
A PROPOSAL OF A NOVEL CARDIORESPIRATORY
LONG-TERM MONITORING DEVICE
S. Lapi, E. Biagi, G. Borgioli, M. Calzolai, L. Masotti
Department of Electronics and Telecommunications, University of Florence, Florence, Italy
G. Fontana
Department of Internal Medicine, University of Florence, Florence, Italy
Keywords: Wearable accelerometer, Cardiorespiratory holter, Sleep monitoring.
Abstract: Monitoring of respiratory movements is an important feature in planning of medical care. We present here a
simple, portable, accelerometer-based device suitable for long term-monitoring of the breathing and heart
rates, along with postural changes, during sleep and wakefulness. Recordings of respiratory frequency, heart
rate, posture and voluntary cough were obtained from a group of volunteers who also participated in sleep
studies (6-8 hrs). A pair of capacitive MEMS tri-axial accelerometers was positioned at the level of the 10
th
rib along the mid-axillary line bilaterally; simultaneous recordings of respiratory movements, heart rate and
body position could be easily performed. The signal were digitized and used to detect body position and
relative movement between accelerometers. Conventional spirometry was performed in parallel when
appropriate. During resting breathing, qualitative analysis revealed that the accelerometric assessment of
respiratory pattern correlated well with that obtained by spirometry. Values of respiratory rates were
identical with the two techniques. Recordings of respiratory and cardiac activity during sleep were
satisfactorily obtained except for short lasting episodes corresponding to changes in body position. These
devices seem to be also suitable for detecting the motor pattern of cough.
1 INTRODUCTION
It has repeatedly been shown that detailed analysis
of breathing pattern can provide valuable
information regarding the respiratory system (Tobin,
1983). In patients with respiratory and sleep
disturbances, including the chronic obstructive
pulmonary disease (Pauwels, 2001) and the sleep
apnoea syndrome (Britton, 2003), continuous
monitoring of simple vital functions may provide
useful therapeutic options. COPD is a prevalent and
disabling condition that results in significant
personal impact to patients and their carers, and
financial cost to health services. (Pauwels, 2001)
More than half of these costs relates to hospital
admissions for acute exacerbation (Britton, 2003).
Reducing exacerbations and hospitalizations are
therefore key goals in COPD management (Pauwels,
2001).
Obstructive sleep apnoea syndrome (OSAS) is a
highly prevalent disorder (Panossian, 2009)
characterized by instability of the upper airway
during sleep, which results in markedly reduced
or
absent airflow at the nose/mouth. Episodes are
typically
accompanied by oxyhemoglobin
desaturation and terminated by brief micro-arousals
that result in sleep fragmentation (Panossian, 2009).
Despite having significant breathing problems
during sleep, most patients have no readily
detectable
respiratory abnormality while awake
(Redline, 1993).
Conceivably, continuous monitoring of
respiratory and heart rates, cough frequency and
motor pattern, and time spent daily in physical
activities may provide early information on
deterioration of clinical conditions in patients with
respiratory diseases, thus allowing prompt medical
intervention and possibly reducing both the severity
of disease exacerbations and the need of sudden
hospitalization of the patient (Deegan, 1995). In
addition, domestic sleep monitoring by means of a
simple device that allows simultaneous assessments
38
Lapi S., Biagi E., Borgioli G., Calzolai M., Masotti L. and Fontana G..
A PROPOSAL OF A NOVEL CARDIORESPIRATORY LONG-TERM MONITORING DEVICE.
DOI: 10.5220/0003136100380042
In Proceedings of the International Conference on Bio-inspired Systems and Signal Processing (BIOSIGNALS-2011), pages 38-42
ISBN: 978-989-8425-35-5
Copyright
c
2011 SCITEPRESS (Science and Technology Publications, Lda.)
of cardiorespiratory rates and posture may represent
a useful tool in the management of OSAS patients.
Several devices have been proposed to measure
ventilation indirectly. Respiratory monitoring is
usually achieved by having a subject breathing
through a mouthpiece or face mask attached
to a
pneumotachograph or spirometer. Although these
devices permit
the accurate measurement of
ventilation and its variables, they
also alter the
pattern of breathing and minute ventilation
(McNicholas, 2008). They are not useful for
monitoring ventilation
in any circumstance in which
keeping a mouthpiece and nose clip
in place is too
difficult or
impossible, as it may be the case of
continuous monitoring at home and/or during sleep
(Hurst, 2009). Devices that measure changes in
thoracic volume (respiratory inductance
plethysmography), and airflow at the airway opening
(oro-nasal thermistors) have been fully validated and
largely employed in the clinical assessment of sleep
disturbances; however, it is widely recognised that
their use for recording respiratory activity during
daily life is impractical, mainly due to their limited
portability.
We present here a simple, mini-invasive,
accelerometer-based device that can be used for long
term-monitoring of respiratory movements and
cardiac activity, thus allowing the detection of the
breathing frequency and heart rate, along with the
ongoing postural changes, during sleep and
wakefulness. The device can also provide useful
information on the motor pattern of cough and other
expulsive efforts. In this connection, it seems worth
to recall that the cough reflex is an important airway
defensive mechanism and the assessment of its
functionality is becoming increasingly important,
especially in elderly patients who are at risk of
aspiration pneumonia (Perez, 1985). The intensity of
a cough effort, generally indexed in terms of
expiratory flow rate and/or electromyographic
abdominal muscle activity (Que, 2002) is of pivotal
importance in the assessment of cough effectiveness.
Specifically, the purposes of this paper are i) to
determine whether the accelerometer-based device is
suitable for short- and long-term recordings of
respiratory and heart rates in conditions such as
sleeping and daily activities; ii) to obtain preliminary
information on the feasibility of non-invasive
recording of more complex respiratory motor acts
such as the cough.
2 MATERIALS AND METHODS
The proposed device consists of two MEMS
capacitive tri-axial accelerometers (MMA7260Q,
Freescale Semiconductor) which were chosen for
their high sensitivity (800 mV/g @1.5 g).
Due to manufacturing process and physical
structure of each sensor, measures could be affected
by a systematic error; to offset the output of the
accelerometers used in the experimentation, a
calibration procedure was devised.
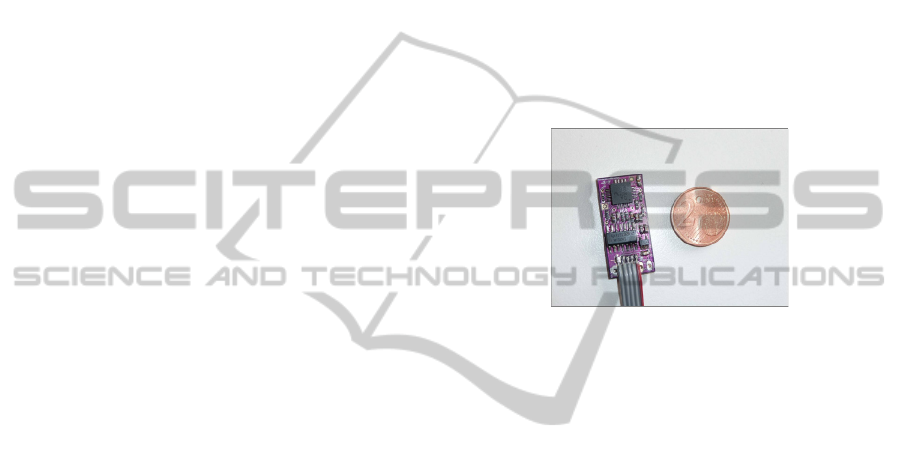
Accelerometric sensors were mounted on two
small circuit boards, as illustrated in figure 1,
containing a first conditioning module and a voltage
regulator.
Figure 1: Accelerometer mounted on the circuit board.
Note the small size of the device compared with a 2 Euro
cent coin.
Accelerometric sensors were positioned
bilaterally on the skin of the anterior thoracic wall at
the level of the 10
th
rib along the mid-axillary line,
by using paper adhesive bandage. In preliminary
experimental sessions, several different attempts at
identifying the most suitable thoracic area for sensor
positioning were carried out. The margin of the 10
th
rib on the mid-axillary line was selected as it turned
out to provide a respiratory signal consistent with
that obtained with conventional spirometry.
Both sensors were connected with a flexible flat
cable to a data acquisition board, containing
analogue conditioning circuits, A/D converter, a real
time clock for acquisition management and power
supply. The acquisition board is embedded in a
12 cm x 7 cm x 3 cm lightweight plastic case
equipped with a clasp on the back side for hanging
the device to the subject’s belt in order to improve
monitoring device’s portability.
Acceleration signals were sampled at 340 Hz,
stored in a removable mass memory device and later
transferred to the computer for off-line processing,
which included digital filtering, offset correction and
study of frequency components.
During offline processing two digital FIR filters
were used to extract the respiratory and cardiac
components from the raw signal, respectively in the
A PROPOSAL OF A NOVEL CARDIORESPIRATORY LONG-TERM MONITORING DEVICE
39
[0.1, 0.6] Hz and [1, 15] Hz frequency range.
However, the use of a digital filter “per se” is not
effective in removing signal components originating
from body movements unrelated to respiratory
activity; in facts, the frequency components of non-
respiratory body movements are generally lower
than 15 Hz and therefore comprised in the range of
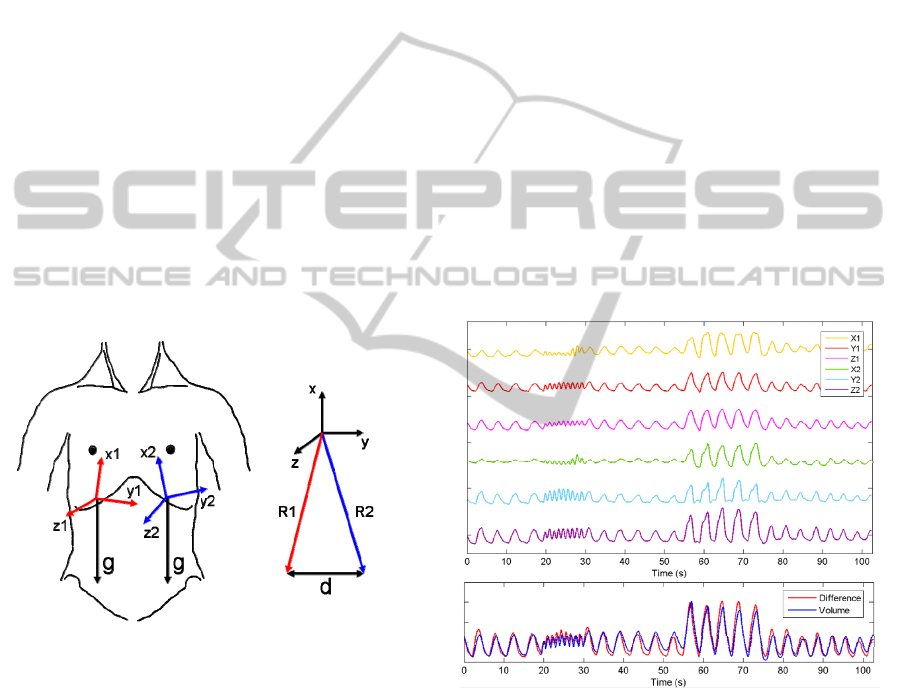
respiratory and cardiac signals. In consequence, the
influence of non-respiratory thoracic movements
was minimised by considering the difference ‘d’
between the sensor’s resultant vectors ‘R1’ and ‘R2’
(figure 2). By subtracting the common components
acquired from the two accelerometers, a signal of
purely respiratory origin was obtained. Once
positioned on the chest wall, however, the reference
co-ordinate systems of the two sensors were not
aligned, leading to a systematic error due to an
imbalance between common components. To avoid
imbalance, we developed a procedure that rotates the
reference system of one sensor in order to align it to
the reference system of the other sensor. With this
procedure, the accelerometric signals deriving from
non-respiratory thoracic movements were
minimised.
(a) (b)
Figure 2: Sensors location on the chest wall (a),
representation of resultant vectors ‘R1’, ‘R2’ and their
difference ‘d’ (b).
We recruited six subjects of both sexes (age
range 19 – 64) among faculty personnel and
students; none of them complained of any relevant
respiratory or cardiac disturbance and agreed to
participate in accelerometric recordings of
respiratory frequency and heart rate. Three other
subjects were selected to perform a series of
maximum voluntary cough efforts starting either
from near total lung capacity or from functional
residual capacity. Accelerometric measurements in
awaken patients were always performed in parallel
with conventional spirometry by using a mouthpiece
connected to a pneumotachograph which provided
standard outputs of respiratory volume and flow.
Nine additional subjects participated in sleep studies
lasting 6-8 hrs during which simultaneous
recordings of posture, respiratory and heart rate by
means of the accelerometers were obtained.
3 RESULTS
As expected, accelerometric recordings of
respiratory activity provided a precise measure of
respiratory rate in all subjects tested (figure 3, upper
panel); similar consideration were also valid for
heart rate recordings (figure 4). Furthermore, with
the subject seated in the upright position, qualitative
analysis of the recordings revealed that the pattern of
breathing obtained by considering the difference ‘d’
between the two accelerometers was fairly coherent
with that obtained with the spirometer (figure 3,
lower panel). In more detail, the different patterns of
rapid shallow breathing and deep breathing were
correctly detected by the accelerometers (figure 3).
Figure 3: Upper panel: respiratory signals from the
accelerometer pair: X, Y and Z are the signals originating
from each of the two tri-axial accelerometers. For the
purpose of morphological comparisons, all traces are in
arbitrary units and displayed at different levels. Lower
panel: morphological comparison of the spirometric
volume (in blue) and of the accelerometer signal
difference (in red) during normal breathing, rapid shallow
breathing and deep breathing. Signals were differently
amplified to allow superimposition.
As shown in figure 5, the accelerometric tracings
recorded during voluntary cough efforts of variable
intensity turned out to be clearly distinguishable
from those of resting breathing. The intensity of
BIOSIGNALS 2011 - International Conference on Bio-inspired Systems and Signal Processing
40
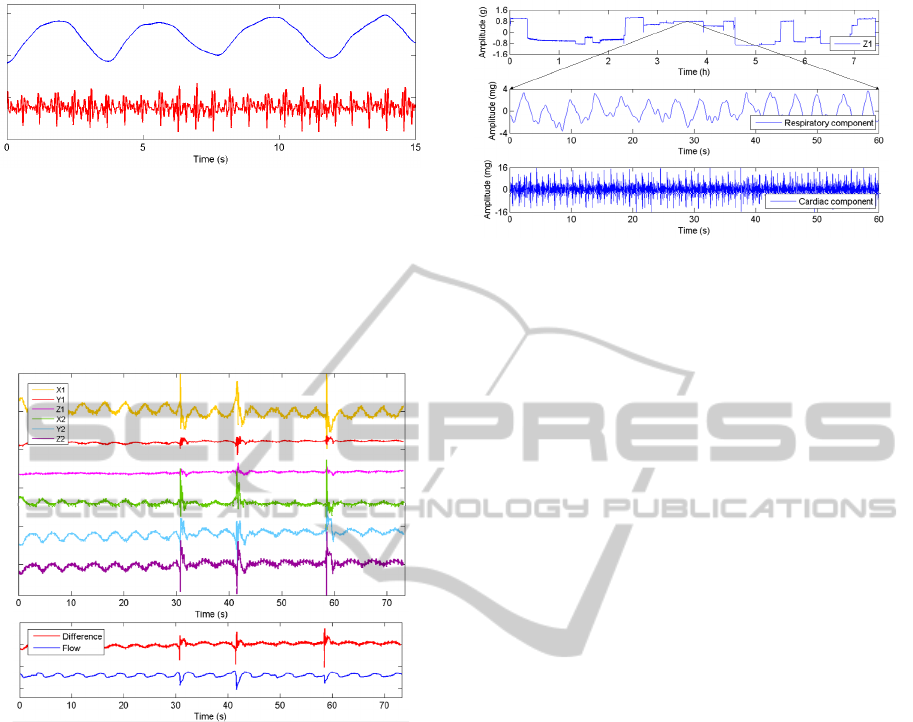
Figure 4: 15 s recording of cardiorespiratory activity by
means of an accelerometer in an awake subject at rest.
Traces derive from the Y axis of an accelerometer
positioned on the chest wall projection of the cardiac area
and were digitally filtered (see methods) to obtain the
signals of the ongoing respiratory (in blue) and cardiac
activities (in red). Traces are in arbitrary units and were
similarly amplified.
Figure 5: Upper panel: accelerometric recordings of three
single cough efforts obtained by means of the
accelerometer pair: X, Y and Z are the signals originating
from each of the two tri-axial accelerometers. Traces are
in arbitrary units and displayed at different levels to
facilitate comparisons of their morphology. Lower panel:
morphological comparison of spirometric flow (in blue,
cough expulsions marked by downward swings) and
accelerometer signal difference (in red, expulsions marked
by upward swings) during three single cough efforts.
Signals were differently amplified to facilitate
morphological comparison.
each cough event can be appreciated in terms of the
magnitude of the corresponding spirometric flow
signal. At the present stage of development it seems
likely that the accelerometric signals are suitable to
detect cough appearance but not to quantify its
intensity.
Long term accelerometric recordings of
cardiorespiratory activity and postural behaviour
during sleep were successfully accomplished in all
of the nine normal subjects. Respiratory and cardiac
activity
could be recorded only during stable body
Figure 6: Upper panel: 7.5 h recording of cardiorespiratory
and postural activities during sleep in one representative
subject using an accelerometer. The signal of respiratory
activity was derived from a single axis of one of the two
accelerometers (see methods). Sudden variations of signal
mark the changes in body position that occurred
throughout the recording period. Middle and lower panels:
60 s - time window of respiratory and cardiac activities
obtained from the upper panel tracing.
posture; in fact, during changes in body position, the
signal related to general movement masked the
cardiorespiratory signal (figure 6, upper panel). As a
consequence, the device allowed us to accurately
detect the number of postural adjustments that
occurred during the recording period.
4 DISCUSSION
This study shows that the use of an accelerometer
pair positioned on the chest wall seems to be suitable
for non-invasive detection of cardiorespiratory and
postural behaviours, both during wakefulness and
sleep; furthermore, the device may also be useful for
recording the number and the motor pattern of cough
events.
Any signal derived from each of the sensors can
provide information about the frequency of cardiac
activity. The latter is displayed as a sequence of
peaks corresponding to the systole. Further analyses
revealed that the Z axis is the most sensitive one in
picking vibrations of the chest wall caused by heart
activity, especially when the sensor is positioned on
the chest wall area corresponding to heart projection.
Qualitative analysis also revealed that the signals
obtained by the two accelerometric sensors,
particularly the difference signal, strictly matched
with the respiratory thoracic movements. The
preliminary results seem also to suggest that not
only respiratory frequency, but also the amplitude of
each breath, is correctly detected by the
accelerometer pair. Indeed, values of respiratory rate
obtained by spirometry and accelerometers were
A PROPOSAL OF A NOVEL CARDIORESPIRATORY LONG-TERM MONITORING DEVICE
41

identical, in keeping with previous findings
(Reinvuo, 2006) and (Hung, 2008). However, this
study is the first to show that voluntary changes in
the depth of breathing can also be accurately
detected by the device.
This study is also the first to demonstrate that the
motor pattern of voluntary cough can successfully be
distinguished from that of normal breathing by
means of an accelerometer pair. In addition, the
accelerometric pattern of cough was fairly coherent
with that recorded spirometrically, and revealed high
frequency components due to speed of the expulsive
activity and related chest wall vibrations. However,
inaccuracies still exist as far as the accelerometric
evaluation of cough intensity is concerned.
Accelerometric long-term recordings of
cardiorespiratory activity during sleep in normal
subjects provide some advantages compared with
standard techniques. Although not formally tested
here, it seems obvious that our device offers better
portability than the conventional ones and that the
possibility of simultaneous recording of body
posture may represent an important tool in the
evaluation of sleep disturbances.
It could be argued that, in order to monitor
cardiorespiratory activity, the use of an
accelerometer-based device is somewhat limited by
the interfering signals of body motion, especially
during daily activities. Whilst we acknowledge that
this limitation may exist at least to some extent, we
also feel that the recording a cardiorespiratory signal
“disturbed” by that originating from body
movements is “per se” of clinical usefulness. It may
be inferred that patients with respiratory
disturbances must present a ratio of resting-to-
activity time that is inversely related to the general
clinical condition. Therefore, an increase in the
above time ratio could be interpreted as an index of
a deteriorating clinical condition. In addition, in
patients with respiratory diseases, the detection of an
increase in cardiac and respiratory activity at rest
could also point to an increased metabolic demand
such as in the event of a respiratory exacerbation.
5 CONCLUSIONS
Simultaneous recordings of respiratory movements,
heart rate and body position can easily be
accomplished by using pairs of tri-axial
accelerometers; these devices seem to be also
suitable for the detection of the motor pattern of
cough.
The device can be employed for daytime and
nocturnal long-term monitoring thanks to its small
dimensions, small weight and easy positioning of
sensors on the chest wall, that warrant non-invasive
measurements. It could be employed in the diagnosis
of sleep disturbances such as the sleep apnoea
syndrome, or in the monitoring of the elderly. Even
at the present stage of development, the device
presented here appears to be ready for accurate and
reliable long-term sleep studies. Being easily
portable and not bulky, the device seems to be
particularly suitable for sleep studies in the domestic
environment.
REFERENCES
Tobin, M. J., Chadha, T. S., Jenouri, G., Birch, S. J.,
Gazeroglu, H. B., Sackner, M. A., 1983. Breathing
patterns. 1. Normal subjects. In Chest; 84 (2): 202-5.
Pauwels, R. A., Buist, A. S., Calverley, P. M., Jenkins, C.
R., Hurd, S. S., 2001. Global strategy for the
diagnosis, management, and prevention of chronic
obstructive pulmonary disease. NHLBI/WHO Global
Initiative for Chronic Obstructive Lung Disease
(GOLD) Workshop summary. In Am J Respir Crit
Care Med; 163(5):1256-76.
Britton, M., 2003. The burden of COPD in the U.K.:
results from the Confronting COPD survey. In Respir
Med; 97 Suppl C:S71-9.
Panossian, L. A., Avidan, A. Y., 2009. Review of sleep
disorders. In Med Clin North Am.; 93(2):407-25.
Redline, S., Young, T., 1993. Epidemiology and natural
history of obstructive sleep apnea. In Ear Nose Throat
J; 72(1):20-1, 24-6.
Deegan, P. C., McNicholas, W. T., 1995. Pathophysiology
of obstructive sleep apnoea. In Eur Respir
J;8(7):1161-78.
McNicholas, W. T., 2008. Diagnosis of obstructive sleep
apnea in adults. In Proc Am Thorac Soc;5(2):154-60.
Hurst, J. R., Wedzicha, J. A., 2009. Management and pre-
vention of chronic obstructive pulmonary disease
exacerbations: a state of the art review. In BMC Med;7:40.
Perez, W., Tobin, M. J., 1985. Separation of factors
responsible for change in breathing pattern induced by
instrumentation. In J Appl Physiol; 59 (5):1515-20.
Que, C. L., Kolmaga, C., Durand, L. G., Kelly, S. M.,
Macklem, P. T., 2002. Phonospirometry for non-
invasive measurement of ventilation: methodology and
preliminary results. In J Appl Physiol;93(4):1515-26.
Reinvuo, T., Hannula, M., Sorvoja, H., Alasaarela, E.,
Myllyla, R., 2006. Measurement of respiratory rate
with high-resolution accelerometer and emfit pressure
sensor. In Sensors Applications Symposium, 2006.
Proceedings of the 2006 IEEE , vol., no., pp. 192- 195,
Hung, P. D., Bonnet, S., Guillemaud, R., Castelli, E., Yen,
P. T. N., 2008. Estimation of respiratory waveform
using an accelerometer. In Biomedical Imaging: From
Nano to Macro, 2008. ISBI 2008. 5th IEEE
International Symposium on, vol., no., pp.1493-1496,
14-17 May
BIOSIGNALS 2011 - International Conference on Bio-inspired Systems and Signal Processing
42
