
THE IMPORTANCE OF SYSTEM INTEGRATION
IN INTENSIVE CARE UNITS
A Review
Rui Fonseca
1,2
and Pedro Pereira Rodrigues
1,3
1
Faculty of Medicine, University of Porto, Al. Prof. Hernâni Monteiro, 4200-319 Porto, Portugal
2
Faculty of Sciences, University of Porto, Rua do Campo Alegre, s/n, 4169-007 Porto, Portugal
3
LIAAD - INESC Porto, L.A. & CINTESIS - Center for Research in Health
Technologies and Information Systems, Porto, Portugal
Keywords: Intensive Care Units, System integration, Electronic Health Records, Patient outcome.
Abstract: Due to the severity of patients treated in the intensive care units, these units are commonly equipped with a
variety of equipment that is handled by a multidisciplinary team. In order to identify problems, present and
future, clinicians perform periodic assessments that produce huge amount of data, which availability is of
vital importance. This study was performed in order to assess the impact of clinical data centralized in a
clinical information system for inpatients in an intensive care unit, when compared with data disseminated
in different systems. A literature search was conducted on PubMed in order to identify relevant articles
published between 2000 and 2010. From a total of 48 articles, 7 articles were selected for assessment. 2
articles studied the impact of system integration, 4 articles studied the impact of computerized medical
records and 1 article studied both the impact of computerized medical records and system integration. A
centralized clinical information system was proved to have a positive impact for inpatients in an intensive
care unit. These systems allow time savings on vital signs transcription, reduced medication errors, a
quicker access to clinical data and a reduction in prescription errors.
1 INTRODUCTION
The Intensive Care Units (ICU) are a specialized
section of an hospital containing the equipment,
medical and nursing staff, monitoring and life-
support devices necessary to provide continuous
care to patients that are severely ill and medically
unstable.
Due to the severity of the patients, these units are
commonly equipped with mechanical ventilators to
assist breathing, cardiac monitors including
telemetry, external pacemakers and defibrillators,
dialysis equipment for renal problems, equipment
for the constant monitoring of bodily functions, a
web of intravenous lines, feeding tubes, nasogastric
tubes, suction pumps, drains and catheters, and a
wide array of drugs to treat the main conditions. All
of this equipment is handled by a multidisciplinary
team that may be consisted, among others, by
intensivists (clinicians who are specialized in critical
illness care), clinical pharmacists, nutritionists,
nurses, anaesthesiologists, surgeons or emergency
medicine specialists.
In order to identify problems that may arise and
require urgent attention or treatment, clinicians
perform periodic assessments of the patient's cardiac
status, breathing rate, urinary output, and blood
levels. In some cases, patients may need special
requirements for monitoring. That’s the case for
patients who are admitted to the ICU for observation
after surgery. These patients may have catheters
placed to detect hemodynamic changes (blood
pressure changes) or require endotracheal intubation
to help them breath, with the breathing tube
connected to a mechanical ventilator. In order to
perform a correct treatment, the availability of
detailed information is of vital importance.
Physicians have not only to analyze data displayed
by the equipment, but also to analyze laboratory and
radiology results, evaluate patient’s history and
current medication, analyze patient-specific
information such as age, weight and height, analyze
142
Fonseca R. and Rodrigues P..
THE IMPORTANCE OF SYSTEM INTEGRATION IN INTENSIVE CARE UNITS - A Review.
DOI: 10.5220/0003128801420147
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2011), pages 142-147
ISBN: 978-989-8425-34-8
Copyright
c
2011 SCITEPRESS (Science and Technology Publications, Lda.)
warnings of drug interactions and evaluate
diagnoses.
All the mentioned information is extremely
important to physicians in order to prevent mistakes,
to decide the better treatment plan and to perform
acts that allow a better patient outcome. However, in
some cases, the information is distributed by various
information systems, which may result in a huge
time loss when looking for specific data.
The aim of this study is to provide an assessment
of the impact of data centralized in one Clinical
Information System (CIS) for inpatients in an ICU,
when compared with data distributed in different
systems. In order to do so, the following question
should be answered at the end of this study:
Is system integration important in patient
outcome in the ICU, when compared with the
evaluation of data from different systems?
Can computerized medical records in ICU
allow a better decision making?
Can system integration decrease the length of
stay in ICU?
In order to answer these questions, a review will
be performed on the importance of integrating
clinical data provided from equipments, laboratory
and radiology results, administrative inputs and
clinician’s assessments into one centralized system.
This review will be carried out in order to identify
the results of length of stay, mortality rate and
patient outcome and the ability of a better decision
making, which should result in a better overall
treatment.
2 METHODS
A literature search was conducted by one reviewer
in January 2010 on PubMed in order to identify
articles published between January 2000 and
January 2010. The search was performed based on
Medical Subject Heading (MeSH) terms, in order to
identify the importance that system integration or
computerized medical records have on ICU,
influencing patient outcome results.
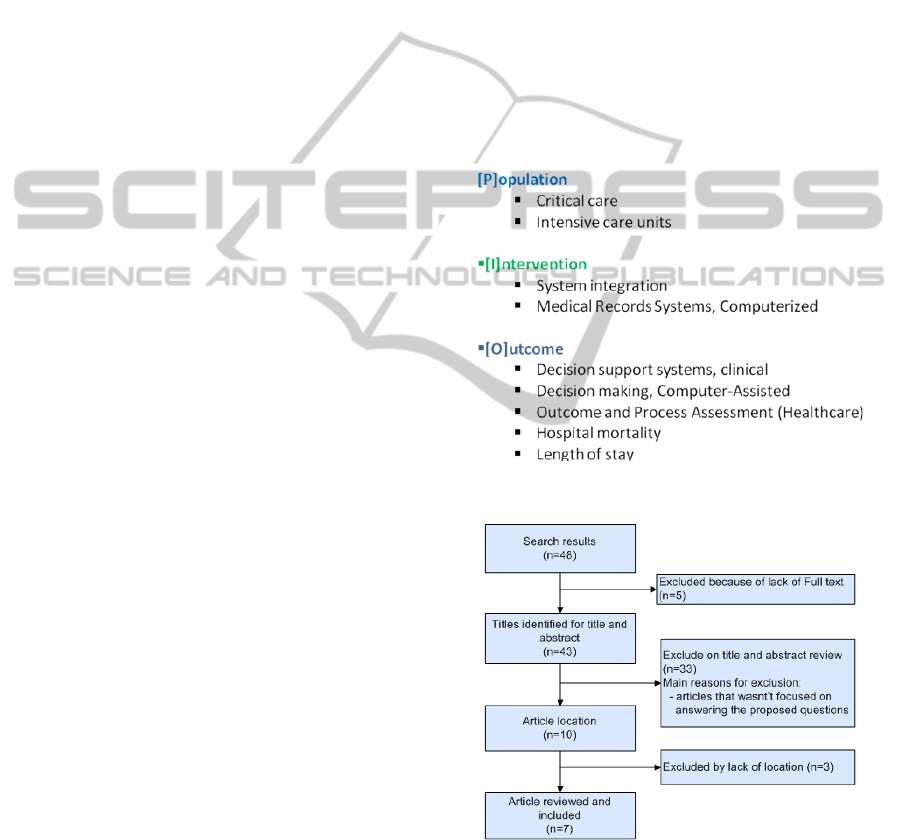
The keywords that were used included ICU in
conjunction with System integration or
Computerized medical records. These terms were
then used in conjunction with Decision support
system or Decision making or Outcome and process
assessment or Hospital mortality or Length of stay
as it can be seen in figure 1.
The inclusion criteria required that the studies:
(1) where based on intensive care units, (2) were
related to system or data integration, (3) evaluated
the patient outcome, (4) were published in English
or Portuguese and (5) where available in Full text.
In order to identify the articles used in the
review, the following selection method was used, as
identified in figure 2. After performing the search on
PubMed database, the availability of full text was
analyzed, resulting in the exclusion of the articles
that weren’t available. At this point, a screening of
the title and abstract was performed, resulting in the
exclusion of articles by lack of the correct content.
Finally, the digital document corresponding to the
article was searched and the articles that couldn’t be
found were excluded. After the identification of the
articles included for revision, its quality was
analyzed through the process of reading and
selection.
Figure 1: Keywords used in the search strategy.
Figure 2: Data search, analysis and selection process.
3 RESULTS
As shown in figure 2, a total of 48 articles were
found in scientific literature (2000-2010) that
THE IMPORTANCE OF SYSTEM INTEGRATION IN INTENSIVE CARE UNITS - A Review
143

examined the outcomes of decision making, decision
support system and patient outcome with the use of
system integration and clinical information systems.
However, the analyses and selection process
outlined in figure 2 guided to an evaluation of the
availability of full text articles, which lead to an
exclusion of 5 articles. The 43 remaining articles
were considered for title/abstract review and a
detailed screening of titles and abstracts resulted in a
selection of 10 articles which were considered for
full text review. After the identification of these
articles, 3 of them could not be located for review,
even though its title and abstract suggested that they
would have been selected for inclusion. Performing
this process led to an inclusion of 7 articles. One of
these articles is a narrative review that focuses on
the benefit of using Computerized Physician Order
Entry (CPOE) in performing a better patient
outcome (Rothschild, 2004).
As shown in table 1, most of the selected articles
assessed the evaluation of the impact of
computerized medical record systems (5 articles)
while only a few number of articles assessed the
impact of system integration (3 articles). All the
articles that studied the impact of the system
integration also evaluated the outcome of
computerized decision making. In the set of articles
that studied the impact of computerized medical
records were found articles that analyzed the
outcome on: length of stay (1 article), computerized
decision making (3 articles) and outcome and
process assessment (2 articles).
The studies can be classified in three groups of
interest: computerized medical records with outcome
and process assessment; computerized medical
records with computerized decision making; system
integration with computerized decision making. One
of the articles (Reina-Tosina et al., 2002) evaluated
simultaneously the effect of system integration and
computerized medical records with computerized
decision making.
3.1 Computerized Medical
Records and Outcome
and Process Assessment
(Ward, Snyder, Ross, Haze, Levy , 2004) conducted
a randomized analysis in order to evaluate the
correctness and completeness of the use of a CIS,
when compared with direct and indirect methods of
measuring critical care outcomes. Medication
administration is used to analyze the medication that
is being administered to the patients. The CIS was
implemented in an ICU where medications are
dispensed by automated machines. Since the CIS
records information about the patient, time, and
medication dosage, a review of this information can
be done at any time, allowing physicians to perform
a better decision making. However, within the
analysis period, 411 medications were administered
but only 341 were logged in the CIS.
(Donati et al., 2008) conducted a before and after
study in a European Medical and Surgical ICU, in
order to evaluate the impact of a CIS in an ICU. The
study focused on the comparison of the time spent
charting on paper and on the CIS by physicians and
nurses. The activities evaluated were: transcription
of vital signs, physician therapeutic orders and
laboratory data and time spent for computing fluid
balance and scores. The time spent on performing
one of these activities was measured separately and,
when using the CIS, the time spent for the same
activities was measured by the difference between
the login and the logout. All the measure was done
by a person not involved in the study. The time spent
charting on paper and on CIS was highly decreased
(3 ± 2 minutes/day versus 37 ± 7 minutes/day
respectively, P < 0.001). In some cases, such as fluid
balance and exam transcription, the time was
reduced to 0 minutes.
3.2 Computerized Medical
Records and Computerized
Decision Making
(Menke, Broner, Campbell, McKissick,
Edwards-Beckett, 2001) conducted a before and
after comparison study in a Paediatrics ICU in order
to identify the impact of a clinical decision system
on decision making and overall patient outcome.
The study was performed by an independent
observer that measured the time spent in direct
patient care, number of medication errors,
medication’s delay evaluation and speed of clinical
decision-making. The previous measures were done
before and after the implementation of a centralized
CIS, through the observation of the clinicians. After
the implementation of the CIS, no significant
difference devoted to direct patient care was
identified. However, the number of medication
errors and delay decreased substantially and there
was an increase in the speed of clinical decision-
making due to the availability of data provided from
laboratory and vital signs. There was an
improvement in data access due to the availability of
data on several computers. The rapid access to
previous medication, laboratory and vital signs data
also allowed a better patient outcome.
HEALTHINF 2011 - International Conference on Health Informatics
144

Table 1: Details for studies found for the outcomes System integration and Electronic Health Records in an ICU. The
numbers in brackets represent the articles, as described at the bottom of this table.
System integration Electronic Health Records
Number of studies
3 (43%)
[2] [4] [6]
5 (71%)
[1] [3] [4] [5] [7]
Year of publication
2008 1
2004 2
2003 2
2002 1 1
2001 1
Study outcome
Outcome and Process Assessment 2
Length of Stay 1
Computerized decision making 3 3
Study design
Before and after 1
[6]
2
[1] [3]
Review 1
[5]
Non Randomized control trial 2
[2] [4]
2
[4] [7]
Study population
Not specified 2
[2] [4]
3
[1] [4] [7]
Paediatric/Neonate 1
[6]
1
[3]
Not applicable 1
[5]
[1] Donati et al., 2008; [2] Kowe and Burgess, 2003; [3] Menke et al., 2001; [4] Reina-Tosina et al., 2002;
[5] Rothschild, 2004; [6] Shin, Huh, Lee and Kim, 2003; [7] Ward et al., 2004
(Rothschild, 2004) conducted a review in order to
assess the effects of CPOE on patient outcome in
both general and critical care settings. The
performed review included only randomized
controlled trials. Study design evaluated not only
before and after comparisons, but also time series
(off-on-off-on). The outcomes measured included
clinical and surrogate outcomes. Clinical outcomes
are mortality, morbidities, adverse events and length
of stay. Surrogate outcomes include medical errors,
costs or charges and intermediate outcomes (e.g.,
laboratory results) with well-established connections
to the clinical outcomes of interest such as clinical
guideline compliance or the use of institutional best
practices (Rothschild, 2004). In this review, the
author identified three areas of interest: CPOE on
medication prescribing area; the effects of CPOE on
diagnostic test ordering and test result management;
the effects of CPOE on injury prevention. In all
areas of interest, the author identified an overall
increase of patient outcome when a CPOE is used in
ICU.
(Reina-Tosina et al., 2002) conducted a study in
Europe in order to provide methodological issues
and technological solutions for an integrated system
that allows the management of a hospital unit. This
study presents a proposal for the development of a
clinical information system that allows the
integration of all the information produced within a
burn ICU. According to the author, time efficiency
has grown increasingly.
3.3 System Integration
and Computerized
Decision Making
(Kowe and Bugess, 2003) conducted a
Non-Randomized Controlled Trial study on a
neonatal ICU in order to demonstrate the importance
of continuous monitoring by presenting a prototype.
The prototype developed is a system that provides
automatic and unattended monitoring of many of the
electrophysiological parameters that were shown to
be useful. The purpose of this prototype is to allow
untrained neurophysiologists to identify abnormal
trends easier. It consists in an integrated bedside
monitor that continuously monitors the function of
the patient’s central nervous system in a predefined
interval, as well as monitors cardiac and respiratory
parameters (Shin, Huh, Lee and Kim, 2003)
THE IMPORTANCE OF SYSTEM INTEGRATION IN INTENSIVE CARE UNITS - A Review
145

Table 2: Relationship between Outcomes and Interventions of studies.
Author Year
Outcome Intervention
OPA LOS DM SI EHR
Donati et al. 2008 x x
Kowe and Bugess 2003 x x
Menke et al. 2001 x x
Reina-Tosina et al. 2002 x x x
Rothschild 2004 x x
Shin, Huh, Lee and Kim 2003 x x
Ward et al. 2004 x x x
OPA:Outcome and Process Assessment; LOS:Length of stay; DM:Decision Making; SI:System Integration; EHR:Electronic Health Record
conducted a study in a neonatal ICU in order to help
managing and monitoring conditions within
incubators in the infant ICU using the hospital
network. In order to accomplish this goal, a pilot
system that monitors the humidity and temperature
of infant incubators was developed. This system is
connected to a centralized supervisory monitoring
system, allowing clinicians to monitor the overall
state of the inpatients of the ICU in one single
system. As a result, the author identified that a
centralized control centre in a neonatal ICU
performs a primary supervision, allowing for an
immediate response. However, the overall
supervision shouldn’t rely only on this system.
4 DISCUSSION
This study was designed with particular attention to
evaluate the importance of centralization of data
provided from equipment, such as vital signs and
life-support monitoring, and from other information
systems within the ICU, like radiology and
laboratory results, in order to access the results of
patient outcome, such as mortality rate, length of
stay and overall quality of care. From a total of 7
articles identified, 4 articles studied the importance
of computerized medical records, 2 articles studied
the importance of system integration and 1 articled
studied both the importance of system integration
and computerized medical records. A few limitations
can be found in this review: the search was only
based on MeSH terms; only one database – PubMed
– was used to perform the search.
From the analysis of the searched studies, this is
the first review exclusively dedicated to evaluating
such case-control study. However, one study was
found mentioning the importance of such integration
(Donati et al., 2008). In this study, the author was
focused on comparing the importance of a CIS in
order to reduce the time spent on charting, while
compared to paper based records. As mentioned by
the author, their system is able to “retrieve
automatically data from physiologic monitoring, IV
pumps, ventilators and moreover interfaces with a
blood gas analyzer and utilizes web browser
technology to provide users with access to chemistry
and microbiology labs, radiology systems and
intranet sites” (Donati et al., 2008), but the
evaluation of the relevance of this integration was
not part of the study. Despite of identifying the
reduction of time in charting by all the clinicians
inside the ICU, this study didn’t evaluate if the time
was correctly applied to patient’s treatment, which
could have been done evaluating patient outcome.
The importance of system integration was
mentioned through the use of continuous monitoring
systems that had the ability to display current status
of the variables in analysis. Both studies were
performed in a neonatal ICU. One of the systems
had the ability to produce alarms when values were
above or below some parameters. Both systems have
the ability of reviewing previously recorded values,
using a web browser with intranet access. While one
of the articles conducted a non-randomized
controlled trial, the other one conducted a before-
after comparison. However, the information was
relevant for this article (Kowe and Burgess, 2003;
Shin, Huh, Lee and Kim, 2003).
The importance of computerized medical records
was mentioned through the use of centralized
systems that allowed a better access to data, such as
vital signs and laboratory results, and an
improvement in prescription. Due to the amount of
data that has to be transcribed for each patient, a
centralized system that registers signals
automatically allows a substantial decrease in
transcription time and errors (Ward et al., 2004;
Donati et al., 2008).
The use of a CIS in order to prescribe medication
can allow a reduction in transcription errors in the
nurse team and gives physicians the ability to easily
review all the prescribed and administrated
prescription, leading to a better decision making.
HEALTHINF 2011 - International Conference on Health Informatics
146

The integration of prescription with laboratory
results and vital signs can allow better decision
making, prevent the prescription of drugs that could
be harmful for the patient and reduce prescription
errors. The centralization of this information into
one single CIS allows the reduction of time on
searching medical records and results, providing
more time for patient care (Ward et al., 2004; Menke
et al., 2001; Rothschild, 2004; Donati et al., 2008).
In order for the integration of information to
produce benefits, it’s necessary to take into account
the availability of systems that can be affected by
viruses, system incompatibilities or computer
downtime (Donati et al., 2008).
The use of a CIS represents a change in the way
clinician’s access to data. Taking this factor into
account, it is necessary to consider the problem
associated to the learning curve that, in an initial
implementation’s phase, may not produce the
expected results (Menke et al., 2001). A significant
lack in the number of studies addressing the effect of
the physician’s time in the treatment of patients was
also mentioned (Donati et al., 2008).
There was a study that mentioned limitations on
demonstrating the usage of system integration for
certain situations, which might not have any
influence in patient outcomes (Rothschild, 2004).
In some situations, although the usage of
innovating technologies could be seen as an
improvement for patient, clinical staff discarded this
approaches due to the long needed training on the
technology and the difficulty in learning.
5 CONCLUSIONS
The clinical use of computers has been increasing
substantially, especially in critical care, where they
have become routinely integrated with patient
monitoring, laboratory results and the overall data
resulted from an ICU episode. The evaluation of
such data is extremely important in order to improve
decision making and a better care. However, due to
the large amount of data, clinicians spend a lot of
time searching and analyzing this information.
This review attempted to answer one question: Is
system integration important for the treatment of
inpatients in the ICU?
There are difficulties related to the learning
curve with the usage of a new technology, which
may require an initial higher dedication from clinical
staff. These difficulties can be caused by the
complexity of the systems and by the level of
knowledge in using computers by the clinical staff.
However, a centralized CIS allows the reduction of
incidents resulting from serious medication errors,
including adverse drug events and transcription
errors, allows a significant reduction on time spent
documenting information and vital signs improving
the accessibility to patient data, the quality, the
efficiency and timeliness to data important in the
overall patient care.
Comparing both advantages and disadvantages,
it can be stated that a centralized CIS is extremely
important for inpatients in an ICU.
In future work, a systematic review should be
performed in more databases in order to include a
larger number of articles. In order to effectively
assess a correct evaluation of the importance of a
centralized system in an ICU, a CIS should be
implemented and a clinical case should be evaluated.
REFERENCES
Donati, A., Gabbanelli, V., Pantanetti, S., Carletti, P.,
Principi, T., Marini, B., Nataloni, S., Sambo, G.,
Pelaia, P. (2008). The impact of a clinical information
system in an intensive care unit. Journal of Clinical
Monitoring and Compuing. (Vol.22, pp.31-36).
Kouwe, A., Burgess, J. (2003). Neurointensive care unit
system for continuous electrophysiological monitoring
with remote web-based review. IEEE Transactions on
Information Technology in Biomedicine. (Vol. 7 No 2,
pp.130-140).
Menke, J., Broner, C., Campbell, D., McKissick, M.,
Edwards-Beckett, J. (2001, September 17).
Computerized clinical documentation system in the
pediatric intensive care unit. BMC Med Inform Decis
Mak. 1-3.
Reina-Tosina, J., Roa, L., Cáceres, J., Gómez-Cía, T.
(2002). New approaches toward the fully digital
integrated management of a burn unit. IEEE
Transactions on Biomedical Engineering. (Vol. 49,
No. 12, pp.1470-1476).
Rothschild, J. (2004). Computerized physician order entry
in the critical care and general inpatient setting: a
narrative review. Journal of Critical Care (Vol.19, No
4, pp. 271-278).
Shin, D., Huh S., Lee, T., Kim, I. (2003). Web-based
remote monitoring of infant incubators in the ICU.
Inernationalt Journal of Medical Informatics. (Vol.
71, pp.151-156).
Ward, N., Snyder, J., Ross, S., Haze, D., Levy, M. (2004).
Comparison of a commercially available clinical
information system with other methods of measuring
critical care outcomes data. Journal of Critical Care
(Vol. 19, No 1, pp.10-15).
Pubmed. Available at: http://www.ncbi.nlm.nih.gov/sites/
entrerz [Accessed 2
nd
Feb, 2010]
THE IMPORTANCE OF SYSTEM INTEGRATION IN INTENSIVE CARE UNITS - A Review
147
