
BONE QUALITY TESTING DURING DENTAL IMPLANT
SURGERY
A Novel Device for Intraoperative Compressive Testing of Alveolar Bone
Werner Winter
Department of Mechanical Engineering, University of Erlangen-Nuremberg, Egerlandstrasse 5, 91058 Erlangen, Germany
Tim Krafft
Oral and Maxillofacial Surgeon, Woerthstrasse 7, 92637 Weiden, Germany
Matthias Karl
Department of Prosthodontics, University of Erlangen-Nuremberg, Glueckstrasse 11, 91054 Erlangen, Germany
Keywords: Bone quality, Compressive testing, Dental implant surgery.
Abstract: Based on theoretical considerations, a mathematical equation was set up describing a correlation between
density and mechanical properties of both, cortical and trabecular bone. Simulating the clinical situation of
dental implant placement, finite element analysis was applied to test the validity of compressive testing of
alveolar bone following implant site preparation. As a final step, a loading device was constructed
accordingly and tested in human cadaver bone.
1 INTRODUCTION
Precise evaluation of alveolar bone quality is a
prerequisite for successful implant therapy as dental
implants are subject to masticatory loads of varying
magnitude (Brunski, 1988). The type and
architecture of bone are known to influence its load
bearing capacity, and it has been shown that
implants placed in poor quality bone have higher
failure rates (Norton and Gamble, 2001). In clinical
reality, bone quality does affect treatment planning
and the choice of loading protocols for a specific
patient.
This topic has been addressed by numerous
authors and various techniques for evaluating bone
quality have been described including preoperative
radiographs, subjective hand feeling during drilling
(Alsaadi, 2007; Trisi, 1999; Shapurian, 2006),
implant insertion torque (Beer, 2003; Friberg,
1999a; Johansson, 2004), different forms of
computed tomography (Aranyarachkul, 2005; Ikumi,
2005; Lagravere, 2006; Lindh, 1996) as well as
measurement systems for the determination of
primary implant stability (Friberg, 1999b; Nkenke,
2003; Al-Nawas, 2006) such as the Periotest
®
(Medizintechnik Gulden, Modautal, Germany) and
Osstell
®
(Osstell AB, Gothenburg, Sweden) device
(Meredith, 1998; Schulte, 1992; Aparicio, 2006).
However, a recent literature review pointed out
that a single objective evaluation method for bone
quality is not available so far and that there is only
sparse evidence for the efficacy of clinical methods
to assess jawbone tissue prior to and during
endosseous dental implant placement (Ribeiro-Rotta,
2007).
As compressive testing of human bone
specimens has been successfully used in
experimental research (Giesen, 2003; Giesen, 2004),
it was planned to develop a system capable of
conducting compressive tests on human alveolar
bone during dental implant surgery (Figure 1).
Therefore, the purpose of this study was to
design a method for the non-destructive
determination of bone quality following implant site
preparation. Using mathematical considerations and
finite element analyses it has been clarified which
140
Winter W., Krafft T. and Karl M..
BONE QUALITY TESTING DURING DENTAL IMPLANT SURGERY - A Novel Device for Intraoperative Compressive Testing of Alveolar Bone.
DOI: 10.5220/0003132601400145
In Proceedings of the International Conference on Biomedical Electronics and Devices (BIODEVICES-2011), pages 140-145
ISBN: 978-989-8425-37-9
Copyright
c
2011 SCITEPRESS (Science and Technology Publications, Lda.)
mechanical parameters have to be determined in
order to obtain information on the elastic properties
of bone at a specific site. Based on these findings, a
clinically applicable device for bone quality testing
was fabricated and used for preliminary testing in
human cadaver bone.
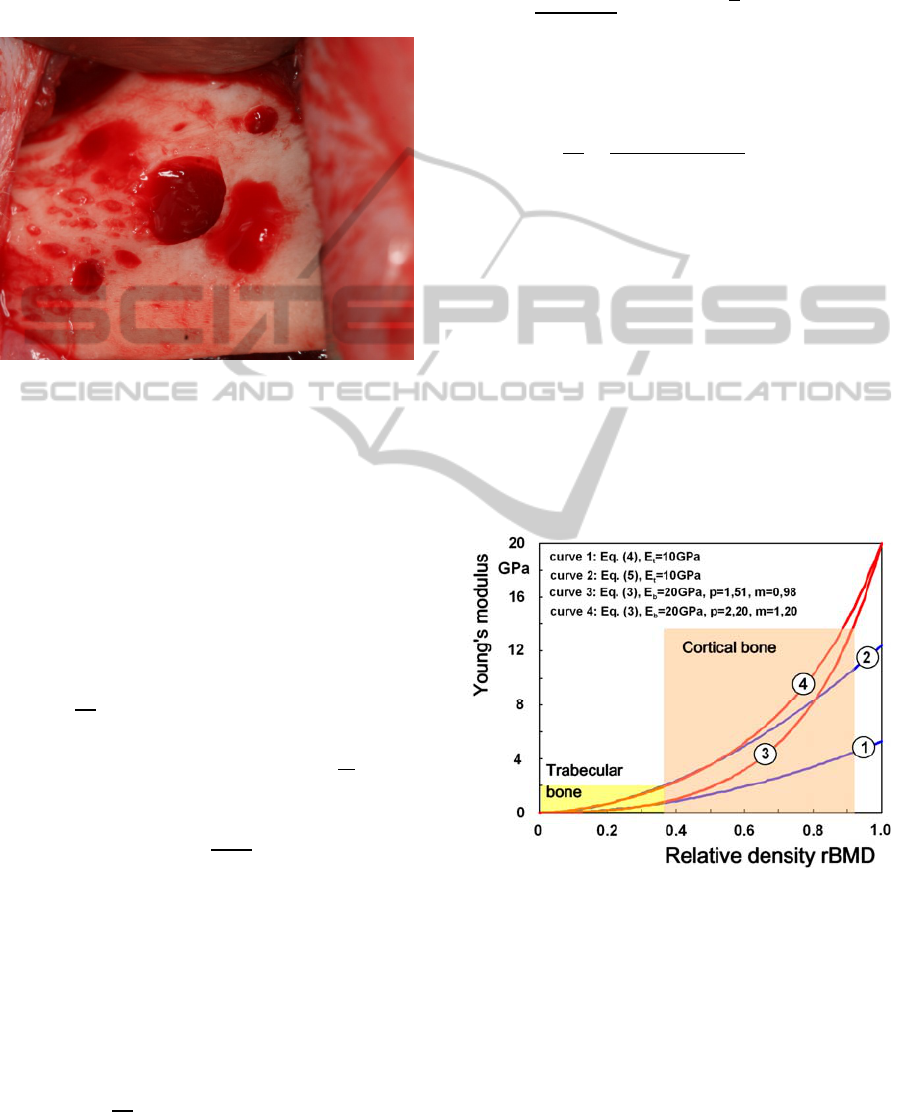
Figure 1: Clinical situation during dental implant surgery
after preparation of an implant site using a series of twist
drills. Note: Areas of decortication surrounding the
implant site provide blood supply for local bone
augmentation in this case.
2 STUDY PARTS AND FINDINGS
2.1 Theoretical Considerations
G Given the non-homogeneous structure of both
cortical and trabecular bone comprising hard tissue
and bone marrow, volumetric bone mineral density
=
(
: bone mass,
: bone volume)
appears to be inadequate for describing bone.
Apparent bone mineral density =
(: total volume with bone mass and marrow) which
takes marrow space into account and relative bone
mineral density =
appear to be more
appropriate.
For biomechanical considerations, bone can be
described as a cellular structure or as a porous
structure with a specific distribution of hollow
spaces. In either situation, can be described
as a function of geometric parameters describing
unit cells.
For an analytical model, the relative elastic
modulus for cellular structures may be described as
= ()
(1)
with E standing for the apparent elastic modulus and
b and n representing material characteristics. E can
also be described as a function of apparent density
=
()
()
=b ()
.
(2)
In order to be able to reflect rBMD values ranging
from 0 to 1, a unifying equation was set up (Winter,
2008)
=
()
(3 − 2 )
(3)
where p and m reflect material parameters. With the
given equation it was possible to approximate values
for trabecular bone reported by Yang and coworkers
(Yang et al, 1999)
= 528
∅
.
(4)
and
= 1240
∅
.
(5)
with ∅≡ being the fraction of bone and
= 10 being the tissue elastic modulus (Yang
et al, 1999).
In Fig. 2 a comparison of Eq. (3) with Eq. (4) and
Eq. (5) is shown over the whole range of the relative
bone mineral density .
Figure 2: Comparison of Young’s modulus over the whole
range of relative bone mineral density. Bone quality can
be characterized by the Young’s modulus of bone or bone
stiffness.
2.2 Design of a Device for Bone Quality
Testing
A three-dimensional finite element model
(MSC.Nastran®, MSC Software Partner Solutions,
Marburg, Germany) representing a 25mm long
BONE QUALITY TESTING DURING DENTAL IMPLANT SURGERY - A Novel Device for Intraoperative
Compressive Testing of Alveolar Bone
141
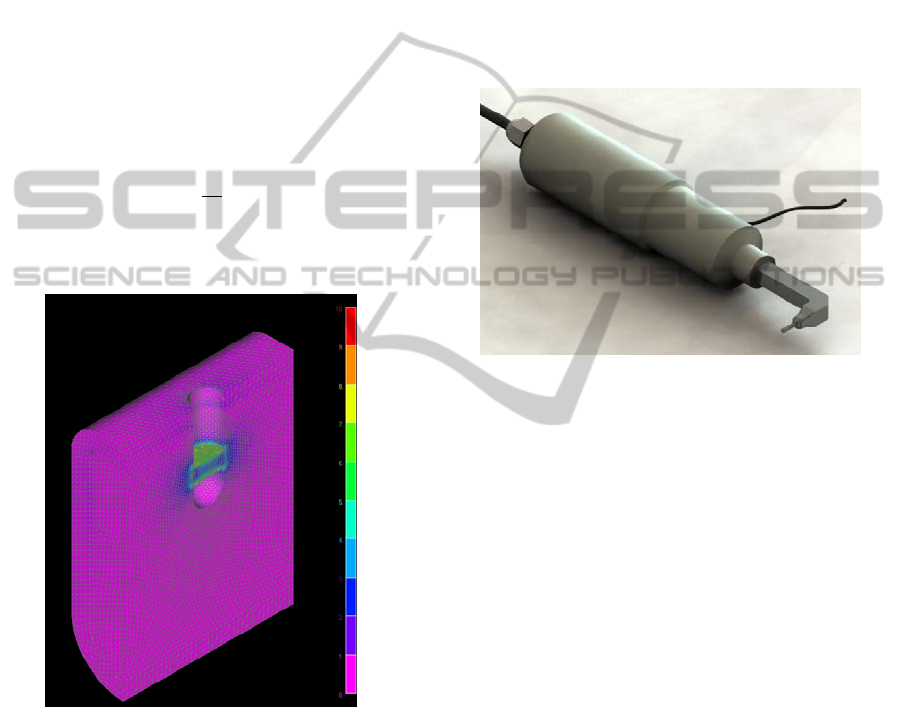
segment of a human mandible with an implant
socket (diameter: 3.5 mm; length: 11mm) was
generated (Figure 3). A peripheral layer (2mm
thickness) and a central layer were created to model
bone using tetrahedral elements. Bone was
considered as an isotropic material with an elastic
modulus of 20GPa in the cortical area and values of
either 1GPa or 3GPa for trabecular bone. Poisson’s
ratio was set to 0.3 for both, cortical and trabecular
bone and the free boundaries (anterior and posterior
segment borders) were fixed. A loading device
3.5mm in diameter was positioned in the trabecular
part of the implant socket and expanded by applying
thermal expansion until a diameter of 3.510 mm was
reached while the resulting pressure values p
1
were
recorded and used to calculate an elastic modulus E
1
applying the equation
=
(6)
with E
0
and p
0
standing for the calibration of the
device.
Figure 3: Finite element model used for validating
intraoperative compressive testing for the objective
classification of alveolar bone quality (scale: MPa). A
loading device was placed in a readily prepared implant
socket and the diameter of the device expanded. The stress
levels measured were used to calculate bone’s elastic
modulus in this area.
The values obtained from the simulation yielded
940MPa and 955MPa for two different finite
elements. Depending on the element considered,
maximum deviations of 6% between pre-set values
for the elastic modulus of bone and values derived
from the simulation were found.
2.3 Fabrication of a Bone Quality
Testing Device
An apparatus was constructed based on a metal
cylinder with a diameter of 3.50 mm which was split
into six segments. The cylinder could be expanded
gradually while the actual force needed was
recorded (Figure 4, Figure 5). This sensor could be
placed into sockets prepared for the placement of
cylindrically shaped dental implants and the
diameter increased to 3.52mm and 3.57mm for
measurements in the cortical and trabecular part of
the osteotomy.
Figure 4: Total view of the bone quality testing device
which is hand-held, motor driven and suitable for intraoral
measurements.
2.4 In vitro Testing in Human Cadaver
Bone
Segments of embalmed human mandibles and
maxillas were obtained from the Institute of
Anatomy, University of Erlangen-Nuremberg and
subject to cone beam computed tomography (CBCT)
scans (3D Accuitomo, J.Morita Europe GmbH,
Dietzenbach, Germany). The sites for implant
placement (number of sites: 110) as determined by
CBCT were classified according to the region in the
oral cavity (Maxilla / Mandible; Anterior /
Posterior).
BIODEVICES 2011 - International Conference on Biomedical Electronics and Devices
142

Table 1: Mean values and standard deviations for all measurements conducted in human cadaver bone.
Drilling
resistance
Bone quality
testing device -
cortical bone
Bone quality
testing device -
trabecular bone
Implant
insertion torque
Resonance
frequency
analysis
Maxilla
anterior
2.83 (0.72) 21.08 (8.68) 14.33 (6.87)
16.68
(11.66)
63.75
(12.99)
Maxilla
posterior
2.85 (0.80) 14.01 (7.19) 14.70 (8.37) 9.33 (5.31)
64.92
(11.23)
Mandible
anterior
1.34 (0.70)
34.65
(18.39)
30.55
(26.71)
29.72
(13.27)
75.39 (6.31)
Mandible
posterior
1.60 (0.72)
43.66
(36.45)
21.21
(20.63)
30.53
(12.18)
78.46 (6.21)
Table 2: Pearson correlation coefficients for all combinations of measurements conducted in human cadaver bone.
Drilling
resistance
Bone quality
testing device -
cortical bone
Bone quality
testing device -
trabecular bone
Implant
insertion torque
Resonance
frequency
analysis
Drilling
resistance
1.0000 -0.4384 -0.3474 -0.6940 -0.4740
Bone quality
testing device -
cortical bone
1.0000 0.1712 0.4672 0.3321
Bone quality
testing device -
trabecular bone
1.0000 0.0621 0.1090
Implant
insertion torque
1.0000 0.4619
Resonance
frequency
analysis
1.0000
Figure 5: Sensing element of the bone quality testing
device consisting of a cylinder which is split into six
segments. The diameter of the cylinder can be increased
and the forces needed are recorded.
A socket 3.5mm in diameter and 11mm in length
was prepared for the placement of a screw-shaped
cylindrical implant with a diameter of 4.1mm and
10mm bone sink depth (Straumann Standard Plus
Implant; Institut Straumann AG, Basel, Switzerland)
in each site. The implant position was marked with a
round burr and a set of twist drills 2.2mm, 2.8mm
and 3.5mm in diameter was used in combination
with a surgical motor (KaVo INTRAsurg 1000;
KaVo Dental GmbH, Biberach, Germany) to create
standardized implant beds. During implant bed
preparation, the surgeon subjectively rated bone
quality according to the Lekholm and Zarb
classification system (Lekholm and Zarb, 1985).
Compressive testing using the bone quality testing
device was conducted in the areas of cortical and
trabecular bone (Figure 6). The sensor was opened
to 3.57mm in the cortical area and 3.52mm in the
trabecular area of each socket The forces needed to
open the sensor were recorded in N. Implants were
then installed using the surgical motor (KaVo
INTRAsurg 1000; KaVo Dental GmbH, Biberach,
Germany) measuring the maximum torque needed to
insert the implants. Primary implant stability was
determined by means of resonance frequency
measurements (Osstell mentor, Osstell AB,
Gothenburg, Sweden). For statistical analysis,
Pearson correlation coefficients were calculated for
all combinations of parameters.
BONE QUALITY TESTING DURING DENTAL IMPLANT SURGERY - A Novel Device for Intraoperative
Compressive Testing of Alveolar Bone
143

Figure 6: Application of the bone quality testing device in
a polyurethane foam model. Following implant site
preparation, the sensing element is inserted in the
osteotomy and opened gradually both in the cervical and
apical part of the socket while the force needed for
opening the sensor is measured.
The mean values and standard deviations for all
measurements conducted are given in Table 1.
Consistent with clinical knowledge, for all
parameters greater values were recorded in the
mandible as compared to the maxilla. Good
correlations between the different measuring
techniques were found.
3 DISCUSSION
It has been shown that the newly designed device
can be used for the objective classification of human
alveolar bone based on intraoperative compressive
testing. The values obtained are consistent with
already established measurement techniques either
evaluating bone quality or primary implant stability.
The major advantage of the system proposed is that
it can be applied independent from any specific
implant system thereby allowing for objective
comparisons. As the implants have not yet been
installed when the bone quality testing device is
applied, the surgeon still has the choice to modify
the treatment plan e.g. by selecting a tapered instead
of a parallel walled implant in order to achieve
greater primary stability. Based on the values
obtained from the bone quality testing device, a
decision can also be made with more confidence as
to when a specific implant can be loaded with a
certain type of superstructure. Following preclinical
testing in animals, further prospective clinical trials
are needed for establishing and verifying the
diagnostic value of the bone quality testing device.
The ultimate goal of the development should be to
establish threshold values on when a dental implant
can be loaded immediately.
REFERENCES
Al-Nawas, B., Wagner, W., Grötz, K. A. 2006. Insertion
torque and resonance frequency analysis of dental
implant systems in an animal model with loaded
implants. Int J Oral Maxillofac Implants 21:726-732.
Alsaadi, G., Quirynen, M., Michiels, K., Jacobs, R., van
Steenberghe, D. 2007. A biomechanical assessment of
the relation between the oral implant stability at
insertion and subjective bone quality assessment. J
Clin Periodontol 34:359-366.
Aparicio, C., Lang, N. P., Rangert, B. 2006. Validity and
clinical significance of biomechanical testing of
implant / bone interface. Clin Oral Implants Res 17
Suppl 2: 2-7.
Aranyarachkul, P., Caruso, J., Gantes, B., Schulz, E.,
Riggs, M., Dus, I. et al. 2005. Bone density
assessments of dental implant sites: 2. Quantitative
cone-beam computerized tomography. Int J Oral
Maxillofac Implants 20:416-424.
Beer, A., Gahleitner, A., Holm, A., Tschabitscher, M.,
Homolka, P. 2003. Correlation of insertion torques
with bone mineral density from dental quantitative CT
in the mandible. Clin Oral Implants Res 14:616-620.
Brunski, J. B. 1988. Biomechanics of oral implants: future
research directions. J Dent Educ 52:775-787.
Friberg, B., Sennerby, L., Grondahl, K., Bergstrom, C.,
Back, T., Lekholm, U. 1999a. On cutting torque
measurements during implant placement: a 3-year
clinical prospective study. Clin Implant Dent Relat
Res 1:75-83.
Friberg, B., Sennerby, L., Meredith, N., Lekholm, U.
1999b. A comparison between cutting torque and
resonance frequency measurements of maxillary
implants. A 20-month clinical study. Int J Oral
Maxillofac Surg 28:297-303.
Giesen, E. B., Ding, M., Dalstra, M., van Eijden, T. M.
2003. Reduced mechanical load decreases the density.
stiffness. and strength of cancellous bone of the
mandibular condyle. Clin Biomech 18:358-363.
Giesen, E. B., Ding, M., Dalstra, M., van Eijden, T. M.
2004. Changed morphology and mechanical properties
of cancellous bone in the mandibular condyles of
edentate people. J Dent Res 83:255-259.
Ikumi, N., Tsutsumi, S. 2005. Assessment of correlation
between computerized tomography values of the bone
and cutting torque val-ues at implant placement: a
clinical study. Int J Oral Maxillofac Implants 20:253-
260.
Johansson, B., Back, T., Hirsch, J. M. 2004. Cutting
torque measurements in conjunction with implant
placement in grafted and nongrafted maxillas as an
objective evaluation of bone density: a possible
method for identifying early implant failures? Clin
Implant Dent Relat Res 6:9-15.
BIODEVICES 2011 - International Conference on Biomedical Electronics and Devices
144

Lagravere, M. O., Fang, Y., Carey, J., Toogood, R.W.,
Packota, G. V., Major, P. W. 2006. Density
conversion factor determined using a cone-beam
computed tomography unit NewTom QR-DVT 9000.
Dentomaxillofac Radiol 35:407-409.
Lekholm, U., Zarb, G. A. 1985. Patient selection and
preparation. In Branemark, P-I., Zarb, G.A. and
Albrektsson, T. (eds): Tissue Integrated Prostheses:
Osseointegration in Clinical Dentistry. Chicago,
Quintessence Publishing, 1985, pp 199-209.
Lindh, C., Nilsson, M., Klinge, B., Petersson, A. 1996.
Quantitative computed tomography of trabecular bone
in the mandible. Dentomaxillofac Radiol 25:146-150.
Meredith, N. 1998. A review of nondestructive test
methods and their application to measure the stability
and osseointegration of bone anchored endosseous
implants. Crit Rev Biomed Eng 26:275-291.
Nkenke, E., Hahn, M., Weinzierl, K., Radespiel-Troger,
M., Neukam, F. W., Engelke, K. 2003. Implant
stability and histomorphometry: a correlation study in
human cadavers using stepped cylinder implants. Clin
Oral Implants Res 14:601-609.
Norton, M. R., Gamble, C. 2001. Bone classification: an
objective scale of bone density using the computerized
tomography scan. Clin Oral Implants Res 12:79-84.
Ribeiro-Rotta, R.F., Lindh, C., Rohlin, M. 2007. Efficacy
of clinical methods to assess jawbone tissue prior to
and during endosseous dental implant placement: a
systematic literature review. Int J Oral Maxillofac
Implants 22:289-300.
Schulte, W., d'Hoedt, B., Lukas, D., Maunz, M., Steppeler,
M. 1992. Periotest for measuring periodontal
characteristics correlation with periodontal bone loss.
J Periodontal Res 27: 184-190.
Shapurian, T., Damoulis, P. D., Reiser, G. M., Griffin, T.
J., Rand, W.M. 2006. Quantitative evaluation of bone
density using the Hounsfield index. Int J Oral
Maxillofac Implants 21:290-297.
Trisi, P., Rao, W. 1999. Bone classification: clinical-
histomorphometric comparison. Clin Oral Implants
Res 10:1-7.
Winter, W (2008) Bone strength in pure bending: Bearing
of geometric and material properties..Proceedings of
the 2
nd
Conference on Applied Biomechanics Regens-
burg. J. Hammer, M. Nerlich, S. Denkdorfer (eds.),
IOS Press, Amsterdam, Netherland, 230-237.
Yang, G., Kabel, J., van Rietbergen, B., Odgaard, A.,
Huiskes, R., Cowin, S. C. 1999. The anisotropic
Hooke’s law of cancellous bone and wood. J Elast
53.125-146.
BONE QUALITY TESTING DURING DENTAL IMPLANT SURGERY - A Novel Device for Intraoperative
Compressive Testing of Alveolar Bone
145
