
USE OF MOBILE TECHNOLOGY TO SUPPORT PROVISION
OF COMMUNITY-BASED MATERNAL AND NEONATAL CARE
IN DEVELOPING COUNTRIES
Marlen Stacey Chawani and Caroline Ngoma
Department of Informatics, University of Oslo, P.O. Box 1080 Blindern, N-0316 Oslo, Norway
Keywords: Community-based maternal and neonatal care, Community health workers, Mobile technology, Electronic
health records, Developing countries, Rural areas, Malawi.
Abstract: The health systems in many developing countries in Africa are facing critical shortages in nursing and
midwifery health professionals and the situation is worse in the rural areas resulting in poor maternal and
neonatal health outcomes. One of the interventions to address this challenge has been the use of Community
Health Workers to supplement the provision of maternal and neonatal healthcare services within their
communities. The international community is advocating for the use of Mobile technology in supporting
various health service areas including community-based healthcare. This paper presents findings of a
research on the information and communication needs of Community Health Workers in the provision
Community -Based Maternal and Neonatal care in the rural areas of a developing country, Malawi, and it
examines the potential use for adopting mobile technologies in such a setting to meet their needs.
1 INTRODUCTION
Developing countries in Africa are struggling to
make progress towards the achievement of health-
related Millennium Development Goals (MDGs)s
particularly MDG 4 and 5 which are aimed at
reducing child and maternal mortality (UNICEF,
2008). One of the challenges causing this is the
acute shortage of nursing and midwifery health
professionals which is particularly severe in rural
areas due to poor infrastructure and working
conditions (SavetheChildren, 2010). In order to
address this challenge, the international community
recommends governments to scale up human
resources for health including paid community
health workers (MDGAfricaSteeringGroup, 2008).
Thus, interventions are being implemented that
involve Community Health Workers (CHWs) in the
provision of Maternal and Neonatal Healthcare
services at the community level; and countries such
as Pakistan have already demonstrated the positive
impact such interventions can make on improving
health status of the community (GHWA, 2008).
The use of mobile technology to support various
health services as advocated by the international
community can be adapted for community/home-
based healthcare and (Illuyemi and Briggs, 2010)
indicate that supporting Community Health Workers
with mobile information and telecommunication
technologys should be considered a top priority
within the e-health agendas of developing countries.
Many studies on mobile-health (m-health)
applications implemented in developing countries
have reported their use to support HIV/AIDs and
Child health services (Kinkade and Verclas, 2008;
Manda, 2009; UNICEF, 2009; Vital Wave
Consulting, 2009). However, limited literature exists
on the application and use of such technologies to
support Maternal and Neonatal Healthcare even
though this is a high priority health area in
developing countries. Therefore, this study was
conducted to investigate the provision of
Community-based Maternal and Neonatal healthcare
services in a developing country, Malawi, with the
aim of exploring the potential of using mobile
technology to support service delivery. In particular,
the research had four objectives:
1. To investigate the duties and activities of
Community Health Workers (CHWs) in relation to
maternal and neonatal health care.
2. Identify the information and communication
needs of these CHWs in their work
260
Chawani M. and Ngoma C..
USE OF MOBILE TECHNOLOGY TO SUPPORT PROVISION OF COMMUNITY-BASED MATERNAL AND NEONATAL CARE IN DEVELOPING
COUNTRIES .
DOI: 10.5220/0003157902600267
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2011), pages 260-267
ISBN: 978-989-8425-34-8
Copyright
c
2011 SCITEPRESS (Science and Technology Publications, Lda.)

3. Identify the areas in which mobile health
applications can be used to support their needs.
4. Define the design for a mobile-based maternal
and neonatal health application.
Therefore, this paper presents the current activities
of CHWs in the provision of maternal and neonatal
health care at community level in Malawi and their
associated information and communication needs. It
further discusses the potential of using mobile
technology to support the CHWs.
The study is part of an ongoing research on the
use of ICT to support Maternal and Child Health
service whose overall objective is to identify
strategies, through action research, for designing and
implementing ICT-based information systems for
Maternal Health Care services in rural settings of
developing countries.
2 RESEARCH CONTEXT - THE
MALAWI HEALTH SYSTEM
This study was conducted in Malawi where the
majority of the population (85%) is located in rural
areas (NSO, 2008) .
Healthcare services are mainly provided by the
Ministry of Health and there are three levels of
service provision in the health system: the primary
level comprising of health centres, health posts,
dispensaries, and rural hospitals; the second level is
made up of district hospitals; and the tertiary level
consists of the central hospitals and one private
hospital with specialist services (ibid.). The health
centre is the most easily accessible health facility
and thus, it is where most women go to seek
maternal health care. At this level basic maternal and
child health services such as antenatal care, delivery
(for normal cases), postnatal care, child
immunisation, and family planning are provided and
these services are provided by various groups of
health professionals such as nurses, midwives,
medical assistants and clinical officers (MoH,
2007;Sharan et al., 2009). The hospitals provide
more comprehensive obstetric care therefore women
observed with obstetric complications at health
centres are referred to hospitals (ibid.)
The country is reported to have one of the
highest maternal mortality ratios globally as it
almost doubled between 1992 and 2000 from 620 to
1120 deaths per 100,000 live births (Sharan et al.,
2009). Poor access and utilisation of services is one
of the contributing factors to these high mortality
rates and some of the barriers to the utilisation of
maternal health care services include social and
cultural/traditional beliefs and practices (Sharan et
al., 2009). Therefore, one of the strategies of the
Ministry of Health for addressing these problems is
to establish and strengthen community initiatives for
Maternal and Neonatal Health (MoH, 2007).
2.1 Community Health Workers
in Maternal and Neonatal Care
There are different types of health workers involved
in maternal and child health services within the
communities both from the formal/modern health
system and the traditional side. The traditional
health system consists of women known as
Traditional Birth Attendants (TBAs). The TBAs
used to have more established links with the modern
health sector as some had been trained to support
primary health care (MoHP, 2001). However, in
2007, the TBAs role changed from a service
provider for antenatal care and deliveries to a safe
motherhood advocate to refer women to health
facilities (Kanjo and Kaasbøll, 2009).
The formal/modern health system has
Community nurses, Health Surveillance Assistants
(HSAs), and Village Health Workers involved in
provision of community maternal and neonatal
health service, having been recruited and associated
with health facilities.
The community nurses are nurses in health
centres responsible for organising and providing
healthcare services in the community in addition to
providing services at the health centre. These
community nurses are expected to conduct outreach
clinics to provide antenatal care services.
Village Health workers (VHWs) are volunteers
who assist in various health programmes within their
villages and their duties include following-up on
PMTCT clients and facilitating community
sensitisation on HIV/PMTCT. The VHWs also assist
in identifying and registering pregnant women in the
village and reporting births that take place in the
village to the HSAs
The HSAs are the main link between the
communities and the health facilities; however, their
involvement in maternal and neonatal health
services has been limited as this was not established
as part of their duties. The research discovered it
was only in 2008 that the Ministry of Health in
partnership with donors started the establishment of
Community Based Maternal and Neonatal Care
(CBMNC) by piloting in three districts in Malawi
(Dowa, Chitipa and Thyolo). Therefore, the duties
and activities of HSAs in relation to maternal and
USE OF MOBILE TECHNOLOGY TO SUPPORT PROVISION OF COMMUNITY-BASED MATERNAL AND
NEONATAL CARE IN DEVELOPING COUNTRIES
261

neonatal health vary among the districts as well as
the health facilities.
In this study, the focus was on the HSAs as they
are the major link between the communities and the
health facilities and current Government efforts are
focusing more on their involvement in CBMNC.
3 RESEARCH METHODOLOGY
The study was conducted in three districts in Malawi
namely Lilongwe, Dowa and Machinga. A total of
17 rural health facilities were visited, the majority
being health centres (12). Other facilities visited
were rural hospitals (3) and district hospitals (2).
A qualitative research approach was adopted in
order to obtain a deep understanding of the work and
activities of the HSAs and their related information
and communication needs. Thus, qualitative data
collection techniques such as interviews and
document reviews were employed. Additionally,
review of existing software applications in use for
data management and communication was done.
To acquire information on the HSAs and their
work in relation to maternal and neonatal health
care; 26 nurses, 12 Health Surveillance Assistants
and 2 district coordinators of the community-based
maternal and neonatal healthcare programmes were
interviewed individually. The interviews provided
data on the community based programme activities
and procedures, data collected, reported and the
reporting systems.
Documents such as service registers, CBMNC
programme forms and Village Health Registers were
reviewed to obtain data on the information
requirements of the HSAs and the programme.
4 M-HEALTH APPLICATIONS
IN DEVELOPING COUNTRIES
The high diffusion of mobile technology in
developing countries has led to the widespread
conviction that the adoption of mobile applications
can be beneficial in supporting health care delivery
in developing countries (UnitedNations,
2007;VitalWaveConsulting, 2009). Statistics
indicate that in 2008, Malawi had 1.2 fixed phone
lines per 100 inhabitants, mobile cellular
subscription was at 12 per 100 people and the
proportion of households with internet was 1.7,
thereby indicating the diffusion of mobile telephony
is higher than that of the Internet and fixed line
telephones (ITU, 2010).
There are various ways in which mobile
technology can be used to support health service
delivery. According to Iluyemi and Briggs (2009),
sustainable improvement in healthcare in developing
country can be brought about by providing CHWs
access to reliable health information and mobile
applications present opportunities to complement
conventional methods of accessing and
disseminating this information effectively.
Additionally, the mobility of CHWs activities can
very much be accommodated by using mobile
applications to meet their information requirements
(Chatterjee et al., 2009).(Mechael et al., 2010) also
indicate that m-health applications present an
opportunity to break down the traditional
information barriers between diagnosis and
treatment and surveillance activities.
Furthermore, (Mechael et al., 2010) report that
mobile technologies have been found to increase
communication between health professionals and
community health workers in developing countries
through the use of voice calls and SMS applications
thereby resulting in a collaborative support system
and better patient care.
Several studies have presented various uses of
mobile applications for improving health service
delivery at community level in developing countries
with most cases focusing on their use to monitor and
support treatment for chronic infectious diseases
such as HIV/AIDS and TB (Mechael et al., 2010;
Kinkade and Verclas, 2008; Manda, 2009; United
Nations, 2007). Other cases have also presented the
use of mobile technology for collecting child
nutrition data and the Integrated Management of
Child Infections (IMCI) data within the community
(DeRenzi et al., 2008;UNICEF, 2009). Literature on
the use of similar applications to support maternal
and neonatal health care has been limited thus
indicating limited use of m-health applications in
this health domain. The few cases presented
portrayed how mobile devices such as Walkie-
talkies and cell phones were being used for voice
communication among service providers for referral
cases as well as consultation on delivery cases
(Musoke, 2002;Mechael, 2005).
Nevertheless, more recently, several cases have
been presented which are focusing on using m-
health applications to support maternal and neonatal
healthcare in various ways including collecting data
on the mother and infant’s condition for patient
monitoring, referring the mother or infant to health
HEALTHINF 2011 - International Conference on Health Informatics
262

facilities and follow-up care (Dimagi;UnitedNations,
2007).
A summary of m-health applications and projects
in use by community health workers is presented in
table 1 below. Even so, (Mechael et al., 2010)
indicate there is need for studies that investigate the
use and development of Electronic Health Records
(EHRs) on mobile phones because EHRs have the
potential to create a foundation for which the scope
of m-Health can be realized.
5 FINDINGS
The findings of this study are on the activities of the
Health Surveillance Assistants (HSAs) who were
involved in Maternal and Neonatal Healthcare at
community level and the associated information and
communication needs for those activities. Four main
activities of the HSAs were identified and are
presented in the subsections that follow.
5.1 Follow-up on Antenatal Clients
The HSAs conduct follow-up on pregnant women
within their communities and there are basically two
types of follow-ups. The first type is follow-up on
pregnant women who had attended antenatal clinic
and were expected to have delivered in a particular
month but they had not gone to the health centre for
delivery. The second type is part of the PMTCT
programme whereby follow-up is done on HIV
positive pregnant women who have missed their
appointments. The follow-ups are initiated by the
health centre nurses who provide the clients’
residential details to the appropriate HSA. The HSA
provide feedback on the follow-up in special cases
e.g. if the woman has moved to another location.
In some heath facilities, a mobile-based
application, FrontlineSMS, is being used to
communicate the details of clients needing follow-
up to the appropriate HSA and/or VHW.
Table 1: Mobile-Health Applications used by Community Health Workers.
m-Health
Application
Functions Goals
Countries
Implemented
CommCare
- Manage household visits
- Assist in planning daily activities
- Record information on mother and child’s
conditions and birth data
- Transmission of data/information to a central
repository
- Referral of infant or mother in need of medical
attention
- To provide better and efficient health
care
- Enabling supervision and coordination
of community health programs
- Enabling monitoring and evaluation of
the community health programs
- Tanzania
- Bangladesh
(Dimagi;Lesh)
Nacer
- Communicating and exchanging critical health
information among health professionals for:
patient monitoring, patient referral, follow-up
care and disease surveillance
- To improve communication among
health professionals
- Share data with hospitals when referring
patients
- Receiving feedback for follow-up
- Peru (United
Nations, 2007)
MoTeCH
- Recording patient encounter information (i.e.
mother/child assessment and treatment given)
- Tracking of patients
- To increase the quality and quantity of
antenatal and neonatal care in rural
Ghana
- Ghana
(Heatwole,
2010)
Cell-Life
- Accessing real-time health records of ART
clients
- Collect information on drugs and side effects,
and relevant socio-economic indicators.
- Monitoring and providing feedback to the
CHWs as required
- Management of the HIV/AIDS
epidemic by providing real-time voice
communication between the care
manager and CHWs
- South Africa
(United
Nations, 2007)
e-IMCI
- Provide decision support tool to guide health
workers in the management of childhood
illnesses based on WHO protocols
- Facilitate standardised diagnosis and
treatment of common childhood
illnesses.
- Tanzania
(DeRenzi et
al., 2008)
FrontlineSMS
- Communicating patient condition and treatment
given during home-based care
- Provision of treatment guidance
- Enables communication and
coordination among health workers on
home-based care.
- Malawi
(Manda, 2009)
USE OF MOBILE TECHNOLOGY TO SUPPORT PROVISION OF COMMUNITY-BASED MATERNAL AND
NEONATAL CARE IN DEVELOPING COUNTRIES
263

5.2 Provision of Community based
Maternal and Neonatal Care
The HSAs are required to conduct household visits
during the antenatal period and the early postnatal
period, thus, they need to identify and maintain lists
of all pregnant women within their catchment areas.
The HSA is expected to conduct at least three
household visits to the woman during her pregnancy
in which the following activities are done:
1. Review of the woman’s health record which is in
form of a health passport.
2. Assessment of the client’s current health status
by interviewing the woman. If danger signs are
discovered, the HSA refers the client to the health
centre.
3. Provide heath education and counselling based
on the findings of the review and assessment.
4. Develop a birth plan to help the woman prepare
for delivery and the newborn.
The HSA is also required to make at least three
visits at home after delivery and within 8 days after
delivery, the first visit being day 1 after delivery
especially for home deliveries. In order to make
these visits in the appropriate timeframe, the HSA
needs to be informed when the delivery has
occurred. This is done by either the woman’s
guardian, a village health committee member or a
VHW who sends a message or either visits the HSA
in person.
During the postnatal visits, the following
activities are conducted by the HSA:
1. Obtain the labour and delivery details by
reviewing the health passport if a delivery occurred
at a health centre. Other details are also obtained
from interviewing the woman since not all the
details are recorded in health passports.
2. Assessment of the current health status of mother
and baby and if any danger sings/illnesses are
discovered, they are referred to the health centre.
3. Provide health education and counselling on
danger signs and family planning.
The details and findings of the activities conducted
during antenatal and postnatal household visits are
recorded on CBMNC register forms.
Two kinds of reports are submitted by HSAs to
their supervisors: a CBMNC register form
containing client-level data and a monthly reporting
form containing aggregated data for the catchment
area. The CBMNC register forms are reviewed then
forwarded to the district programme offices where
the data is entered into a Microsoft Access database
application and different types of reports are
produced. On the other hand, the submitted monthly
reports are compiled by the supervisor to produce a
report for the whole facility and this is then
submitted to the district programme coordinator. It
was noted that availability of reporting forms to the
HSAs was usually a problem and requests for
stationary (e.g. reporting forms) were at times
communicated by the HSAs to their supervisors
using mobile phones.
In addition to these activities, the HSAs follow-
up on the clients they refer to the health centre in
order to make sure the clients have gone to the
health centre. This follow-up is done by asking the
nurse at the health centre or by checking the health
centre service registers. Alternatively, the HSA may
also visit the client again after several days to check
whether they actually went to the health centre.
5.3 Monitoring the Antenatal and
Delivery Service Provision using
Village Health Registers
The HSAs are required to capture demographic and
health information of each individual in their
catchment areas as a way of monitoring the
implementation of the Essential Health Package
(EHP) at household level.
Village Health Registers (VHR) are designed to
fulfil this purpose and the details recorded include
household demographic information and antenatal
care and delivery, among others. These details are
obtained from health passports and interviewing
individuals.
5.4 Provision of Maternal Health
Education and Counselling
The HSAs provide education and counselling on
maternal health issues to the community through
community gatherings and outreach clinics. The
community sensitisations gatherings are sometimes
conducted based on information from health centres.
For instance, one nurse explained that they were
getting cases of women delivering before arrival at
the health centre from a particular area and therefore
informed the HSA of that area, who then conducted
a sensitisation campaign.
HEALTHINF 2011 - International Conference on Health Informatics
264

6 PROSPECTS ON USING
M-HEALTH APPLICATIONS
The findings in section 5 indicate that HSAs are
using mobile phones for communicating with their
supervisors and voice phone calls are the most
common use of the mobile phones. This is similar to
cases presented in literature (Mechael et al.,
2010;Mechael, 2005;Manda, 2009). In some health
centres, the FrontlineSMS platform is being used to
request for follow-ups and provide feedback on the
follow-up cases thereby improving communication
among the health workers. This is also similar to
other studies presented in literature
However, based on the activities of the HSAs
and the associated information requirements, we
examine the potential areas in which Electronic
Health Records (EHR) and m-health applications
could be used in tandem to support the information
and communication needs of the HSAs.
6.1 Shared Access
to Healthcare Records
The findings indicate the HSAs require information
on healthcare provided at health centres and this
information is currently obtained from health centre
staff, service registers and health passports. This
demonstrates the need for shared access to the health
records of clients and this can be achieved through
implementing an EHR system that is accessible
through mobile technology to CHWs as
implemented in other projects presented in the
literature (UnitedNations, 2007).
The HSAs also require feedback on the clients
they refer to health centres and this is currently
obtained by asking the nurse at the health centre, or
checking the service registers or visiting the client
again. All this is time-consuming and having an
EHR/mobile health application that enables the HSA
to follow-up on a client’s health record would be
beneficial in saving time on the follow-up.
Additionally, some new clients are identified by
the HSAs in the community and then referred to the
health centre for healthcare services. With an EHR
and a mobile application, the HSAs would be able to
register new clients and refer them to the health
centres electronically as is done using the
CommCare application.
6.2 Data Collection
and Guiding Healthcare Protocol
The findings indicate that data is collected on the
condition of the women and /or their newborn babies
in order to assist in the early identification of danger
signs. This client-level data is then sent for data
entry into a computer database at the district level
which results in a bulk of forms needing to be
entered at the district level. With a mobile-based
health application, the HSAs would be able to
capture the data directly to an EHR system thereby
improving timeliness and availability of the data.
Additionally, this would increase the access to
information on deliveries occurring at home or by
TBAs thereby enabling health centre staff to monitor
births taking place within the community.
Furthermore, the research discovered that HSAs
faced challenges in the assessment of clients which
resulted in clients wrongly diagnosed as having
danger signs and this can be attributed to the fact
that the HSAs have a non-medical background and
are new to maternal and neonatal healthcare. Thus,
with an application that guides the health worker in
the assessment of clients, as is implemented in
CommCare, the accuracy on the assessment (and
data) would be improved. This has been
demonstrated in other applications such as the
implementation of the e-IMCI in Tanzania (DeRenzi
et al., 2008) and (Mechael and Dodowa Health
Research Centre, 2009) advocate for such an
application.
6.3 Providing Notification on Deliveries
The HSA needs to be informed when a delivery
occurs and the woman has been discharged.
However, the current mechanisms for obtaining this
information are unreliable and chances are the HSA
can go for days without knowing or being informed
about the birth especially with the fact that one
HSA’s catchment area spans over several villages.
Thus to ensure the HSA is informed on time, getting
updates from the EHR system when a birth/delivery
occurs at the health facility would ensure the HSAs
are immediately informed and therefore, can
schedule the necessary postnatal visit.
6.4 Providing Follow-up Requests
The health centre nurses use the HSAs to follow-up
on certain clients and this requires that the nurse
should identify the clients, identify the right HSAs
and then communicate the details of the clients
needing follow-up to the HSAs. The findings,
however, indicate that due to high workload and low
staffing levels in health centres, the nurses are not
able to compile such information hence resulting in
USE OF MOBILE TECHNOLOGY TO SUPPORT PROVISION OF COMMUNITY-BASED MATERNAL AND
NEONATAL CARE IN DEVELOPING COUNTRIES
265
poor follow-up service. With an EHR system that
can automatically identify clients needing follow-up,
and incorporates mapping of clients to appropriate
HSAs based on their residential addresses, the EHR
system would enable automated requests to be sent
to the HSAs, thereby relieving the nurses of this
cumbersome task.
6.5 Overall Design of EHR / M-health
System
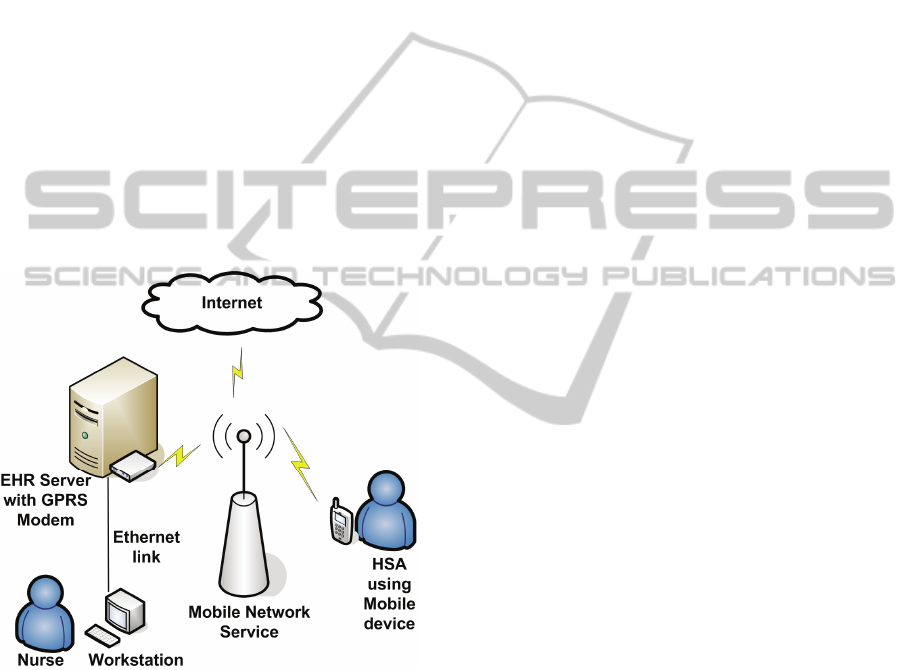
In essence, the proposed overall setup of the system,
represented in Figure 1 below, is to have an
Electronic Health Record system implemented on a
server located at the health centre which the HSA is
associated with. The EHR system will be accessible
to local health workers at the health centre using
workstations connected to the server on a LAN. The
Server will have a GPRS modem to enable remote
access to the health records by HSAs using a
mobile-based application.
Figure 1: Overall design of the EHR/m-health system.
7 CONCLUSIONS
Adaptation of mobile technology in the HIS in
developing countries is in the infant stages however
promising results have been identified in different
contexts showing improvements in health care
delivery (Dimagi; Manda, 2009; United Nations,
2007). Through a detailed analysis of the current
activities of Community Health Workers, the
findings have indicated potential benefits of using
mobile technology coupled with EHRs in improving
delivery of maternal and neonatal health at the
community level in Malawi.
Thus, the next stage of this ongoing research is
the implementation of the EHR/mobile applications.
The study will continue to explore existing systems
such as CommCare and MoTECH with the aim of
building on these already existing infrastructures and
collaborating with other organisations implementing
similar interventions.
REFERENCES
Chatterjee, S., Chakraborty, S., Sarker, S., Sarker, S. &
Lau, F. Y. (2009) Examining the success factors for
mobile work in healthcare: A deductive study.In
Decision Support Systems, 46, 620-633.
Derenzi, B., Parikh, T., Mitchell, M., Chemba, M.,
Schellenberg, D., Lesh, N., Sims, C., Maokola, W.,
Hamisi, Y. & Borriello, G. (2008) e-IMCI: Improving
Pediatric Health Care in Low-Income Countries.In
ACM, 978.
Dimagi CommCare- Community health mobile platform.
Ghwa (2008) Pakistan's Lady Health Worker Programme.
Country Case Study. WHO.
Heatwole, A. (2010) MoTeCH: A Mobile Approach to
Maternal Health Care.
Illuyemi, A. & Briggs, J. S. (2010) Wireless Access and
Connectivity for Community Based Health Workers in
Developing Countries: Models. Question 14-2/2 Final
Report: Mobile eHealth solutions for Developing
Countries Geneva, ITU.
Itu (2010) Measuring the Information Society 2010. IN
ITU-D (Ed.).
Kanjo, C. & Kaasbøll, J. (2009) Rules,Reality and Results:
Inter-Institutional Coordination and Impact on Health
Information Systems in Developing Countries. IN
MOLKA-DANIELSEN, J. (Ed.) 32nd Information
Systems Research Seminar in Scandinavia, IRIS 32,
Inclusive Design. Molde, Norway.
Kinkade, S. & Verclas, K. (2008) Wireless Technology for
Social Change: Trends in Mobile Use by NGOs.
Access to Communication Publication Series. .
Washington, DC and Berkshire, UK, UN Foundation–
Vodafone Group Foundation Partnership.
Lesh, N. CommCare: Lessons in Interoperability.
Manda, T. D. (2009) Understanding Opportunities and
Challenges in Using Mobile Phones as a Means for
Health Information Access and Reporting: A Case
Study from Malawi. Department of Informatics. Oslo,
University of Oslo.
Mdgafricasteeringgroup (2008) Achieving the Millennium
Development Goals in Africa:Recommendations of
the MDG Africa Steering Group. New York.
Mechael, P., Batavia, H., Kaonga, N., Searle, S., Kwan,
A., Goldberger, A., Fu, L. & Ossman, J. (2010)
Barriers and Gaps Affecting mHealth in Low and
Middle Income Countries: Policy White Paper. The
HEALTHINF 2011 - International Conference on Health Informatics
266

Earth Institute Columbia University
mHealth Alliance.
Mechael, P. N. (2005) Mobile phones for mother and child
care.In Information for Development.
Mechael, P. N. & Dodowahealthresearchcentre (2009)
MoTECH: mHealth Ethnography Report. The
Grameen Foundation.
Moh (2007) Road Map for Accelerating the reduction of
Maternal and Neonatal Mortality and Morbidity.
Mohp (2001) Malawi National Health Accounts: A
broader Perspective of the Malawian Health Sector.
Musoke, M. G. N. (2002) Simple ICTs reduce maternal
mortality in rural Uganda. A telemedicine case
study.In Bulletin of Medicus Mundi Switzerland, 85.
Nso (2008) 2008 Population and Housing Census Results.
IN NSO (Ed.). Zomba, NSO.
Savethechildren (2010) Women on the Front Lines of
Health Care: State of the World's Mothers 2010. Save
the Children.
Sharan, M., Ahmed, S., Malata, A. & Rogo, K. (2009)
Quality of Maternal Health Services in Malawi: Are
Health Systems Ready for MDG 5. Africa Human
Development, The World Bank.
Unicef (2008) Countdown to 2015:Maternal, Newborn &
Child Survival. Tracking Progress in Maternal,
Newborn and Child Survival: The 2008 Report. New
York, UNICEF.
Unicef (2009) Using Mobile Phones to Improve Child
Nutrition Surveillance in Malawi.
Unitednations (2007) Compendium of ICT Applications
on Electronic Government. Volume 1: Mobile
Applications on Health and Learning. IN DESA (Ed.).
New York.
Vitalwaveconsulting (2009) mHealth for Development:
The Opportunity of Mobile Technology for Healthcare
in the Developing World. Washington, D.C.
Berkshire, UK, UN Foundation-Vodafone Foundation
Partnership.
USE OF MOBILE TECHNOLOGY TO SUPPORT PROVISION OF COMMUNITY-BASED MATERNAL AND
NEONATAL CARE IN DEVELOPING COUNTRIES
267
