
INTEGRATING CLINICAL INFORMATION FROM A PERSONAL
HEALTH RECORD INTO THE VIRTUAL HEALTHCARE RECORD
Andrei Vasilateanu, Luca Dan Serbanati
Universitatea Politehnica Bucuresti, Facultatea de Inginerie in Limbi Straine, Splaiul Independetei 313, Bucuresti, Romania
Mihai Isaroiu
Universitatea Politehnica Bucuresti, Facultatea de Inginerie in Limbi Straine, Splaiul Independetei 313, Bucuresti, Romania
Keywords:
eHealth, EHR, PHR.
Abstract:
In this paper we describe our proposed architecture for an integrated eHealth solution based on a patient-
centric electronic health record called Virtual HealthCare Record (VHCR). VHCR is a central, unifying,
internet-based entity acting as a flagship in the eHealth ecosystem and integrating different sources of medical
information in a longitudinal record. The focus of this paper is how VHCR interacts and integrates data from
a Personal Health Record.
1 INTRODUCTION
In the previous years e-Health has become a ma-
jor concern in the academic, medical and business
worlds. In the context of an ageing population in the
developed countries e-Health promises to be a solu-
tion for the increasing costs demanded by healthcare.
An important concept in e-Health is the use of the
Electronic Health Record (EHR), that is an individual
patient’s medical record in digital format. It enables
a doctor to keep better track of her/his patients, to is-
sue documents that can be interpreted by other doc-
tors and other EHRs. EHR systems reduce medical
errors, increase physician efficiency and reduce costs,
as well as promote standardization of care.
Another concept is the patient empowering,
namely involving the patient in his/her treatment pro-
cess by giving him the means to make informed de-
cisions. One of the ways to support patient empow-
ering is the use of Patient Health Records (PHR), IT
applications designed to allow the patient to manage
his/her clinical information
From the many fields of e-Health we choose
to concentrate on improving the continuity of care,
by designing and implementing a shared, elec-
tronic record which we named Virtual HealthCare
Record.(Contenti et al., 2010) VHCR is a longitudi-
nal record, spanning over the whole life of the patient
and integrating distributed and heterogeneous sources
of information. VHCR is designed as a multiagent
system in which stakeholders involved in the health-
care process centered on a patient are represented by
agents organized in agencies cooperating to maintain
a complete and accurate virtual representation of the
patient‘s health state and clinical history as well as to
support distributed health care processes.(Luzi et al.,
2006)
From the many sources of information which the
VHCR mediates and integrates this paper focuses on
the interaction with a personal health care record,
managed by the patient, with the purpose of involv-
ing the patient as a proactive party in the health care
process.
In the following a more detailed view of VHCR is
presented and the PHR is introduced. Then we pro-
pose a methodology for the interoperability between
the PHR and VHCR highlighting advantages as well
as the factors resisting to change, the potential pitfalls
in implementation and usage.
2 VHCR
The Virtual HealthCare Record is the flagship in
our envisioned digital health ecosystem(Kim et al.,
2007).VHCR is not a document repository; instead it
is a provider of electronic services supporting health-
521
Vasilateanu A., Dan Serbanati L. and Isaroiu M..
INTEGRATING CLINICAL INFORMATION FROM A PERSONAL HEALTH RECORD INTO THE VIRTUAL HEALTHCARE RECORD.
DOI: 10.5220/0003138405210524
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2011), pages 521-524
ISBN: 978-989-8425-34-8
Copyright
c
2011 SCITEPRESS (Science and Technology Publications, Lda.)

care processes. It holds data extracted from medi-
cal documents from various sources in a finer grained
model than the documental model permits. The
model is derived from HL7 RIM v3 and European
Continuity of Care standards like CONTSYS and
based on a dedicated ontology. In this model medical
data is organized into episodes of care which are ini-
tiated or appended during encounters with the health-
care providers by accessing the VHR services.
VHCR‘s purpose is to maintain a unified, coherent
and consistent view on the clinical status of the patient
by integrating healthcare events generated through-
out the whole life of the patient by different enti-
ties. These documents can derive from the healthcare
applications of the healthcare providers like general
practitioners or specialists in the form of prescrip-
tions, procedures and referrals organized into care
plans, from laboratories in the form of blood tests or
x-ray images or from medical devices like intelligent
measurement devices for blood pressure of glicemy
which can send the results wirelessly to a proxy.
These documents are digitally signed by an au-
thorized healthcare provider before being integrated
within VHCR. Once the data has been integrated, and
a “snapshot“ of the patient clinical status is avail-
able, VHCR becomes a complex e-service provider,
generating and providing customized views on this
integrated status to the stakeholders involved in
the healthcare process and responding to complex
queries. Before presenting how we can also integrate
data from PHRs let us describe in detail what PHRs
represent.
3 PATIENT EMPOWERMENT
AND PHR
A trend in healthcare is to involve the patient as a
pro-active party in his/her own treatment. Patient em-
powerment involves raising the health literacy, pro-
viding customized, sanctioned medical information to
the patient as required by his/her condition or level
of training with the purpose of giving the patient
the means to make informed decisions regarding the
treatment. Health literacy denotes the skills neces-
sary to understand and use health information. Pa-
tients with chronic illnesses will be able to follow
and manage their diseases in cooperation with their
care providers, promoting earlier interventions when
they encounter a deviation or problem. Parents can
also monitor the immunizations, diet and treatment
of their children. Also, using evolved search engines,
they can search and retrieveinformation from credible
medical knowledge basis including advices regarding
emergency interventions in domestic accidents, sim-
ple medical conditions (common colds, indigestions)
or tending to very young children.
Another issue is supporting the patient in pre-
venting illness by raising the awareness to a healthy
lifestyle. Taking into consideration that while at the
turn of the last century most of the deaths were caused
by acute diseases while at the moment 2/3 of the
deaths are caused by chronic diseases and that these
chronic diseases are caused not by one but by many
risk factors, hard to quantify and deriving from the
environment and lifestyle of the patient, it becomes
ever more important to inform the patient in leading a
healthy lifestyle. These concerns are addressed by a
concept and family of products called Personal Health
Records or Patient-centered Health Records. A defi-
nition for PHR can be the following:
an electronic application through which
individuals can access, manage, and share
their information, and that of others for whom
they are authorized, in a private, secure envi-
ronment.
(Brennan et al., 2007)
In addition to conditions, medications, appoint-
ments PHRs also provide a repository for self-
monitoring information or nutritional facts.
As we can see the main difference between an
EHR and PHR is the fact that in a PHR data is in-
troduced and governed mainly by the patient. At the
moment different commercial PHR solutions exist on
the market, from which we mention the products from
important players like Google - Google Health and
Microsoft -Microsoft Health Vault.
4 INTEROPERABILITY
BETWEEN PHR AND VHCR
Since VHCR aims to aggregate and integrate relevant
clinical information for a patient it is clear that the
PHR is an important source which should not be left
out. Also, since PHR represents the patient‘s view
into his health status, important clinical events from
the VHCR should be integrated as well into the PHR.
4.1 VHCR to PHR
The main concern when importing data from VHCR
to PHR is translating medical data from a health care
provider representation to a patient representation.
The data organization in VHCR into health issues,
episodes of care and contacts could prove not very
relevant to the patient and should be reorganized in a
HEALTHINF 2011 - International Conference on Health Informatics
522

more intuitive way. Also the specificity of medical in-
formation should be adapted to the health literacy of
each patient, health literacy which changes in time.
4.2 PHR to VHCR
The main obstacle is the fact that for clinical infor-
mation to be imported into VHCR it needs to be ap-
proved via signing by a healthcare professional, in
this case the general practitioner. The general prac-
titioner has objective but also subjective reasons to
refuse to do so:
• Not reimbursed to do it. Doctors can view spend-
ing time in filtering information from the PHR to
VHCR as a waste of their time since it is an ac-
tivity for which they are not financed. One way
to encourage doctors to guide their patient in us-
ing IT-enabled, patient empowering tools is to re-
imburse “e-Visits“ (Tang et al., 2006), namely
the virtual encounter between the doctor and the
patient. Moreover, even without reimbursement,
the previous virtual encounter with the healthcare
provider can make the actual encounter more pro-
ductive and more focused, using the provider‘s
time more effectively and lowering the commu-
nication barrier.
Also in the case of pediatric doctors with young
children registered in their care, the PHR can
prove very helpful as it frees them from contin-
uous domestic visits or visits of the parents with
their children to the cabinet, by being able to mon-
itor remotely the children evolution and to raise
the responsibility with the parents.
• Not willing to take responsibility for unchecked
data. Once a fact from the PHR is integrated into
VHCR via his signature, the doctor becomes re-
sponsible for that entry.
While some of these obstacles can be overcome by
changing legislation (e.g. reimbursing eVisits) we be-
lieve that technology can also play a part in assisting
the GP, by partially automizing the filtering process
and using notifications.
5 IMPLEMENTATION
VHCR is implemented using a service oriented archi-
tecture(Serbanati and Vasilateanu, 2008). The POS
uses a wrapper that transforms the output from the
EHR application to a HL7 compliant message that
is sent to the intelligent broker which forwards it to
VHCR component. The broker is also responsible for
sending notifications to the interested parties.
In the present prototype we add to the POS a fil-
tration subsystem based on an automatic, rule based,
system that analyzes the coherency of data (double
submits, submits with no body, etc) which commu-
nicates directly with the PHR. The PHR chosen for
this proof-of-concept was Google Health (McBride,
2008), which implements a partial subset of Continu-
ity of Care Record (CCR)(Ferranti et al., 2006).
The information inspected for validation is repre-
sented by the Problems element and Medication ele-
ment. The PHR used does not allow an asynchronous
retrieval of medical information introduced therefore
a synchronous retrieval of data must be implemented;
the data is retrieved by a worker thread created and
started on the start of the application. The POSDi-
gester is responsible for retrieving data for all pa-
tients marked as registered at the logged in physician,
afterwards for all new information it generates no-
tifications which are processed by the filtration sys-
tem. The flow of the validation process from PHR to
VHCR is presented in fig 1. The system receives noti-
fications when in PHR either a new medicine is added
or a new symptom is added and these two types of
notifications are processed differently:
• If the notification is a symptom and its syntax is
correct, it is displayed as an alert to the physi-
cian in charge; the physician can either classify
it medically irrelevant and the flow stops, or it can
be classified medically relevant and an encounter
event is created (ADT) and sent to the VHCR.
The encounter can belater appendedto an existing
medical episode, or it can generate a new medical
episode on its own.
• If the notification is a new medicine its counter
indications are checked; if there are no known in-
teractions between the medicine and other drugs
or conditions than it is disregarded. If the previ-
ous condition is not fulfilled then a check is made
to see if the new drug has interactions with an ex-
isting patient condition and if this is so then an
encounter(ADT) should be created automatically
and an alert displayed; if the medication has in-
teractions with other drugs , therefore this infor-
mation should be taken into account for further
prescriptions, the information is appended to the
VHCR and the physician is alerted.
To include data from VHCR to PHR, PHR must
register as a client to the notifications dispatched by
the VHCR. To make a customized selections of what
types of events should be included in PHR, we have
devised a proxy service between the PHR and VHCR.
In effect the proxy registers to VHCR notifications
and it forwards them selectively to PHR. The proxy
also acts as a translator, transforming HL7 messages
INTEGRATING CLINICAL INFORMATION FROM A PERSONAL HEALTH RECORD INTO THE VIRTUAL
HEALTHCARE RECORD
523
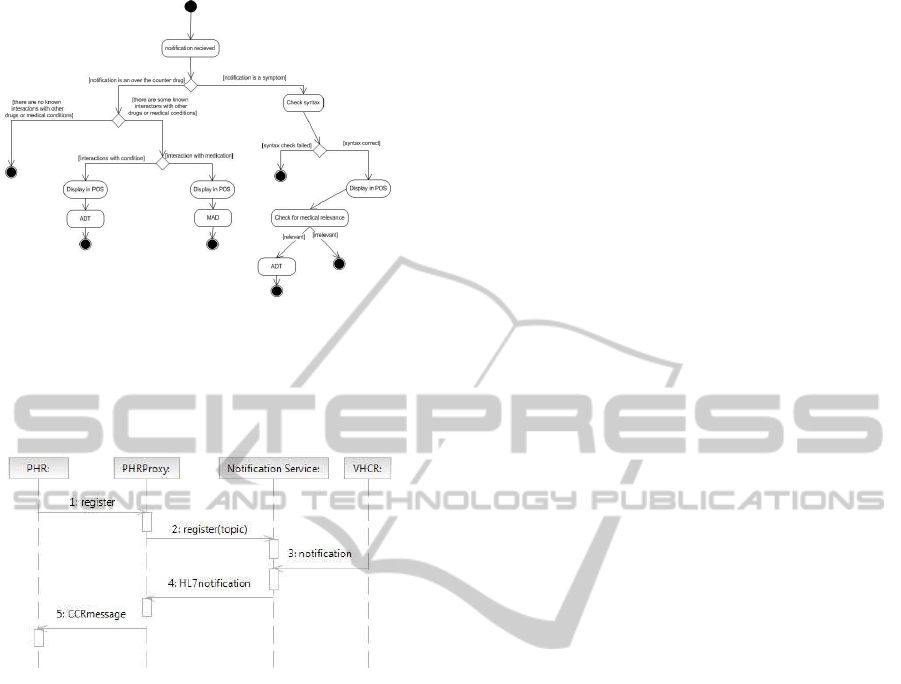
Figure 1: PHR to VHCR validation.
to CCR standard, which can be interpreted and inte-
grated by Google Health. The process is described in
detail in fig 2.
Figure 2: PHR notification through proxy.
6 CONCLUSIONS AND FURTHER
IMPROVEMENT
PHR represents an important source of information
for having a comprehensive view on the patient‘s
health. It not only allows to raise the patient‘s re-
sponsibility to health issues in general, and his/her
treatment in particular, but it can be used to obtain
information from a primary, direct interested source.
Our prototype filtration system and PHR proxy act
in fact as semantic mediators between the patient‘s
view and the healthcare professionals‘ views on the
curative process, overcoming the language barriers to
bring them together in a virtual, reconciled space.
Further improvements can be made in raising the
autonomy of the filtration system by using intelligent,
adaptive agents, which can learn from the patient’s
preferences and previous choices. Also we are ex-
tending the number of PHR applications which can
be integrated in the system. Contemporarly we are
designing vocabularies and a general ontology de-
scribing concepts belonging to PHR functions, from
which a general filtration system can be customized
autonomously.
REFERENCES
Brennan, P., Downs, S., Casper, G., and Kenron, D. (2007).
Project HealthDesign: Stimulating the Next Genera-
tion of Personal Health Records. In American Medical
Informatics Association.
Contenti, M., Mercurio, G., Ricci, F., and Serbanati, L.
(2010). The LUMIR Project: Developing the GPs
Network Pilot Program in the Basilicata Region. In-
formation Systems: People, Organizations, Institu-
tions, and Technologies, pages 255–263.
Ferranti, J., Musser, R., Kawamoto, K., and Hammond, W.
(2006). The Clinical Document Architecture and the
Continuity of Care Record. British Medical Journal,
13(3):245.
Kim, H., Lee, J., and Han, J. (2007). The Roles of Informa-
tion Technology in Business Ecosystems from a Flag-
ships Perspective. In Proceedings of the Korea Man-
agement Information Systems Fall Conference, pages
343–348.
Luzi, D., Ricci, F., and Serbanati, L. (2006). E-Clinical
trials supported by a service-oriented architecture. in
MedNet.
McBride, M. (2008). Google Health: Birth of a giant.
Health Management Technology, 29(5):8–9.
Serbanati, L. D. and Vasilateanu, A. (2008). Supporting
Continuity of Care with a Virtual Electronic Health
Record. In IHIC, pages 84–87.
Tang, P., Black, W., and Young, C. (2006). Proposed crite-
ria for reimbursing eVisits: content analysis of secure
patient messages in a personal health record system.
In American Medical Informatics Association.
HEALTHINF 2011 - International Conference on Health Informatics
524
