
KINETIC AND KINEMATIC GAIT ASSESSMENT OF
PARAPLEGIC PATIENTS WITH AND WITHOUT ANKLE
FOOT ORTHOSES
Eliza Regina Ferreira Braga Machado de Azevedo,
Enio Walker Azevedo Cacho
Karina Cristina Alonso, Fernando Tadeu Bueno Martin
Biomechanics and Rehabilitation Lab., Department of Orthopedics and Traumatology, Faculty of Medical Sciences
University of Campinas – Unicamp, Campinas, Brazil
Alberto Cliquet Junior
Biomechanics and Rehabilitation Lab., Department of Orthopedics and Traumatology, Faculty of Medical Sciences
University of Campinas – Unicamp, Campinas, Brazil
Biocybernetics and Rehabilitation Engineering Lab, Department of Electrical Engineering, University of São Paulo, Brazil
Keywords: Kinetic, Kinematic, Gait, Ankle foot orthoses, Paraplegic.
Abstract: Objective: To assess the influence of rigid ankle foot orthoses (AFOs) on paraplegic gait with
neuromuscular electrical stimulation (NMES). Methods: Ten control subjects and five complete paraplegics
went through kinetics and kinematics gait evaluation without and with AFOs. Paraplegics also used 4
channels NMES, walker aided. Results: Cadence, in steps per minutes (94.6/6.8; 84.97/13.15; 13.02/4.11;
16.1/2.29), step length, in meters (1.31/0.15; 1.19/0.17; 0.55/0.11; 0.6/0.11) and % stance time (61.5/1.8;
62.93/3.37; 87.8/7.26; 89.9/2.6) for controls and paraplegics, without and with AFOs, respectively.
Differences are shown for the controls as well as between paraplegic groups. Ankle joints kinematics
displayed no significant changes. However, the ankle dorsiflexion, in the support phase, for controls and
paraplegics with AFO was higher than expected (10.97/5.67; 15.48/8.08). Kinetic values were: maximum
hip extensor moments (Nm/kg) of 1.84/0.48; 3.36/5.79; 1.45/0.59; 1.58/0.41 and maximum knee extensor
moments of 3.53/0.52; 3.04/0.87; 1.44/1.37; 1.24/0.78. Conclusion: Within the paraplegic groups, through
spatiotemporal results, gait with AFO was more effective. Nevertheless, the AFO allowed more ankle
mobility than expected. Furthermore, lower limb loading, i.e. hip and knee moments generated during
NMES+AFO paraplegic gait allows for bone mass increase.
1 INTRODUCTION
The incidence of spinal cord injury varies around the
world, but it is usually reported to be between 20
and 50 cases per million per year and approximately
half of whom are under 30 years of age (Barbeu et
al, 1999).
The main complaint of spinal cord injury
individuals is the mobility loss below the lesion and
consequently, the inability to walk. For this reason,
recent studies are being performed on locomotion
after spinal cord injury (Behrman et al, 2000).
These individuals’ gait can be restored through
the electrical activation of paralyzed or spastic
muscles, using neuromuscular electrical stimulation
(NMES) (Behrman et al, 2000). This gait seeks to
minimize the general physiological effects resulting
from spinal cord lesions, i.e., osteoporosis, muscle
atrophy, cardiovascular deficiencies, spasticity,
repetitive urinary infections, and others (Carvalho et
al, 2005; Carvalho et al, 2006; Sepulveda, 1997).
Auxiliary devices are also used during such gait,
like walkers and orthoses, mainly rigid ankle foot
orthoses (AFO), which restrict the ankle’s mobility,
keeping the foot in dorsiflexion and avoiding ankle
fractures; furthermore it does not allow the tibia’s
bearing on the foot during the stance, reduce the
equinus, thus improving the body weight support
during the stance and pre-balance phases. Besides
the effects on foot and ankle, the rigid AFO also
provides different effects on the proximal joints
during the gait (Abel et al, 1998).
98
Alonso K., Cacho E., de Azevedo E., Martin F. and Cliquet Junior A. (2010).
KINETIC AND KINEMATIC GAIT ASSESSMENT OF PARAPLEGIC PATIENTS WITH AND WITHOUT ANKLE FOOT ORTHOSES.
In Proceedings of the Third International Conference on Biomedical Electronics and Devices, pages 98-102
DOI: 10.5220/0002718700980102
Copyright
c
SciTePress
Therefore, it becomes rather important to analyze
the AFO’s effects on the paraplegic gait, in order to
understand the differences generated by its use,
towards producing a more functional gait for these
patients.
2 METHODS
Ten healthy control subjects and five complete
paraplegics, with lesions over one year old (all male
and aged between 20 and 40 years) were recruited.
The work was approved by the local Ethics
Committee.
All individuals went through kinetics and
kinematics gait evaluation at The Biomechanics and
Rehabilitation Laboratory of the UNICAMP Clinical
Hospital. For this assessment a six meter long
versus one meter wide pathway was used, together
with a force platform (AMTI, Newton, MA, USA)
and six infrared cameras ProReflex (Qualisys),
sampling being done at 240Hz. Rigid AFOs, a pair
of sandals, ankle protection braces and seven
reflective spherical markers placed on a lower limb
(between the second and third metatarsal, on lateral
malleolus, calcaneus, tibial tuberosity, knee joint
line, superior patella and greater trochanter of
femur) were also part of the gear.
The paraplegics walked on the pathway placing a
foot on the force platform, using four channels of
NMES bilaterally (quadriceps muscles and fibular
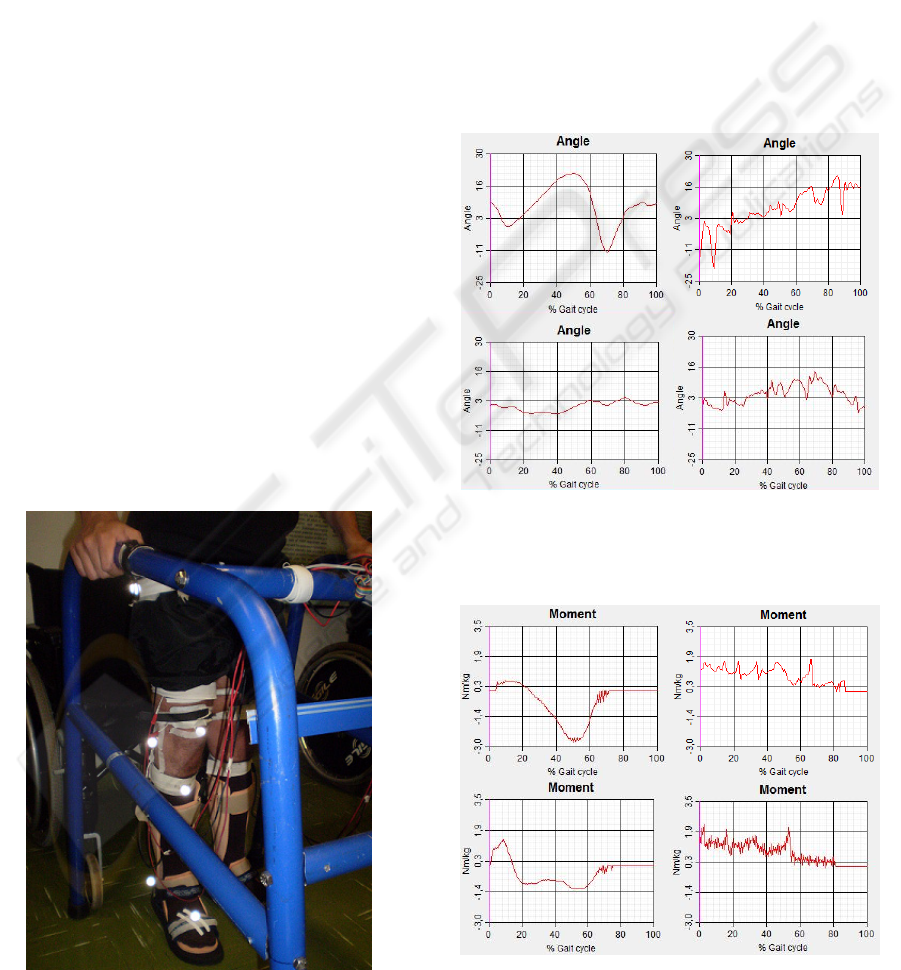
Figure 1: Paraplegic gait with AFOs + NMES, sandals and
reflective spherical markers.
nerve) and walker aided in two different situations.
First with rigid AFOs and sandals (figure 1), after
this, just with sandals and ankle braces.
The control group also walked on the pathway,
placing the right foot on the force platform, first
walking using only the sandals and after that,
sandals with the rigid AFOs. As soon as they put on
the orthoses the subjects walked for some minutes to
get used to the AFOs.
All situations were performed three times on the
same day and the averages were taken for analysis.
Parameters analyzed were cadence, step length,
percentage of stance, ankle, knee and hip angles and
also moments on these joints.
Figure 2: Typical kinematic data of ankle: a) Controls
without AFOs, b) Paraplegics without AFO, c) Controls
with AFOs, d) Paraplegics with AFOs.
Figure 3: Typical kinetic data of ankle: a) Controls
without AFOs, b) Paraplegics without AFO, c) Controls
with AFOs, d) Paraplegics with AFOs.
a b
c d
c d
a
b
Ankle’s angle
Ankle’s moment
KINETIC AND KINEMATIC GAIT ASSESSMENT OF PARAPLEGIC PATIENTS WITH AND WITHOUT ANKLE
FOOT ORTHOSES
99
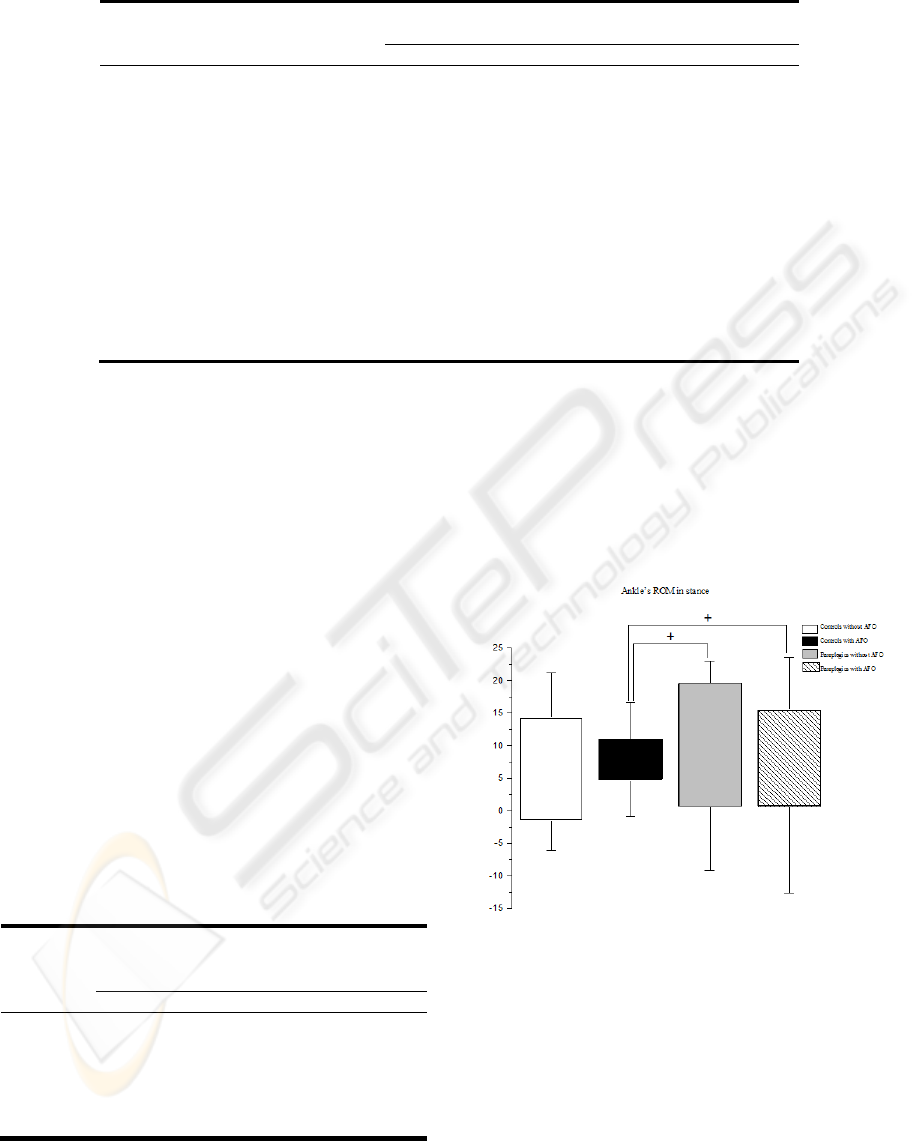
Table 2: Kinematic data.
Variables
Control
without AFO
Control
with AFO
Paraplegic
without AFO
Paraplegic
with AFO
Mean / SD Mean / SD Mean / SD Mean / SD
Ankle initial contact (º) 3,6 / 4,78 4,55 / 4,54 -2,33/3,05*
+
0,25 / 6,22
Ankle’s ROM in stance (º) 15,86/5,76 6,28/1,55 19,72/10,5
+
14,82/7,51
+
Ankle’s ROM in balance (º) 15,00/4,92 5,27/1,73 14,93/10,04
+
12,68/11,82
Knee’s initial contact (º) -0,69 / 5,4 4.51/6.3 1.95/8.0 3.27/6.45
Knee’s flexion at toe-off (º) 35.10/5.5 32.63/4.9 13.73/9.5*
+
11.13/6.9*
+
Maximum knee flexion in balance (º) 64.50/5.8 63.59/7.9 19.17/12.7 14.9/10.6*
+
Knee’s ROM in stance (º) 28,4/3,00 20,92/4,86 25,05/12,08 15,13/4,61
Hip’s initial contact (º) 17.98/4.5 18.35/4.3 4.57/3.6*
+
6.2/2.23*
+
Maximum hip extension in stance (º) -13.08/3.9 -14.07/4.0 -18.98/2.2*
+
20.76/6.07*
+
Hip at toe-off (º) -8.08/4.7 -7.8/4.8 -15.85/6.0*
+
-14.35/5.22*
+
Maximum hip flexion in balance (º) 22.59/4.8 23.75/6.8 9.23/8.0*
+
12.07/4.65*
+
Hip’s rotation ROM (º) 19,41/4,48 18,05/4,6 39,94/14,23*
+
52,56/29,66*
+
Hip’s abdu/adu ROM (º) 7.69/2.6 7.42/2.8 12.44/3.4*
+
13.31/4.42*
+
Abbreviations: SD, standard deviation; Abdu, abduction; Adu, aduction; ROM, Range of motion.
*p<0,05 between controls without AFO and paraplegics,
+
p<0,05 between controls with AFO and paraplegics.
Figures 2 and 3 show typical data illustrating angles
and moment, respectively, about the ankle for
controls and paraplegics (NMES) with and without
AFOs.
Data analysis was performed using the Mann-
Whitney test, using Bioestat 4.0 program to verify
the samples variance. The controls were compared
with the patients in the two different situations,
considering p<0,05 as statistically significant.
3 RESULTS
Individuals in the control group presented a mean
age of 23.6 (±2,46) years old, mass of 80,3 (±12,69)
kilograms and height of 1,81 (±0,06) meters. For
the paraplegic group the mean age was
31,4 (±8,62) years old, mass 80,8 (±14,74)
kilograms and height of 1,81 (±0,08) meters.
Table 1: Spatiotemporal variables.
Variables
Control
without
AFO
Control
with AFO
Paraplegic
without
AFO
Paraplegic
with AFO
Mean/SD Mean/ SD Mean / SD Mean/ SD
Cadence
(steps/ min)
94.6 / 6.8
84.97 /
13.15
13.02 /
4.11*
+
16.1 /
2.29*
+
Step length
(m)
1.37 /
0.15
1.18 /
0.17
0.55/
0.11*
+
0.6/ 0.11*
+
% stance
time
61.5 /
0.15
62.93 /
3.37
87.8 /
7.26*
+
89.9 / 2.6*
+
Abbreviations: SD, standard deviation.
*p<0,05 between controls without AFO and paraplegics,
+
p<0,05 between controls with AFO and paraplegics
The results of spatiotemporal variables are shown in
table1. Table 2
presents kinematic data and figures
4, 5 and 6 flexion-extension range of motion (ROM)
of ankle in stance and balance and knee in stance
respectively. Figure 7 represents hip rotation ROM.
The kinetic results are shown in table 3.
Figure 4: Ankle’s ROM in stance for controls without and
with AFO and paraplegics without and with AFO. Values
are mean and standard deviation (SD). *p<0,05 between
controls without AFO and paraplegics,
+
p<0,05 between
controls with AFO and paraplegics.
BIODEVICES 2010 - International Conference on Biomedical Electronics and Devices
100
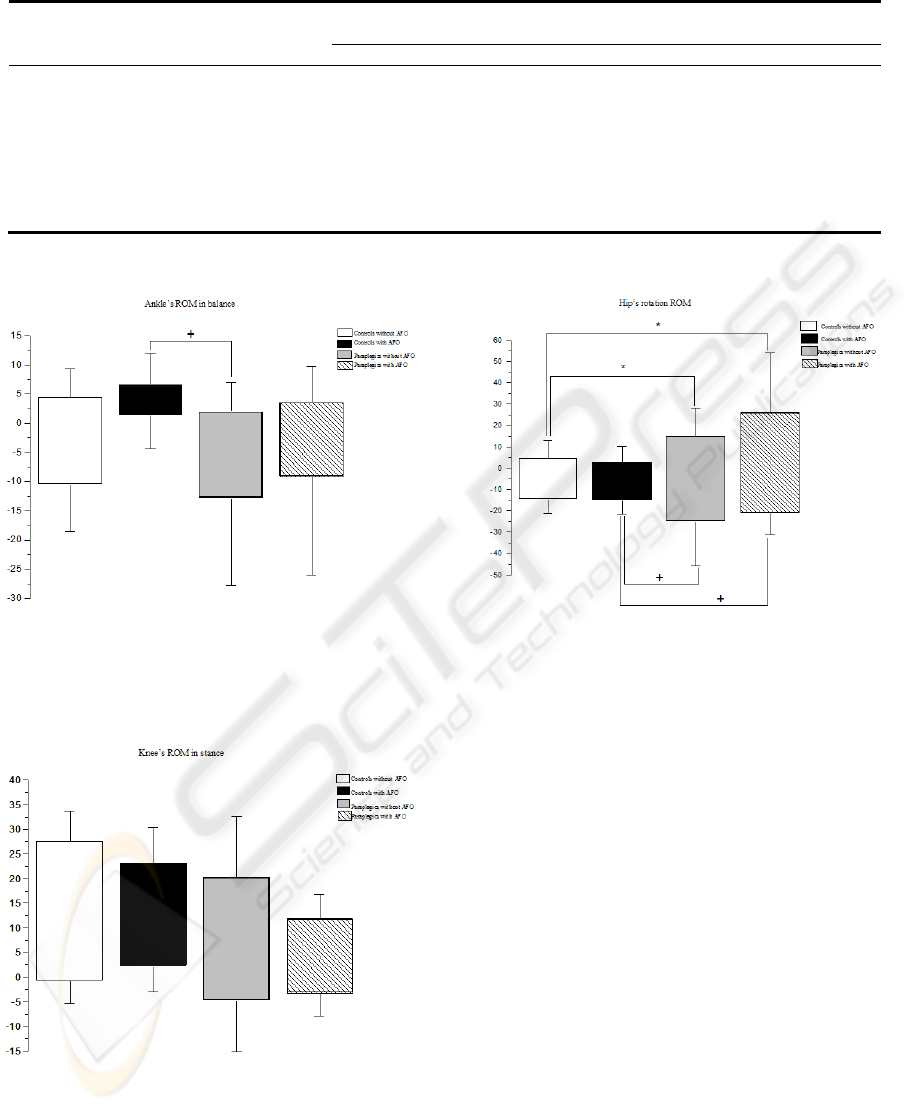
Table 3: Kinetic data.
Variables Control without
AFO
Control with
AFO
Paraplegic without
AFO
Paraplegic with
AFO
Mean / SD Mean / SD Mean / SD Mean / SD
Ankle moment at load response (Nm/kg) -0.01 / 0 0.09 / 0.21 0,42 / 0,37 0,6 / 0,48*
Maximum ankle moment (Nm/kg) 0.74/0.31 0.9/0.51 1.25/0.88 1.4/0.56*
Ankle moment at presswing (Nm/kg) -0.95/0.58 -0.68/0.28 -0.08/0.93 -0.25/0.85
Maximum knee flexion moment (Nm/kg) -1.3/0.36 -1.19/0.51 -1.2/0.47 -1.48/0.35
Maximum knee extension moment (Nm/kg
)
3.53/0.52 3.04/0.87 1.44/1.37* 1.24/0.78*
+
Maximum hip extension moment (Nm/kg) 1.84/0.48 3.36/5.79 1.45/0.59 1.58/0.41
Maximum hip flexion moment (Nm/kg) -4.65/0.6 -3.82/0.89 -1.6/1.85*
+
-1.02/1.1*
+
Maximum abduction moment (Nm/kg) -1.84/0.61 -2.1/0.49 -2.23/0.56 -1.6/0.6
Abbreviations: SD, standard devia
*p<0,05 between controls without AFO and paraplegics,
+
p<0,05 between controls with AFO and paraplegics.
Figure 5: Ankle’s ROM in balance for controls without
and with AFO and paraplegics without and with AFO.
Values are mean and standard deviation (SD). *p<0,05
between controls without AFO and paraplegics,
+
p<0,05
between controls with AFO and paraplegics.
Figure 6: Knee’s ROM in stance for controls without and
with AFO and paraplegics without and with AFO. Values
are mean and standard deviation (SD). *p<0,05 between
controls without AFO and paraplegics,
+
p<0,05 between
controls with AFO and paraplegics.
Figure 7: Hip’s rotation ROM for controls without and
with AFO and paraplegics without and with AFO. Values
are mean and standard deviation (SD). *p<0,05 between
controls without AFO and paraplegics,
+
p<0,05 between
controls with AFO and paraplegics.
4 DISCUSSION
The ankle joint has important mechanical and neural
control roles during gait, its muscles acting to
support the body weight and moving the center of
mass forward during the final stance and early
balance, also reducing the energy loss (Sawicki et al,
2006). However, neurological or orthopedic patients
who have equinus foot, make use of rigid AFOs to
improve gait, through an increasing speed and better
stability during stance phase (Sawicki et al, 2006;
Radtka et al, 2006; Kim et al, 2004). In this study,
subjects in the control group showed an increase in
the stance percentage and a decrease in cadence and
step length when using the rigid AFO. In the
paraplegic group such decrease was noted when the
subjects were not using the orthoses. Kim et al
(2004) analyzed gait in 19 incomplete spinal cord
injured subjects on four different situations: with
KINETIC AND KINEMATIC GAIT ASSESSMENT OF PARAPLEGIC PATIENTS WITH AND WITHOUT ANKLE
FOOT ORTHOSES
101

AFO and NMES (on the fibular nerve), with AFO,
with NMES and without orthoses, finding that when
used together, the AFO and NMES provided better
benefits to the patient’s gait, such as increasing
speed, step length and cadence. NMES acted more
during the balance and the AFO in stance by
improving the patient’s ability to the support the
body weight during the early stance.
In another study, Sawicki et al (2006) performed
a kinematic and electromyographic ankle’s
assessment of five incomplete spinal cord injury
patients during treadmill gait in three different
situations, without AFO, with AFO and with
pneumatic AFO which promoted plantar flexion
during the gait. From that, they observed a better
muscle activation, a greater ankle’s angle and
moment when patients were using the two types of
orthoses. Such results were also found in this present
study, with complete paraplegics.
Rather relevant in this present work is that
dorsiflexion was found higher than expected for the
subjects of all groups using the rigid AFO. This may
have occurred due to polypropylene material
deformation during weight loading / unloading. In
another AFO study also a higher ankle dorsiflexion
was noted due to the material deformation that
occurs even in rigid AFOs type (Behrman et al,
2000).
Kinetics and kinematics compensations in
proximal joints were also noted when the groups
were using the rigid AFO. Radtka et al (2006) also
showed these compensations in healthy subjects
using rigid AFO, but their study was in stair
locomotion.
Subjects who suffer spinal cord injury present a
significant reduction of physical capacity resulting
in a dramatic decrease in bone mineral density.
Carvalho et al (2006) evaluated the effect of
treadmill gait training associated with NMES on
bone mass of twenty one tetraplegic subjects and the
results showed that the increase in bone formation
rate was associated with gait training. This also may
happen in paraplegic’s gait training.
In the present study, the hip extension moment
were higher during the gait with AFO, which means
that the AFO provides an increase of the mechanical
load on the hip, what can lead to prevent or reverse
the bone loss.
5 CONCLUSIONS
The spatiotemporal results suggest that the gait with
AFO is more effective for complete paraplegic
individuals. Also, the findings show how restrictions
on ankle’s joint through AFO can affect not only this
joint, but also knee and hip, for compensation of
ankle’s loss of mobility. Furthermore, the AFO
allowed more ankle mobility than expected and the
lower limb loading, i.e. hip moments generated
during NMES with AFOs paraplegic gait allows for
bone mass increase.
ACKNOWLEDGEMENTS
The State of São Paulo Foundation for Research –
FAPESP.
REFERENCES
Abel, M.F., Juhl, G.A., Vaughan, C.L., Damiano, D.L.,
1998. Gait assessment of fixed ankle-foot orthoses in
children with spastic diplegia. Arch Phys Med Rehabil.
v. 79, p. 126-133.
Barbeu, H., Ladouceur, M., Norman, K.E., Pépin, A.,
1999. Walking after spinal cord injury: evaluation,
treatment, and functional recovery. Arch Phys Med
Rehabil. v. 80, p.225-235.
Behrman, A.L., Harkema, S.J., 2000. Locomotor training
after human spinal cord injury: a series of case studies.
Physical Therapy. n. 7, v. 80, p. 688-699.
Carvalho, D.C., Cliquet, A. Jr., 2005. Response of the
arterial blood pressure of quadriplegic patients to
treadmill gait. Braz J Med Biol Res. n. 38, v. 9, p.
1367-1373.
Carvalho, D.C., Garlipp, G.R., Bottini, P.V., Afaz, S.H.,
Moda, M.A., Cliquet, A.Jr., 2006. Effect of treadmill
gait on bone markers and bone mineral density of
quadriplegic subjects. Braz J Med Biol Res. n. 39,
v.10, p. 1357-1363.
Kim, M., Eng, J.J., Whittaker, M.W., 2004. Effects of a
simple functional electric system and/or a hinged
ankle-foot orthosis on walking in persons with
incomplete spinal cord injury. Arch Phys Med Rehabil.
v. 85, p. 1718-1723.
Radtka, S.A., Oliveira, G.B., Lindstrom, K.E., Borders,
M.D., 2006. The kinematic and kinetic effects of solid,
hinged, and no ankle-foot orthoses on stair locomotion
in healthy adults. Gait and Posture. n. 24, p. 211-218.
Sawicki, G.S., Domingo, A., Ferris, D.P., 2006. The
effects of powered ankle-foot orthoses on joint
kinematics and muscle activation during walking with
incomplete spinal cord injury. Journal of
NeuroEngineering and Rehabilitation. n.3, v.3, p.1-17.
Sepulveda, F., Granat, M.H., Cliquet, A. Jr., 1997. Two
artificial neural systems for generation of gait swing
by means of neuromuscular electrical stimulation. Med
Eng Phys. n. 1, v. 19, p. 21-28.
BIODEVICES 2010 - International Conference on Biomedical Electronics and Devices
102
