less substantial as redundant processing and
data are still a part of everyday processing.
Eliminate medical errors and enhancing the quality
of services provided to users in a cost effective way
is a challenge that IT developers are facing. The
answer can be true interoperability through SOA.
SOA can provide true interoperability and enhance
the quality of healthcare services provided, as it
allows system capabilities to be selected and
packaged as services that are better focused and
available across the entire organization.
REFERENCES
Anderson P., M. S., Bourne P. (2009). Pharmacy
Informatics CRC Press.
Boersma, K., Kingma S. (2005). Business Process
Management Journal, 11, 123-136.
Cowan, J. (2004) Clinical Governance: An International
Journal of Critical Care, 9, 132-135.
Gaunt, N. (2009). In Integrating Healthcare With
Information and Communications Technology(Ed,
Finnegan, D.) Radcliffe Publishing, pp. 274.
Hung, S., Hung, W., Tsai, C., Jiang, S. (2010). Decision
Support Systems, 48, 592-603.
IEEE (1990). IEEE (Institute of Electrical and Electronics
Engineers).
Jay, B., Steve, Leski, Brian, Nicks, Traian, Tirzaman
(2009). In Proceeding of the 24th ACM SIGPLAN
conference companion on Object oriented
programming systems languages and
applicationsACM, Orlando, Florida, USA.
Kabene, S., Orchard, C., Howard, J.,Soriano, M., Leduc,
R. (2006). Human Resources for Health, 4, 20.
Kohn, L., Corrigan, J. M. and Donaldson, M. S. (2000). To
err is human: building a safer health system, National
Academy Press, Washington, D.C.
Land Lesley Pek Wee, R. P., Watson Eilean, (2007). In
Pacific Asia Conference on Information SystemsAIS,
Auckland New Zealand 4th- 6th July 2007,.
Leape, L., Bates, W. and Cullen, J. (1995). Journal of
American Medical Association, 274, 35–43.
Lopez, D. M., Blobel, B. G. (2009). International Journal
of Medical Informatics, 78, 83-103.
Manjoney, R. (2004). Journal of Critical Care, 19, 215-
220.
Mantzana, V. (2006). In School of Information Systems,
Computing and Mathematics Brunel University,
London.
Metzger, J., Welebob, E.,Bates, D., Lipsitz, S.,Classen, D.,
(2010). Health Affairs, 29, 655-663.
NHS CFH (2009). In Report commissioned by NHS
Connecting for Health(Ed, NHS).
Pantanowitz, L., Henricks, W., Beckwith, B. (2007).
Clinics in Laboratory Medicine, 27, 823-843.
Papazoglou M. , v. d. H. W. (2007a). The VLDB Journal
16, 389-415.
Papazoglou M., v. d. H. W. (2007b). The VLDB Journal,
16, 389-415.
Patricia, G. and Noam, A. (2007). Health Level Seven,
EHR Interoperability Work Group.
Rodrigues, R. J., Gattini, G. and Aalmeida, G. (1999).
Setting up Healthcare Services Information Systems: A
Guide for Requirement Analysis, Application
Specification, and Procurement., Washington, USA.
Wachter, R. (2008). Understanding Patient Safety,
McGraw-Hill Professional, New York.
Wootton, R. (2006). Introduction to Telemedicine,
Rittenhouse Book Distributors.
HEALTHINF 2011 - International Conference on Health Informatics
562
