
APPLICA
TION OF WALSH TRANSFORM BASED METHOD ON
TRACHEAL BREATH SOUND SIGNAL SEGEMENTATION
Jin Feng, Farook Sattar
School of Electrical& Electronic Engineering, Nanyang Technological University, Singapore
Moe Pwint
Dept. of Information Science, The University of Computer Studies, Yangon, Myanmar
Keywords:
Segmentation, Walsh Transform, Refinement Scheme, Inspiratory/Expiratory Phase, Various Types of Tra-
cheal Breath Sounds, End-Inspiratory/Expiratory Pause.
Abstract:
This paper proposes a robust segmentation method for differentiating consecutive inspiratory/expiratory
episodes of different types of tracheal breath sounds. This has been done by applying minimal Walsh ba-
sis functions to transform the original input respiratory sound signals. Decision module is then applied to
differentiate transformed signal into respiration segments and gap segments. The segmentation results are
improved through a refinement scheme by new evaluation algorithm which is based on the duration of the seg-
ment. The results of the experiments, which have been carried out on various types of tracheal breath sounds,
show the robustness and effectiveness of the proposed segmentation method.
1 INTRODUCTION
For early detection of diverse illnesses, accurate es-
timation of respiratory rate is very important (Sierra
et al., 2005). Many adventitious lung sounds, which
are indications of infectious and respiratory diseases,
can be clinically characterized by their duration in
respiratory cycle and relationship to the phase of res-
piration (Meslier et al., 1995). Therefore, segmenta-
tion of respiratory sound into individual respiratory
cycles and further subdividing into its inspiratory and
expiratory phases is necessary in quantifying adventi-
tious sounds.
Generally, phonopneumography or spirometer to-
gether with sound recording devices are always used
in respiratory sound analysis, in which amplitude of
the sound signal is displayed simultaneously with
the airflow as a function of time. Signals can
be segmented into consecutive inspiratory phase,
end-inspiratory pause, expiratory phase, and end-
expiratory phase according to the provided Forced
Expiratory Volume (FEV) readings (Taplidou and
Hadjileontiadis, 2007)(Cort ´es et al., 2005). However,
it could be difficult to carry out a spirometric test
for patients with high obstruction in tracheal (Cort ´es
et al., 2005).
Acoustical flow estimation is one of the first at-
tempts to relate respiratory sounds and flow. In (Hos-
sain and Moussavi, 2002) and (Golabbakhsh, 2004),
airflow has been estimated using the respiratory
sounds by applying different models, while exponen-
tial model between flow and averaged sound power
has been found with the highest estimation accu-
racy. The model coefficients calculation in the above
mentioned methods require samples of breath sound
with known flow. However, the calibration process is
not always possible. Therefore, a modified entropy-
based linear model describing relationship between
flow and tracheal sound has been derived in (Yadol-
lahi and Moussavi, 2006) without prior acoustical
flow knowledge. Also, other segmentation methods
using spectral and temporal analysis of transformed
respiratory sounds have been developed in (Hult et al.,
2000)(Sierra et al., 2004). As these researches are still
in preliminary stage, the segmentation is restricted
to normal tracheal breath and the accuracy depends
mainly on signal-to-noise ratio (SNR) for various
types of tracheal breath sounds.
In this paper, an automatic and robust respiratory
sound signal segmentation method is developed. The
proposed method is based on the modification of input
sound signal using a modified analysis and synthesis
116
Feng J., Sattar F. and Pwint M. (2008).
APPLICATION OF WALSH TRANSFORM BASED METHOD ON TRACHEAL BREATH SOUND SIGNAL SEGEMENTATION.
In Proceedings of the First International Conference on Bio-inspired Systems and Signal Processing, pages 116-121
DOI: 10.5220/0001057501160121
Copyright
c
SciTePress

scheme based on Walsh basis functions. Without the
aid of any other features, a decision module is then
applied on the modified signal by adaptive threshold-
ing for segmentation. The preliminary segmentation
result is optimized lastly by the refinement scheme
based on the segment duration. This scheme ensures
the segmentation process to perform equally accu-
rate irrespective of flow and types of tracheal breath
sounds. The proposed method is tested to be effec-
tive for both normal tracheal breath sounds as well as
adventitious respiratory sounds such as, wheeze and
stridor.
2 BACKGROUND
The Walsh transform is a matrix consisting of a com-
plete orthogonal function set having only two values
+1 and -1 over their definition intervals (Beauchamp,
1984). The motivation for using Walsh transform
rather than other transforms is its computational sim-
plicity giving a realistic processing time. The Walsh
function of order N can be represented as
g(x, u) =
1
N
q−1
∏
i=0
(−1)
b
i
(x)b
q−1−i
(u)
(1)
where u = 0, 1, ..., N − 1, N = 2
q
and b
i
(x) is the i-
-th bit value of x. In this context, the Walsh functions
are arranged into sequential order, the number of zero
crossings of Walsh function per definition interval, to
obtain a set of basis functions. The number of zero
crossings increases with the order of basis functions
W = [φ
0
, φ
1
, ··· , φ
N−1
].
3 PROPOSED SEGMENTATION
METHOD FOR RESPIRATORY
SOUND SIGNAL
The proposed respiratory sound signal segmentation
approach is based on segmentation of the respira-
tory sounds using Walsh functions. The segmentation
method is based on the reconstruction/modification of
the analyzed signals by efficient linearly combined
Walsh functions. A simple decision scheme is then
followed for segmentation of our recorded respira-
tory sound signals based on the statistics of the mod-
ified/reconstructed signal. The details of our minimal
Walsh functions based segmentation method is pre-
sented here.
3.1 Modification of Signal
The modification of the input signal consists of two
stages - sinusoidal signal analysis (Arfib et al., 2002)
followed by our signal reconstruction scheme using
minimal Walsh functions.
3.1.1 Signal Analysis
The input signal x(n) is multiplied by a Hann win-
dow to yield successive windowed segments of x
s
(n).
These window segments are mapped into the spec-
tral domain by using FFTs. In this way, a time
varying spectrum X
s
(n, k) = |X
s
(n, k)|e
jϕ(n,k)
with n =
0, 1, ..., N − 1 and k = 0, 1, ..., N − 1 for each win-
dowed segment is obtained. Here, X
s
(n, k) denotes
the spectral component of the input signal at fre-
quency index k and time index n, while |X
s
(n, k)| and
ϕ(n, k) denote the time-varying magnitude and phase
responses, respectively.
3.1.2 Modified Signal Synthesis
The recorded input respiratory signal is reconstructed
as a modified sequence based on our modified anal-
ysis/synthesis approach. Prior to synthesis, each s-
-th windowed segment is modified as the weighted
sum of the magnitude |X
s
(n, k)| using binary Walsh
basis functions. Using basis functions, the number of
parameters required to track along the variations of
the inspiration and expiration phases of the noisy sig-
nal can be reduced. For this reason, SVD (Singular-
Value Decomposition) is used to determine the mini-
mal number of Walsh basis functions to be applied.
The detailed procedure for the identification of the
minimal number of Walsh basis functions and the new
modified basis function used based on the selected
basis functions, are described in the following sec-
tion. Applying the i-th basis function φ
i
, a modified
sequence, y
s
(n), for each windowed segment is then
obtained as
y
s
(n) =
N−1
∑
k=0
|X
s
(n, k)|.φ
i
(k) (2)
All the modified segments are finally concatenated
to generate an output signal y(n) having the time-
varying magnitude responses.
y(n) =
S−1
∑
s=0
y
s
(n − sN) (3)
3.1.3 Selection of Minimal Walsh Functions for
Modified Synthesis
It is very important to select appropriate basis func-
tions so that variations between the dynamics of
APPLICATION OF WALSH TRANSFORM BASED METHOD ON TRACHEAL BREATH SOUND SIGNAL
SEGEMENTATION
117

the two phases can be captured more precisely. A
method used to select the global natural scale in dis-
crete wavelet domain (Quddus and Gabbouj, 2002)
is adopted to determine the minimal number of basis
functions. This method adaptively selects the optimal
scale using SVD, while decomposition is being car-
ried out. Consider an input noisy respiratory signal x
of length V , and y
d
(ν) be its modified sequence ob-
tained by applying the basis functions of order d into
Eq(2) and Eq(3). Modified sequences {y
d
(ν)}
D−1
d=0
can
be represented as a matrix of size D × V . To de-
termine the order of basis functions with dominant
eigenvalues, the SVD of the D × V matrix is calcu-
lated adaptively begin with the first two orders (i.e.
φ
0
and φ
1
) while adding the Walsh functions of higher
orders.
Here, the proposed algorithm defines the minimal
order of basis functions N
min
as 3 throughout the sim-
ulations and found very robust against various situa-
tions. In the original algorithm (Quddus and Gabbouj,
2002), optimal scale is defined as the average of the
details from the first level to the natural scale, the level
associated with the dominant eigenvalue. However,
this averaging may introduce clipping effect for the
signals at low signal level. To avoid this effect, a shift-
ing operator which swaps the right and left halves of
the basis function coefficients is applied first. Then a
good estimate of a modified binary Walsh basis func-
tion within dominant eigenvalues is defined as
φ
m
=
φ
0
−
N
min
∑
i=1
CS(φ
i
)
max{|φ
0
−
N
min
∑
i=1
CS(φ
i
)|}
(4)
where N
min
= 3 is the largest order referring to the
most prominent eigenvalues and CS(·) is the shifting
operator. This new basis function φ
m
provides sharper
representation and higher discriminating features.
3.2 Decision Strategy
3.2.1 Preliminary Decision Module
First, 0-order basis function, φ
0
is used to produce a
modified sequence, y
0
(ν), to get the global informa-
tion of the original sample signals. This modified se-
quence is used as a reference or pilot sequence as used
in the areas of telecommunication. Containing the
local characteristics, another modified signal, y
m
(ν),
is formed using the new basis function φ
m
. From
this new sequence, locations and durations of inspi-
ration and expiration phases can be located more pre-
cisely even for adventitious respiratory sounds such
as wheeze and stridor. In this way, approximate loca-
tions of inspiration and expiration segments are first
determined from the modified signal, y
0
(ν). Then,
the results to determine respiratory phases can be im-
proved by using the second modified signal, y
m
(ν),
which contains the detailed information. Applying
the reconstructed signals y
0
and y
m
, the procedure of
detection scheme can be described as below:
• Extract two sequences of local minima, {α
0i
}
L
i=1
and {α
mi
}
L
i=1
, where L is the number of frames,
from every 4 ms frame of y
0
(ν) and y
m
(ν).
• Set thresholds, τ
0
and τ
m
, for each minima se-
quence which are obtained using a simple statis-
tics: τ
0
= µ
0
− κδ
0
and τ
m
= µ
m
− κδ
m
, where µ
0
and δ
0
are the mean and the standard deviation of
the first set of local minima, and µ
m
and δ
m
are
those of the second set of local minima while κ
is a positive value which depends on the dynamic
range of modified sequence y
0
(v).
• Set threshold coefficient, κ, which is the same for
τ
0
and τ
m
. As shown by Eq(5), κ is proportional to
global average of y
0
(v), and a is a constant value.
After experimenting with 10 reconstructed wave-
forms of different respiration types (stridor and
wheeze, normal tracheal breath for adult and in-
fant), a is found to be 3.4, and universal for all
types of tracheal breath sounds.
κ = a ×
1
N
N−1
∑
v=0
y
0
(v) (5)
• Declare a frame as an respiration frame if either
α
0i
<τ
0
or α
mi
<τ
m
. As it is mentioned earlier,
respiratory cycle is divided into four consecutive
phases: inspiratory phase, end-inspiratory pause,
expiratory phase, and end-expiratory pause. Res-
piration frames is defined in this context as the
frames belong to either inspiratory or expiratory
phases. In this way, the respiration frame indices
are obtained from y
0
(ν) and y
m
(ν) as R and T :
R = {r
1
, r
2
, ..., r
P
} (6)
T = {t
1
,t
2
, ...,t
Q
} (7)
• Combine the two initial boundary decisions as fol-
lows:
C = R ∩ T (8)
where C ={c
1
, c
2
, ..., c
J
} is the set of elements
common to R and T . Considering that the mem-
bers of C are the indices of either inspiration or
expiration frames, the final decision for detecting
respiration frames are obtained.
In the above, we decide that there exist respiration
frames whenever some or all of the prominent local
BIOSIGNALS 2008 - International Conference on Bio-inspired Systems and Signal Processing
118

minima obtained from the first modified signal y
0
(ν)
would coincide with the local minima found from
the second modified signal y
m
(ν). For those detected
frames when their corresponding local minima are not
obtained from both modified sequences of y
0
(ν) and
y
m
(ν), are discarded as outliers.
3.2.2 Refinement Scheme
Due to the quasi-stationary nature of the adventitious
respiratory sounds and their relatively small dynamic
range due to shallow breath, there are chances where
frames are wrongly identified because of the inflexi-
bility of the global threshold value used: small spikes
happen during end-inspiratory/expiratory pauses be-
ing wrongly identified as respiration segments which
are denoted by peaks; and small fluctuations during
inspiration/expiration might be wrongly identified as
pause segments which are denoted by troughs as in-
dicated in Fig.1(c). In order to ensure the accuracy of
the segmentation, the results obtained from the pre-
liminary decision module will be fine-tuned by the
refinement scheme to avoid wrong identification of
the respiratory frames. The scheme consists of two
stages:
• Identify error segments with durations shorter
than threshold σ
t
, where σ
t
varies for patients
with different respiratory rate. Since the duration
of end-inspiratory/expiratory pauses range from
0% to 30% and inspiration time range from 10%
to 80% of a complete breath cycle (Li, 2004), we
defined error segment to be with duration less than
5% of individual’s averaged breath cycle. There-
fore σ
t
is defined as:
σ
t
= 5% ×
60
RR
× F
s
(9)
where RR as Respiration Rate, is the number of
breath cycle per minute and F
s
is the sampling rate
of the signal. Since the averaged RR is the high-
est for infant which is 44 breaths/min (Keszler and
Abubakar, 2004), the scheme adopts this value to
minimize the wrong identification. The selected
parameter values are listed in Table 1. The er-
ror segments are then divided into error respira-
tion segments and error pause segments, where
the number of segments for each error segment
type is counted.
Table 1: Values of parameters for refinement scheme.
Parameter Value
F
s
8000 Hz
RR 44 breaths/min
σ
t
545 samples
• Evaluate the error segments based on segment du-
ration. This process is applied for evaluating error
respiration segments first. The procedure can be
described using our following pseudo code, where
respiration segment is denoted by R(s) and pause
segment by P(s) and s is the positional index of
the segment along time line.
Begin
T = threshold;
Pd(s) = duration of P(s);
Rd(s) = duration of R(s);
I = number of error R(s);
for i=1:I,
locate first error R(s);
if duration of Pd(s-1) & Pd(s) < T
if Pd(s) > Pd(s-1)
R(s) combine with R(s-1);
else
R(s) combine with R(s+1);
else if Pd(s-1) < T or Pd(s) < T
R(s) combine with R(s-1) or R(s+1);
else
R(s) is considered as pause segment;
end
end
End.
This procedure is then applied for the second time to
evaluate error pause segments by interchanging R(s)
with P(s) in the pseudo code.
4 EXPERIMENTAL RESULTS
4.1 Data and Parameter Selection
Five different types of tracheal sound signals are cho-
sen from (Lehrer, 1993) and (Wilkins et al., 2004).
Tracheal breath sound is chosen due to its relatively
larger amplitude compared with the sounds recorded
over chest. Also, it has distinct inspiratory/expiratory
phases and is related closely to respiratory flow.
The segmentation algorithm has been tested on to-
tal 10 sound signals, each consists of 8 breathing cy-
cles. Four phases are distinct in every breathing cycle
for all signals chosen. Since the segmentation method
is working based on the overall trend instead of the
detail fluctuations of the signals, the order m for re-
constructed signal y
m
(v) should be kept low. There-
fore, m = 3 is used in the experiments.
4.2 Illustrative Results and Analysis
Fig.1 illustrates the outputs of individual segmenta-
tion steps on a signal of inspiratory stridor and expi-
ratory moderate wheeze. Fig.1(a) shows the original
APPLICATION OF WALSH TRANSFORM BASED METHOD ON TRACHEAL BREATH SOUND SIGNAL
SEGEMENTATION
119
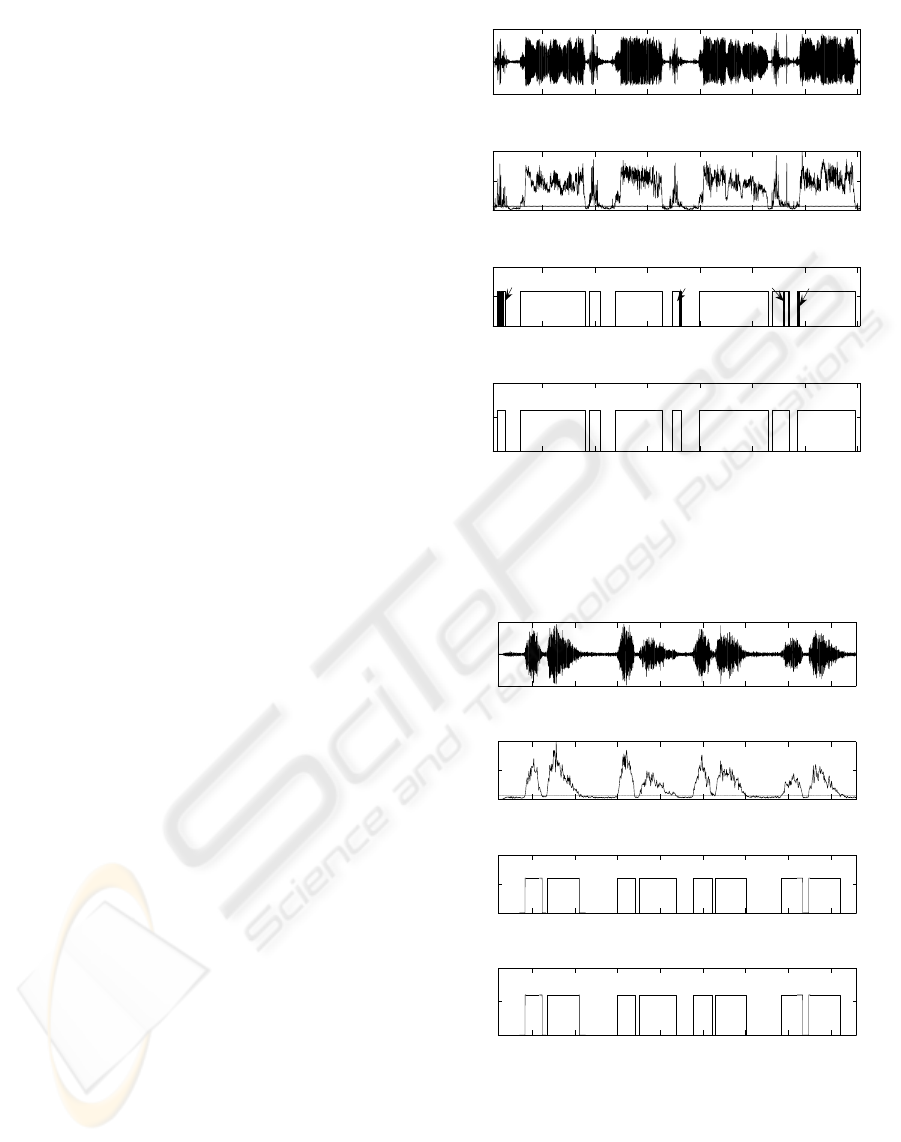
signal containing wheeze and stridor whereas Fig.1(b)
shows its transformed version, the reference modified
sequence y
0
(v), together with the reference threshold
τ
0
. In Fig.1(c), output of preliminary decision mod-
ule is depicted. As indicated by arrows A, B, C, D,
there are 4 locations of preliminary results containing
error segments. Being optimized by the refinement
scheme, the final segmentation result is displayed in
Fig.1(d).
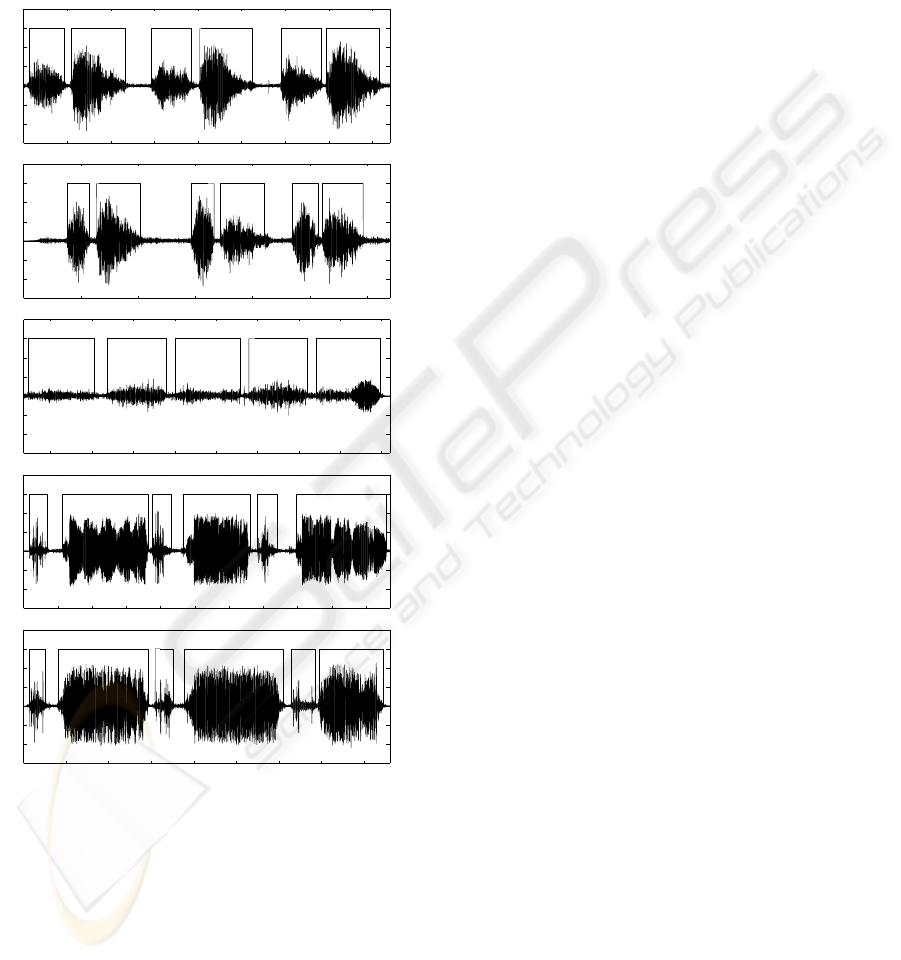
Also, the results for infant normal tracheal breath
are shown by Fig.2. By comparing these two figures,
no error segments are detected in Fig.2(c). This is
due to the different nature of the signals: The quasi-
stationary nature of wheeze and stridor signals gives
them more prominent components at low frequency,
while the fast transient nature of the normal tracheal
breath makes it emphasize more on the high fre-
quency components. Since y
0
(v) focusses on the sig-
nal trend which is represented by the low frequency
components, it captures more spikes (low frequency
details) for wheeze and stridor, but provides smoother
waveforms for normal breath sound signal. There-
fore, after thresholding by τ
0
, segments with short
duration are detected for abnormal breath sound sig-
nals. However, due to the optimization by refinement
scheme, the final segmentation results are equally ac-
curate for both normal tracheal breath sounds and ad-
ventitious breath sounds.
Moreover, illustrative results of the segmentation
algorithm for different types of respiratory sound sig-
nals are shown by Fig.3(a)-(e). These results demon-
strate the robustness of our proposed method on dif-
ferent types of tracheal breath.
5 DISCUSSION
In this paper, we have presented an algorithm to locate
and differentiate inspiratory/expiratory phases with
end-inspiratory/expiratory pauses for different types
of tracheal breath sounds. The use of binary Walsh
transform simplifies the proposed algorithm to a large
extend and left only few parameters for adjustment.
This makes the algorithm fast and automatic even in
the absence of any a priori information of the input
signal types. It performs equally accurate for both
normal as well as adventitious sounds due to the in-
corporation of refined decision module. Thus it is
more robust compared to existing methods as by using
these conventional methods, accurate segmentation is
still restricted within normal breath sounds.
As the only limitation, the proposed method does
not perform well on raw recorded tracheal breath
sound signals. This is due to the presence of the
2 4 6 8 10 12 14
x 10
4
−0.5
0
0.5
Original Expiratory Moderate Wheeze
2 4 6 8 10 12 14
x 10
4
0
0.5
1
0−order Modified Sequency with Threshold
2 4 6 8 10 12 14
x 10
4
0
0.5
1
Preliminary Segmentation Result
2 4 6 8 10 12 14
x 10
4
0
0.5
1
Samples
Final Segmentation Result
A
B
C
D
(a)
(b)
(c)
(d)
Figure 1: (a) Original signal waveform; (b)0-order modified
sequence y
0
(v) with threshold τ
0
; (c) preliminary segmenta-
tion result; (d) final segmentation result for inspiratory stri-
dor and expiratory moderate wheeze.
0.5 1 1.5 2 2.5 3 3.5 4
x 10
4
−0.5
0
0.5
Original Normal Infant Tracheal Breath
0.5 1 1.5 2 2.5 3 3.5 4
x 10
4
0
0.5
1
0−order Modified Sequence with Threshold
0.5 1 1.5 2 2.5 3 3.5 4
x 10
4
0
0.5
1
Preliminary Segmentation Result
0.5 1 1.5 2 2.5 3 3.5 4
x 10
4
0
0.5
1
Samples
Final Segmentation Result
(a)
(b)
(c)
(d)
Figure 2: (a) Original signal waveform; (b)0-order modified
sequence y
0
(v) with threshold τ
0
; (c) preliminary segmen-
tation result; (d) final segmentation result for infant normal
tracheal breath.
prominent heartbeat. Since the frequency range of
heartbeat is below 300Hz, it interferes with the nor-
mal breath sounds and contaminates the signal with
BIOSIGNALS 2008 - International Conference on Bio-inspired Systems and Signal Processing
120
large amount of low frequency components. This can
be solved by taking recording at positions with low
heart sound to respiratory sound amplitude ratio, or
preprocessing using a notch filter to suppress the ef-
fect of heartbeat. However, the algorithm is immune
to other ambient noises due to the wide spectrum oc-
cupied by the noises.
0 1 2 3 4 5 6 7 8
x 10
4
−0.4
−0.2
0
0.2
0.4
0.6
Samples
Normal Adult Tracheal Breath
0 0.5 1 1.5 2 2.5 3
x 10
4
−0.4
−0.2
0
0.2
0.4
0.6
Samples
Noraml Infant Tracheal Breath
3 3.5 4 4.5 5 5.5 6 6.5 7
x 10
4
−0.4
−0.2
0
0.2
0.4
0.6
Samples
Expiratory Mild Wheeze
0 1 2 3 4 5 6 7 8 9 10
x 10
4
−0.4
−0.2
0
0.2
0.4
0.6
Samples
Inspiratory Stridor and Expiratory Moderate Wheeze
0 1 2 3 4 5 6 7 8
x 10
4
−0.4
−0.2
0
0.2
0.4
0.6
Samples
Inspiratory Stridor and Expiratory Severe Wheeze
(a)
(b)
(c)
(d)
(e)
Figure 3: The segmentation results displayed with original
signal waveform for (a)-(b) normal tracheal breath of adult/
infant; (c) expiratory mild wheeze; (d)-(e) inspiratory stri-
dor and expiratory moderate/ severe wheeze.
REFERENCES
Arfib, D., Keiler, F., and Z
¨
oler, U. (2002). DAFX - Digital
Audio Effects. John Wiley Publisher.
Beauchamp, K. G. (1984). Applications of Walsh and Re-
lated Functions. Academic Press.
Cort ´es, S., Jan ´e, R., Fiz, J. A., and Morera, J. (Sept, 2005).
Monitoring of wheeze duration during spontaneous
respiration in asthmatic patients. IEEE Proceedings
of Engineering in Medicine and Biology, pages 6141–
6144.
Golabbakhsh, M. (2004). Tracheal breath sound relation-
ship with respiratory flow: Modeling, the effect of
age and airflow estimation. M. Sc. theses, Electrical
and Computer Engineering Department, University of
Manitoba.
Hossain, I. and Moussavi, Z. (2002). Respiratory air-
flow estimation by acoustical means. [Engineering
in Medicine and Biology, 2002. 24th Annual Confer-
ence and the Annual Fall Meeting of the Biomedical
Engineering Society] EMBS/BMES Conference, 2002.
Proceedings of the Second Joint, 2.
Hult, P., Wranne, B., and Ask, P. (2000). A bioa-
coustic method for timing of the different phases of
the breathing cycle and monitoring of breathing fre-
quency. Medical Engineering and Physics, 22:425–
433.
Keszler, M. and Abubakar, K. (2004). Volume guarantee:
Stability of tidal volume and incidence of hypocarbia.
Pediatric Pulmonology, 38(3):240–245.
Lehrer, S. (1993). Understanding lung sounds, Audio CD.
Saunders.
Li, T. (2004). Invasive mechanical ventilation. Respiratory
problems: Invasive mechanical trainee manual.
Meslier, N., Charbonneau, G., and Racineux, J. L.
(1995). Wheezes. European Respiratory Journal,
8(11):1942–1948.
Quddus, A. and Gabbouj, M. (2002). Wavelet-based cor-
ner detection technique using optimal scale. Pattern
Recognition Letters, 23:215–220.
Sierra, G., Telfort, V., Popov, B., Durand, L. G., Agarwal,
R., and Lanzo, V. (2004). Monitoring respiratory rate
based on tracheal sounds. first experiences. Annual
International Conference of the IEEE Engineering in
Medicine and Biology.
Sierra, G., Telfort, V., Popov, B., Pelletier, M., Despault, P.,
Agarwal, R., and Lanzo, V. (2005). Comparison of
respiratory rate estimation based on tracheal sounds
versus a capnograph. Annual International Confer-
ence of the IEEE Engineering in Medicine and Biol-
ogy.
Taplidou, S. A. and Hadjileontiadis, L. J. (2007). Nonlinear
analysis of wheezes using wavelet bicoherence. Com-
puters in Biology and Medicine, 37:563–570.
Wilkins, R. L., Hodgkin, J. E., and Lopez, B. (2004).
Fundamentals of lung and heart sounds, Audio CD.
Mosby.
Yadollahi, A. and Moussavi, Z. (2006). A robust method for
estimating respiratory flow using tracheal sounds en-
tropy. IEEE Transactions on Biomedical Engineering,
53(4):662–668.
APPLICATION OF WALSH TRANSFORM BASED METHOD ON TRACHEAL BREATH SOUND SIGNAL
SEGEMENTATION
121
