
BCCI - A BIDIRECTIONAL CORTICAL COMMUNICATION
INTERFACE
A. Walter, M. Bensch, D. Brugger, W. Rosenstiel
Department of Computer Engineering, Eberhard-Karls-University Tuebingen, Tuebingen, Germany
M. Bogdan
Department of Computer Engineering, University of Leipzig, Leipzig, Germany
N. Birbaumer
Institute of Medical Psychology and Behavioural Neurobiology, University of Tuebingen, Tuebingen, Germany
A. Gharabaghi
Functional and Restorative Neurosurgery Unit, Department of Neurosurgery, and Neuroprosthetics Research Group
Werner Reichardt Centre for Integrative Neuroscience, University Hospital, Tuebingen, Germany
Keywords:
Brain-computer interface, ALS, Stroke, Cortical stimulation, Adaptive stimulation.
Abstract:
Therapeutic methods based on efferent signals from the patients’ brain have been studied extensively in the
field of brain-computer interfaces and applied to paralysed and stroke patients. Invasive stimulation is used as
a therapeutic tool for patients with Parkinson disease, intractable chronic pain and other neurological diseases.
We give a short review of currently used applications for cortical stimulation for stroke patients and brain-
computer interfaces for paralyzed patients. We propose a refined approach for stroke rehabilitation as well as
the extension of the use of invasive cortical stimulation to ALS patients with an experimental setup inspired
by classical conditioning to facilitate the communication with brain-computer interfaces for LIS and CLIS
patients. A closed-loop system is described with sophisticated methods for the identification of recording and
stimulation sites, feature extraction and adaptation of stimulation algorithms to the patient in order to design a
bidirectional cortical communication interface (BCCI).
1 INTRODUCTION
Brain-computer interfaces (BCI) are a tool for com-
munication without the need of muscle use by mod-
ulation of brain waves and brain states by the user.
These modulations can be detected online or offline
by feature extraction algorithms and fed to classi-
fication or regression algorithms that try to deter-
mine the intention of the BCI user. The aim of
these BCI systems is to allow communication with
the surrounding world even if the normal muscular
communication channels are severly impaired. Pos-
sible applications can be found in the field of neu-
roprosthetics, for example control of a wheelchair
or a robotic limb or they can be designed to en-
able patients to select letters in order to spell sen-
tences (Birbaumer et al., 1999)(Donchin et al., 2000).
There exist different paradigms for BCI, for exam-
ple slow cortical potentials, sensory-motor rhythms
or P300. A detailed description of these paradigms is
found in (Birbaumer and Cohen, 2007). The signals
are measured most commonly by electroencephalog-
raphy (EEG), but magnetoencephalography (MEG)
and blood-oxygen-level dependent functional MRI
(fMRI) BCIs are also used as non-invasive methods.
The advantage of an invasive approach is a better
signal quality. Penetrating multi-electrode arrays are
used in experimental studies, but epicortical grids are
more promising in regular clinical applications be-
cause of the good tradeoff between procedural risk
and signal quality.
Patients that can benefit from the use of BCIs as a
communication tool might be suffering from diseases
like brain stem lesion, spinal cord injury or amy-
otrophic lateral sclerosis (ALS). These conditions can
lead to a locked-in syndrome (LIS) which means that
the patient is severly impaired in his ability to inter-
act with the outside world. Stroke patients on the
440
Walter A., Bensch M., Brugger D., Rosenstiel W., Bogdan M., Birbaumer N. and Gharabaghi A. (2009).
BCCI - A BIDIRECTIONAL CORTICAL COMMUNICATION INTERFACE.
In Proceedings of the International Joint Conference on Computational Intelligence, pages 440-445
DOI: 10.5220/0002318304400445
Copyright
c
SciTePress

other hand can use brain signals as an addition to
standard rehabilitative actions such as physiotherapy
(Buch et al., 2008). We propose in this paper a new
approach for communication with locked-in patients
as well as a therapeutic approach in stroke rehabilita-
tion using epicortical electrical stimulation. The stim-
ulation parameters will be adapted to the background
activity that is measured before stimulus onset. Back-
ground activity is assumed to profoundly change the
properties of signal transmission of neurons and thus
interfere with the activity evoked by stimulation (Des-
texhe et al., 2003). Animal experiments have shown,
that a closed-loop system for adaptation of the param-
eters is feasible, at least for single-electrode measure-
ments (Brugger et al., 2008).
The paper is structured as follows: We describe in
section 2 state of the BCI systems for ALS and stroke
patients. Section 3 contains an overviewover the ther-
apeutic application of cortical stimulation for stroke
patients. We present in section 4 our new approach
for a closed-loop system in stroke rehabilitation and
as an improvement for communication with ALS pa-
tients.
2 BRAIN-COMPUTER
INTERFACES FOR ALS AND
STROKE
2.1 ALS
Amyotrophic lateral sclerosis is an adult-onset mo-
tor neuron disease characterized by degeneration of
the first and second motor neurons (Lakerveld et al.,
2008). Over the course of the disease, the pa-
tient gradually loses control of the muscles, devel-
ops weakness and spasticity and dies from respira-
tory failure usually within a few years, unless arti-
ficially ventilated and fed. Cognitive functions are
said to be spared even in the latest stages of ALS
except for patients with frontal lobe dementia (Lak-
erveld et al., 2008). The patient might communicate
in this state by controlling devices with single mus-
cles. Therefore, a BCI can be useful to allow the
patient to carry out complex tasks, for example the
control of a web browser (Bensch et al., 2007) and to
provide a communication channel after muscular con-
trol has been lost. There has been extensive research
on the use of BCIs for ALS patients and about 75 %
of these patients was able to control a BCI (Kuebler
and Kotchoubey, 2007). However, none of these re-
sults could be transferred to patients in the completely
locked-in state (CLIS) and not a single CLIS patient
has regained communication via a BCI (Birbaumer
and Cohen, 2007). Because of this, new approaches
for BCIs have to be tested to train LIS patients in their
use, hoping that the training effects might carry over
to the CLIS state.
2.2 Stroke
Stroke is a leading cause of paralysis and disability
worldwide with several hundred thousand incidents
per year. The outcome of such an incident depends
heavily on the location and the size of the stroke
area, but is fatal in about a third of all cases during
the first year after the stroke and leaves most of the
surivors with persisting neurological deficits. A pos-
sible deficit is a movement impairement on the con-
tralateral side, if the stroke affects motor areas like the
primary motor cortex M1 or the supplementary motor
area (SMA). Rehabilitative procedures for movement
impaired stroke patients consist mostly of physiother-
apy, which can lead by itself to improvements espe-
cially in lower limb functions like standing or walk-
ing. Therapy of upper limb function on the other hand
still needs to be improved (French et al., 2007).
Brain computer interfaces are a promising tool to aid
in the rehabilitation process of stroke patients. This
idea is based on the standard BCI paradigm of motor-
imagery experiments. Intuitively, the best way to im-
proverehabilitation is to couple the physiotherapyand
the movement intention of the patient in order to get a
causal relationship between the planning of the move-
ment, which should still be possible, and the sensory
feedback of the movement. One paradigm in BCI re-
search is ‘motor-imagery’tasks. The patient imagines
movements of different limbs, for example foot, hand
or tongue. This leads to a detectable event-related
desynchronization of the µ-rhythm originating in sen-
sorimotor areas (Pfurtscheller et al., 2005). In the
MEG BCI study of Buch (Buch et al., 2008), patients
were asked to imagine movements of the paralyzed
hand which were detected by the BCI system and ef-
fected the timed openings and closings of the orthosis.
The patients were able to learn to reliably control the
orthosis. This ability did not lead to functional reha-
bilitation of the affected hand.
3 CORTICAL STIMULATION
FOR STROKE
REHABILITATION
Since the 1990s, non-invasive stimulation has been
used on stroke patients for prognostic and diagnostic
BCCI - A BIDIRECTIONAL CORTICAL COMMUNICATION INTERFACE
441
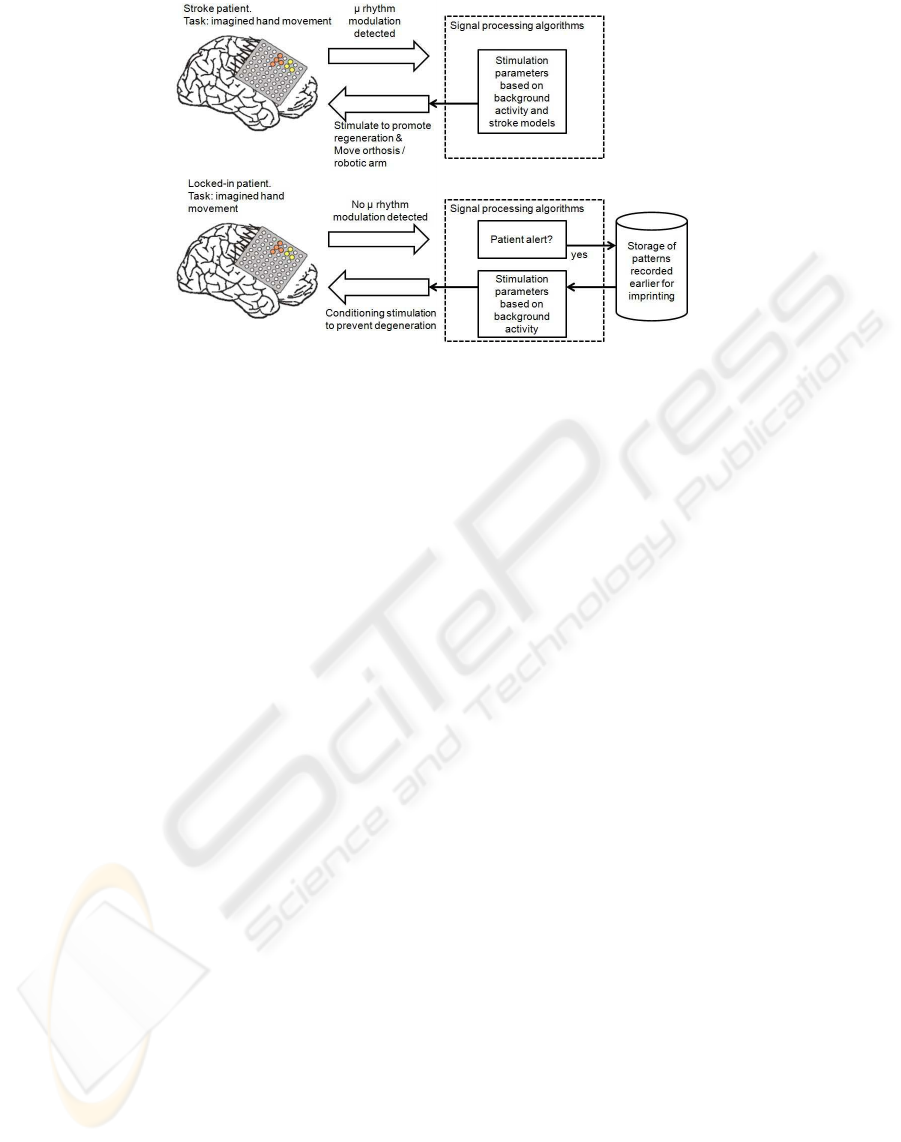
Figure 1: Overview of a stimulation paradigm for stroke patients (top) and locked-in patients (bottom).
measure as well as a tool for pathophysiological re-
search. Transcranial magnetic stimulation (TMS) and
transcranial direct current stimulation (tDCS) are the
best known representatives of this group of methods.
TDCS is applied directly on the scalp with large
sponge electrodes soaked in saline. A direct cur-
rent of a few milliampere is applied to the electrodes.
Even if most of the current travels directly through the
scalp because of the low conductivity of the skull, this
method still influences brain tissue.
TMS on the other hand utilizes strong magnetic fields
typically with a coil placed directly above the area of
interest. Magnetic fields are less influenced by the
low conductivity of the skull than electrical currents
which leads to induction of currents in the underlying
brain tissue. Measureable aftereffects of this method
can last for several minutes to more than an hour, de-
pending on the stimulation protocol used (Fitzgerald
et al., 2006). It is possible to enhance or decrease
cortical excitability depending on the stimulation fre-
quency of repetitive TMS and the stimulus polarity in
case of tDCS. A review on noninvasive brain stimula-
tion can be found in (Wagner et al., 2007).
In recent years, these non-invasive techniques were
applied to stroke patients to improve the success rate
of standard physiotherapy (Hummel et al., 2008). A
disadvantage of the application of tDCS is the loss of
effect focality as the affected area is stretched out be-
tween two large electrodes. TMS is not affected by
this issue, but the aftereffects of TMS are not long-
lasting.
A possibly powerful alternative is invasive cortical
stimulation by epicortical electrode strips. A cran-
iotomy is necessary for the implantation, bearing the
risk of infections or other complications, but first
studies with implanted electrodes show promising
results without serious complications (Levy et al.,
2008)(Brownet al., 2006). Implantabledeviceswhich
act autonomously or may be switched on and off by a
handheld wand offer the possibility of cortical stimu-
lation during physiotherapy. In 2007, Northstar Neu-
roscience conducted a multicenter Phase III clinical
trial that tested a prototype of an implanted stimula-
tor for stroke recovery with 146 patients (Levy et al.,
2008). The results were promising, but the effectsizes
were not as high as expected. The fraction of pa-
tients improving on the Upper Extremity Fugl-Meyer
Scale or the Arm Motor Ability Test did not differ sig-
nificantly between the physiotherapy group and the
group that additionally received cortical stimulation.
Our goal is to improve this result with a closed-loop
stimulus control that utilizes the capacity of implanted
electrodes to be used for stimulation and recording si-
multaneously. This opens a new field that is still un-
explored to the best of our knowledge: Invasive stim-
ulation of stroke patients for rehabilitation based on
simultaneous recorded background activity. A possi-
ble stimulation paradigm is summarised in figure 1.
4 A CLOSED-LOOP SYSTEM
FOR STROKE AND ALS
There are at least three issues that need to be ad-
dressed in order to provide optimized stimulation for
the patient (Plow et al., 2009): (1) Identification of the
target site and electrode placement, (2) models for the
effect of the stimulation and (3) finding the optimal
stimulation pattern depending on the disease and the
patient.
IJCCI 2009 - International Joint Conference on Computational Intelligence
442

4.1 Electrode Placement
The target area will be determined preoperatively by
fMRI guided TMS. EMG measurements will be used
to track the arm movements initiated by the patient
as well as those evoked by TMS. During surgery, the
neurosurgeon will perform functional mapping of the
area of interest on the motor cortex to decide upon the
exact electrode placement. This is an improvement to
earlier studies that used only fMRI to place the elec-
trodes (Plow et al., 2009).
4.2 Modeling the Current Flow
The specific anatomy, the pathologic alterations and
the influx of cortico-spinal fluid change the conduc-
tivity with respect to healthy tissue due to the creation
of new shunting routes for the currents, which can
distort the electric field produced by the stimulation
(Wagner et al., 2006). Thus, we need to ensure that
the desired brain regions are targeted by the stimula-
tion (Plow et al., 2009). We will conduct modeling
studies of the stimulation that show volume conduc-
tion effects by a finite element model (FEM). Stan-
dard models range in complexity from simple spher-
ical head models to complex realistic head models
based on MRI measurements. The different tissue
classes are modeled with conductivities based on val-
ues measured during experiments. Models of the elec-
trodes will be placed in the vicinity of the lesion to
investigate the effect of stimulation on the tissue. The
integration of areas affected by stroke based on MR
measurements of the patients into the model will lead
to further improvements of the accuracy of predic-
tions on the current spread by volume conduction.
4.3 Patient-specific Stimulation
4.3.1 ALS
Hypotheses, why ALS patients are not able to com-
municate with BCIs in the completely locked-in state
include: (1) difficulty in performing the task because
of cognitivedeficits or lack of alertness (2) inability to
modulate the cortical rhythms due to degeneration or
missing feedback (3) unwillingness to cooperate (Hill
et al., 2005). Especially because of (1), we need to
ensure that the ALS patients are in a suitable cogni-
tive state.
Cognitive deficits, for example frontotemporal de-
mentia have been reported in ALS, so we will use
cognitive tests to make sure that the patient is able
to understand the instructions and operate the BCI.
The alertness of the patient should be as high as pos-
sible during the experiments. Late-stage ALS patients
can not report on their current level of alertness and
thus, the researcher has to ensure that the patient is not
drowsy or sleeping during the experiment. There are
some peripheral measures that can be used as an indi-
cator for alertness, for example the heart rate. A spec-
tral analysis of the EEG or ECoG can also be helpful,
as lack of alertness can be correlated to changes in the
alpha and beta frequencies (Jung et al., 1997).
We include a third option: the analysis of connectivity
patterns in the ECoG during BCI experiments based
on phase synchronization and causality measures. It
can be assumed, that the BCI performance of patients
(which can be measured by the classification error
of the BCI system) is to a certain degree related to
their state of alertness. As an extreme example: One
can expect, that the performance of a very drowsy or
even sleeping person will be found to be somewhere
around chance level.
With this in mind, an alertness classification to
identify the relevant cortical activity and/or spectral
patterns should be possible if we link the signals
recorded before each trial to the BCI performance of
the trial. We will use the activity or spectral patterns
associated with particularly good and bad BCI per-
formance to assess the alertness of the patient before
an experimental session takes place. This evaluation
will help to decide whether an experiment should be
conducted, or if additional methods should be used to
stimulate the alertness of the patient.
Degeneration of nervous tissue and cortical connec-
tions in ALS may stem from two processes: On the
one hand direct pathological degeneration that pre-
vents the patients from controlled use of their mus-
cles and on the other hand the missing feedback due
to the underused muscles. Our theory here is: if the
patient is not able to affect his environment, the miss-
ing feedback leads to functional deterioration. As a
result, the patient is unable to reactivate these connec-
tions which has a negative effect not only on muscle
control, but might also impair his ability to imagine
muscle movement for a BCI based on µ rhythm mod-
ulation (Pfurtscheller et al., 2005).
P300 BCIs and slow cortical potential BCIs rely on
visual stimulus presentation and visual feedback re-
spectively. The inability of ALS patients in CLIS to
operate these types of BCI may stem from the fact
that eye focussing is also affected by the disease (Bir-
baumer and Cohen, 2007). Thus, the visual system
is not a good communication channel for ALS pa-
tients. There exist auditory P300 systems, but their
efficiency for CLIS patients has not been tested yet.
Our hypothesis here is, that feedback applied by cor-
BCCI - A BIDIRECTIONAL CORTICAL COMMUNICATION INTERFACE
443

tical stimulation to the patient’s brain can also be used
to counter the effects of neural degeneration.
Depending on the scope of control the stimulation has
over the evoked activity in terms of amplitudes and
duration, we may be able to imprint cortical activity
that was measured in earlier sessions of the same pa-
tient. This is a potentially interesting approach for
the improvement of communication with ALS pa-
tients: When they have learned to operate a BCI in
the locked-in state, we will store the relevant activity
patterns for later use. If the BCI performance drops
during the transition from LIS to CLIS, imprinting of
the patterns recorded earlier can be considered as a
form of classical conditioning and may slow down the
functional deterioration.
If we are not able to perform the imprinting with suf-
ficient precision, a simpler approach also inspired by
classical conditioning is still feasible. We will gen-
erate two stimulation patterns for each patient, one
representing ’No’, the other one ’Yes’. True and false
statements can then be used in conjunction with the
respective stimulation pattern to condition the patient
to involuntarily modulate brain states in the absence
of stimulation. This provides the patient with a bi-
nary communication device.
While the neurosurgical procedure, the presence of
the grid in the skull and the electrical stimulation
imposes a risk on the patient, the inability of cur-
rent BCIs to establish a communication channel with
CLIS patients enforces the test of alternative ap-
proaches.
4.3.2 Stroke
The experimental setup for stroke patients will in-
clude the hand orthosis used in (Buch et al., 2008)
and a robotic arm to move the arm of the patient. The
patient will imagine movementsof the paralyzed hand
that are identified by a BCI system. If a hand move-
ment imagination is detected, the orthosis opens or
closes the hand of the patient, while elbow or shoul-
der movement imaginations trigger movements of the
robotic arm. Additionally, electrical cortical stimula-
tion is applied to the ipsilesional cortex. We will use
it to enhance cortical excitability near the lesion in
the first patients to promote regeneration. As a refine-
ment to existing stroke studies like (Levy et al., 2008),
the stimulation electrodes and parameters will depend
on results of functional mapping, volume conduction
modeling and the measured background activity.
If most of the brain tissue associated with upper limb
function is destroyed by the stroke, cortical stimula-
tion can be used to condition unaffected ipsilesional
motor cortex areas to upper limb movements. The
feasibility of this was shown by (Jackson et al., 2006)
with intracortical microstimulation in macaque mon-
keys.
4.3.3 Stimulation Parameters
Stimulation for cortical mapping or motor cortex
stimulation for patients with intractable chronic pain
consists of trains of short pulses, applied with fre-
quencies around 50-100 Hz (Brown, 2001)(Franzini
et al., 2003), which was found in animal studies to
be a frequency range that enhances local cortical ex-
citability (Teskey et al., 2003). Frequencies of 50 or
100 Hz were also used in the Northstar Neuroscience
multicenter stroke study.
As the space of all possible stimulation patterns is
very high, especially if one takes into account stim-
ulating on multiple electrodes at the same time with
a possibly free form stimulus, systematically testing
all patterns on patients is out of the question. Thus,
we will start with standard stimulation paradigms and
record the effects of the stimulation simultaneously
with the ECoG electrodes in order to analyse them
and improve the stimulation in later experiments.
We use these first experiments to investigate the pa-
rameters that establish a functional relationship be-
tween the recorded data before the stimulation, the
delivered stimulus and the stimulus evoked potentials.
This connection between stimulation parameters and
the cortical evokedpotentials will then be used to con-
struct a closed-loop system (Brugger et al., 2008). It
will enable us to adapt the stimulation parameters to
the ongoing activity and will allow prespecified target
activities to be evoked by adaptive stimulation.
5 CONCLUSIONS
We propose here an extension to classical brain-
computer interfaces that enhances the afferent path-
way to the patient’s brain using electrical stimulation
by epidural electrodes controlled by a closed-loop
system for recording, feature extraction and stimula-
tion. It is summarised in figure 1. We believe, that
our sophisticated approach for the placement of the
epidural electrodes, the stimulation patterns used and,
in case of stroke patients, the physiotherapy will lead
to therapeutic improvements for stroke patients com-
pared to standard physiotherapy and first studies on
applications of cortical stimulation for patients. Cur-
rent noninvasive BCI methods were not able to estab-
lish a communication channel with CLIS patients up
to this date. Because of this are ALS patients a sec-
ond target group of our bidirectional cortical commu-
nication interface. They might benefit by an improved
IJCCI 2009 - International Joint Conference on Computational Intelligence
444

ability to control brain-computer interfaces even in
the completely locked-in state due to the direct inter-
face for feedback to the patient’s brain which does not
rely on possibly impaired sensory systems.
ACKNOWLEDGEMENTS
This work was supported by German Research Foun-
dation (DFG GH 94/2-1), the Federal Ministry of Ed-
ucation and Research (BMBF Bernstein 01GQ0761,
BMBF 16SV3783) and the European Union (ERC
227632).
REFERENCES
Bensch, M., Karim, A., Mellinger, J., Hinterberger, T.,
Tangermann, M., Bogdan, M., Rosenstiel, W., and
Birbaumer, N. (2007). Nessi: An EEG controlled
web browser for severely paralyzed patients. Compu-
tational Intelligence and Neuroscience, 2007:71863.
Birbaumer, N. and Cohen, L. (2007). Brain-computer inter-
faces: communication and restoration of movement in
paralysis. J. Physiol., 579:621–636.
Birbaumer, N., Ghanayim, N., Hinterberger, T., Iversen, I.,
Kotchoubey, B., Kbler, A., Perelmouter, J., Taub, E.,
and Flor, H. (1999). A spelling device for the paral-
ysed. Nature, 398(6725):297–298.
Brown, J., Lutsep, H., Weinand, M., and Cramer, S. (2006).
Motor Cortex Stimulation for the Enhancement of
Recovery from Stroke: A Prospective, Multicenter
Safety Study. Neurosurgery, 58:464–473.
Brown, J. A. (2001). Motor Cortex Stimulation. Neurosurg
Focus, 11(3):A5.
Brugger, D., Butovas, S., Bogdan, M., Schwarz, C., and
Rosenstiel, W. (2008). Direct and inverse solution for
a stimulus adaptation problem using SVR. In Pro-
ceedings of the 16th European Symposium on Artifi-
cial Neural Networks. d-side Publishing.
Buch, E., Weber, C., Cohen, L., Braun, C., Dimyan,
M., Ard, T., Mellinger, J., Caria, A., Soekadar, S.,
Fourkas, A., and Birbaumer, N. (2008). Think to
Move: a Neuromagnetic Brain-Computer Interface
(BCI) System for Chronic Stroke. Stroke, 39:910–917.
Destexhe, A., Rudolph, M., and Pare, D. (2003). The high-
conductance state of neocortical neurons in vivo. Nat
Rev Neurosci, 4:739–751.
Donchin, E., Spencer, K., and Wijesinghe, R. (2000). The
Mental Prosthesis: Assessing the Speed of a P300-
Based BrainComputer Interface. IEEE TRans on Re-
hab Eng, 8:174–179.
Fitzgerald, P., Fountain, S., and Daskalakis, Z. (2006). A
comprehensive review of the effects of rTMS on mo-
tor cortical excitability and inhibition. Clinical Neu-
rophysiology, 117:2584–2596.
Franzini, A., Ferroli, P., Donges, I., Marras, C., and Broggi,
G. (2003). Chronic motor cortex stimulation for
movement disorders: A promising perspective. Neu-
rological Research, 25:123–126.
French, B., Thomas, L., Leathley, M., Sutton, C., McAdam,
J., Forster, A., Langhorne, P., Price, C., Walker, A.,
and Watkins, C. (2007). Repetitive task training for
improving functional ability after stroke. Cochrane
Database of Systematic Review, 4:CD006073.
Hill, N., Lal, T., Schroeder, M., Hinterberger, T., Wil-
helm, B., Nijboer, F., Mochty, U., Widman, G., Elger,
C., Schoelkopf, B., Kuebler, A., and Birbaumer, N.
(2005). Classifying EEG and ECoG Signals without
Subject Training for Fast BCI Implementation: Com-
parison of Non-Paralysed and Completely Paralysed
Subjects. IEEE Transactions on Neural Systems and
Rehabilitation Engineering, 14:183–186.
Hummel, F., Celnik, P., Pascual-Leone, A., Fregni, F., By-
blow, W., Buetefisch, C., Rothwell, J., Cohen, L., and
Gerloff, C. (2008). Controversy: Noninvasive and in-
vasive cortical stimulation show efficacy in treating
stroke patients. Brain Stimulation, 1:370–382.
Jackson, A., Mavoori, J., and Fetz, E. (2006). Long-term
motor cortex plasticity induced by an electronic neural
implant. Nature, 444:56–60.
Jung, T., Makeig, S., Stensmo, M., and Seinovsky, T.
(1997). Estimating Alertness from the EEG Power
Spectrum. IEEE Trans Biomed Eng, 44:60–69.
Kuebler, A. and Kotchoubey, B. (2007). Brain-computer
interfaces in the continuum of consciousness. Current
Opinion in Neurology, 20:643–649.
Lakerveld, J., Kotchoubey, B., and Kuebler, A. (2008).
Cognitive function in patients with late stage amy-
otrophic lateral sclerosis. J. Neurol. Neurosurg. Psy-
chiatry, 79:25–29.
Levy, R., Ruland, S., Weinand, M., Lowry, D., Dafer, R.,
and Bakay, R. (2008). Cortical stimulation for the
rehabilitation of patients with hemiparetic stroke: a
multicenter feasibility study of safety and efficacy. J
Neurosurg, 108:707–714.
Pfurtscheller, G., Brunner, C., Schloegl, A., and da Silva,
F. L. (2005). Mu rhythm (de)synchronization and
EEG single-trial classification of different motor im-
agery task. NeuroImage, 31:153–159.
Plow, E., Carey, J., Nudo, R., and Pascual-Leone, A. (2009).
Invasive Cortical Stimulation to Promote Recovery of
Function After Stroke. A Critical Appraisal. Stroke,
40:1926–1931.
Teskey, G., Flynn, C., Goertzen, C., Monfils, M., and
Young, N. (2003). Cortical stimulation improves
skilled forelimb use following a focal ischemic infarct
in the rat. Neurol Res, 25:794–800.
Wagner, T., Fregni, F., Eden, U., Ramos-Estebanez, C.,
Grodzinsky, A., Zahn, M., and Pascual-Leone, A.
(2006). Transcranial magnetic stimulation and stroke:
A computer-based human model study. NeuroImage,
30:857–870.
Wagner, T., Valero-Cabre, A., and Pascual-Leone, A.
(2007). Noninvasive human brain stimulation. Annu
Rev Biomed Eng, 9:527–565.
BCCI - A BIDIRECTIONAL CORTICAL COMMUNICATION INTERFACE
445
