
INTEGRATION SOLUTION FOR THE ACCESS TO
HETEROGENEOUS MEDICAL DEVICES
Communication with Healthcare Devices in Intensive Care Units
Susana Martin-Toral, Jose Luis Rodriguez-Gonzalez
Computer and Information Technologies Division. CARTIF Foundation
(Centre for Automation, Robotics and Information and Manufacturing Technology)
Ave. Francisco Valles 204-205, Parque Tecnologico de Boecillo, Valladolid, Spain
Javier Perez-Turiel
Head of Biomedical Engineering Division, CARTIF Foundation
Keywords:
Medical devices, drivers, VITAL (Vital Signs Information Representation), manager/agent architecture, MDIB
(Medical Data Information Base).
Abstract:
This paper presents a free Critical Care Information System (CCIS) that shows an essential infrastructure for
critical care medical and nursing practice. Specifically, a Patient Integral Analysis Aid System (SAIP) in Inten-
sive Care Units (ICU) has been developed to cover the needs discovered in these scenarios. An importart part
of this system is related to medical equipment, that offers important information to help in medical diagnosis.
ICU patients are usually connected to several of these devices which register their physiological parameters.
The integration of these devices, in order to exchange the generated information, is difficult because they are
developed by different manufacturers and with different communication protocols and information represen-
tations. Due to this, it has been necessary to develop a set of communication drivers for each medical device,
according to the current regulations. To reach this objective, the developed drivers have a common interface
for the access and collection of medical device data. The main goal of the present paper is to show the work
done to obtain a real interoperability among medical devices from different manufacturers and with different
communication protocols in ICU services for automatic data collection, storage and retrieval.
1 INTRODUCTION
In this paper a free Critical Care Information Sys-
tem (CCIS) is presented. CCIS is an essential infras-
tructure for critical care medical and nursing practice.
This premise is described in terms of the critical care
environment, clinical decision making in critical care,
increasing demands for information about quality and
costs, and national initiatives for the sharing of health-
care information. This kind of systems are designed
to collect, store, organize, retrieve, and manipulate all
the data related to the care of the patient in Intensive
Care Units (ICU). Some of the main purposes of these
systems are: automated vital signs capture, cardiac
rhythm analysis and dysrhythmia detection, reporting
laboratoryresults, entry and transmission of physician
orders, admission, discharge and transfer of patients,
calculation of medication doses, fluid infusion rates,
shift, and daily intake and output volumes, organiza-
tion of patient records, calculation of patient plan of
care, entry and organization of care documentation
and prompting the caregiver for recorded documen-
tation (Adhikari and Lapinsky, 2003; Fraenkel et al.,
2003; Frize et al., 1997). In this research project a
Patient Integral Analysis Aid System (SAIP) in Inten-
sive Care Units (ICU) has been developed, which is
now being used in the ICU of the University Clinical
Hospital of Valladolid, in Spain.
The SAIP is a system based on free software GNU
GPL (General Public License) (Ope, 2007) composed
by a set of computer applications to facilitate and im-
prove the attention received by the patient in inten-
sive care units (Martin et al., 2004; Jose, 2007). It
provides a support system to collect, store and man-
age the clinical information in the ICU, with the pur-
pose of facilitating the daily medical routine and to
improve the quality of the attention provided to the
patient by overcoming the actual difficulties of inter-
247
Martin-Toral S., Luis Rodriguez-Gonzalez J. and Perez-Turiel J. (2008).
INTEGRATION SOLUTION FOR THE ACCESS TO HETEROGENEOUS MEDICAL DEVICES - Communication with Healthcare Devices in Intensive
Care Units.
In Proceedings of the First International Conference on Health Informatics, pages 247-253
Copyright
c
SciTePress

connection and storage (Shortliffe, 2001).
The ICU patient is, habitually, connected to one or
several devices - called in this paper medical devices
- that allow information on several of their physio-
logical parameters to be measured, as shown in figure
1 with a vital signs monitor. These devices generate
a great amount of information, but their capacity of
storage is limited. In addition, they are usually from
different manufacturers and models, and they are not
interconnected with the rest of the devices. That is
why the integration of the generated information is
difficult. This heterogeneity of medical devices is one
of the main problems for making an integral system
for the ICU. Each device has its own communica-
tion protocol and its own connection interface, for
example, RS-232, Ethernet, MIB (Medical Informa-
tion Bus), etc. and there is no interface or protocol
that allow the unification of communication and ac-
cess between different devices and a user application
that wants to communicate with them. In order to
solve this problem, the developed system unifies, for
each type of medical device, the data obtained from
the different medical devices that compose the sys-
tem, by using diverse standards of denomination and
storage.
Figure 1: Monitor connected to the ICU room PC.
The initial situation in the ICU consists of a series
of medical devices, such as infusion pumps, respira-
tory ventilators and vital signs monitors, each with
a different type of connection, a different communi-
cation protocol and without a common interface that
allows homogeneous access to the data that these de-
vices provide (Martin et al., 2004; Jose, 2007). Due
to this, it has been necessary to develop a set of com-
munication drivers for each medical device that al-
low the information provided by the medical devices
be collected and stored automatically, although these
are from different manufacturers, as well as the infor-
mation contributed by the medical staff. Because of
that, the drivers developed for the SAIP system have
a common interface for the access and collection of
data from the medical devices.
Although the main objective of the present paper
is to show the work done to obtain the homogeneous
interoperability between medical devices in the ICU,
additional objectives of the SAIP system (Jose, 2007)
are summarized as follows:
- Automation of the medical workflow: electronic
management of documents.
- Collection and storage of other types of manu-
ally acquired information: medical devices with-
out possibility of automatic capture of informa-
tion, connectionless devices and data from the pa-
tient exploration task filled in directly by medical
staff.
- Calculation of medical statistical indexes:
APACHE, NEMS,etc.
- Consultation of registered information. The infor-
mation stored in the system is readily accessible.
- Document elaboration of patients’ management
(registries, personal information, etc).
- The SAIP must comply with the National medical
information security laws.
- Interchange of data with other hospital services.
The intensive care unit is not an isolated service,
so it needs constant communication with other
hospital services. The efficient implementation of
defined interfaces should ensure communications
between the diverse systems/services of the hos-
pital.
- To manage a safe and trustworthy access to the
system. Most of the information generated in hos-
pitals is personal medical information and there-
fore is confidential.
- Development under the concept of free software
(GPL license). The development of applications
based on free software is an area of activity of ever
growing interest that generates numerous expecta-
tions, given the ample possibilities it offers.
The rest of this paper is organized as follows : sec-
tion 2 describes the proposed control architecture of
the SAIP system in the ICU, paying special attention
to the part related to the integration of medical de-
vices. Section 3 describes the communication drivers
developed to allow the medical devices to commu-
nicate with the SAIP System. In addition, it de-
scribes the dynamic libraries of plugin type solution
proposed. Section 4 describes the agent entity whose
function is to communicate with the different medical
devices with its associated database. This database
stores the device data. In section 5 the results of the
system development are presented. Finally, a sum-
mary of the work done and some conclusions are in-
cluded in section 6.
2 ARCHITECTURE SOLUTION
The SAIP is a system based on the use of computer,
control and communication technologiesto generate a
set of computer applications whose main objective is
to ease and improve the attention received by patients
in intensive medical services. From a physical point
of view, the planned system requires the connection
of medical devices (vital signs monitors, ventilators,
infusion pumps, etc.) to external elements, the instal-
lation of computer systems and communication net-
works, and the development of software applications
for data recording, storage, processing and access.
The proposed system architecture is based on a
manager/agent framework, and in general it can be
seen as a three layer architecture (data, business logic
and presentation). Furthermore, the system function-
ality has been divided in two different parts: the in-
tegration environment and the execution environment
or healthcare information system (HIS) (Scherrer and
Spahni, 1999; Martin et al., 2004).
In general, the aim of the integration environ-
ment is to unify the information obtained from ev-
ery kind of system device (both medical and com-
puter). To achieve this objective, several network de-
vice manager frameworks have been used (Leinwand
and Fang, 1995), such as the ones based on the OSI
(Open System Interconnection) interconnection basic
reference model or the ones based on SNMP (Sim-
ple Network Management Protocol) (Stallings, 1999;
Case et al., 1990). On the other hand, the execution
environment, or HIS environment, is the one in charge
of implementing the business logic, so it develops
the thickness functionality provided by the SAIP. The
modules that form the HIS environment are located
throughout the diverse physical devices that house the
application, based on the information type they han-
dle. This information is provided by both the integra-
tion environment and users, or through other appli-
cations and external systems (admission information,
laboratory results, etc.). Therefore, the execution en-
vironment has the elements needed to process the in-
formation and to provide the functionality required by
users.
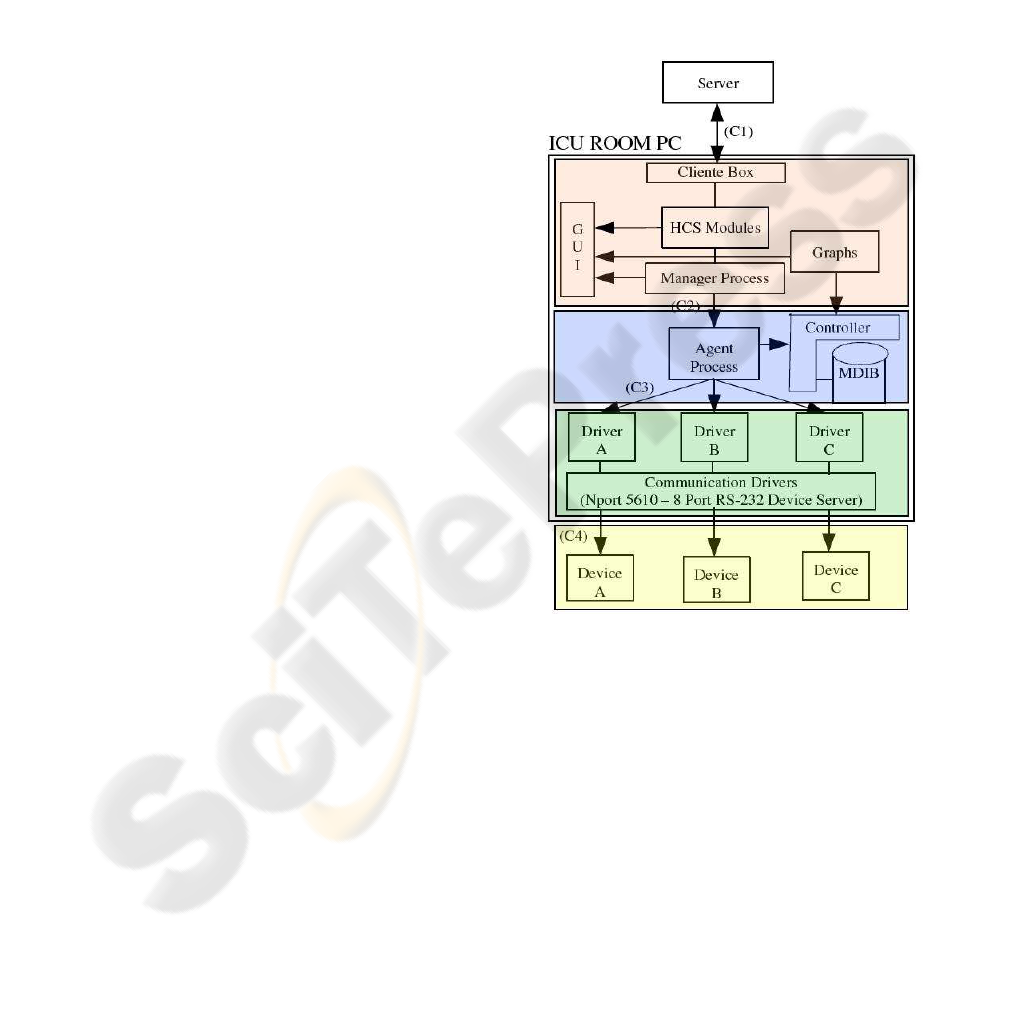
From this architecture, the present work empha-
sizes the part dedicated to the communication and
information processing provided by medical devices,
according to norms (CEN/CENELEC, 1993; CEN,
2000). The goal pursued in this aspect is to have a
system that allows the interaction with patient vital
support devices, so as to make the data and alarms
generated by these devices available for users (doc-
tors, nursing staff, nursing assistant, etc.). Since
these medical devices are in the patients’ emergency
rooms, the computer equipment entrusted to interact
with them must also be located in the same emer-
gency rooms. This IT equipment (pesonal computer)
is called, in our system, ICU room PC. The ICU room
PC architecture is shown in figure 2, and its main
characteristics will be detailed in the rest of the sec-
tion.
Figure 2: Block diagram of ICU Room PC.
For the ICU room PC connection architecture, the
main objective of the integration environment is to
unify, for every type of medical device and as far as
possible, the data obtained from the different devices
that compose the system. This environment, there-
fore, converts and translates the hardware dependent
information provided by medical devices into an an-
notation and nomenclature understandable by all the
devices. Moreover, it also unifies the way in which
the calls are made to access information. In this way
an integrated and homogeneous medical device man-
agement is obtained.
With these objectives, the integration environment
uses some parts of the VITAL norm (Vital Signs In-
formation Representation) (CEN, 2002) to define the

semantics of the information provided by medical de-
vices as a structured set of objects and methods to rep-
resent medical information. The VITAL experimental
norm provides the definition of an independent com-
mon device representation of vital signs information,
and the definition of a common model for accessing
to this information. It means that VITAL looks for
real interoperability between medical devices even if
they are from different manufacturers (CEN, 2002).
In general, the information provided by medical
devices is transformed into VITAL nomenclature to
be stored in a database called MDIB (Medical Data
Information Base). An agent entity is responsible for
updating this database, which in addition attends to
the requests made by a manager entity, as can be seen
in detail in section 4. In short, the integration environ-
ment needs:
- A set of drivers that allow communication with
diverse medical devices. Each one is device de-
pendent, so they must speak the same language as
the device they access.
- The translation of device dependent information
into VITAL nomenclature.
- An agent entity that gathers this information peri-
odically.
- A database where information is stored.
In figure 2 the connection schema of the elements
housed in the ICU room PC is shown. Three differen-
tiated groups are distinguished in this schema. From
the lower level of abstraction to the upper, firstly the
set of drivers can be seen, then the agent entity and
its related database, and finally the business logic and
the graphic user interface housed in the ICU room PC.
Each of these groups is presented in detail in the fol-
lowing sections.
3 COMMUNICATION DRIVERS
Drivers are programs in charge of serving as middle-
wares between the computer operating system and the
different elements connected to it. In this particular
case, the system works with two different kinds of
drivers, as can be seen in figure 2. The first one fits the
definition given before, and is called “communication
driver” in the figure. This driver allows the communi-
cation with medical devices through a communication
element. Currently, the system works with a unique
communication driver, that is, a serial port hub of
Moxa trademark (Moxa’s NPort 5610 8 Port RS-232
Device Server). The reason is that almost all the med-
ical devices provide their output through an RS-232
interface, so we have chosen to work with this type
of device server, that allows a greater the number of
RS-232 interfaces than a conventional computer. Per-
haps in the future the system could need other types
of drivers for medical device communication, maybe
through Ethernet or MIB (Medical Information Bus)
interfaces.
The second driver type presented in the schema is
related to special programs developed to implement
the communication protocol of each medical device.
Therefore, there must be a driver for each type and/or
model of medical device. These drivers can be seen as
translator gateways, since they translate data requests
from the agent entity, who makes them in a homo-
geneous way, into a language understandable by the
corresponding medical device, and then they respond
in a standard VITAL format. In this way the agent
entity can talk to the different devices using the same
language, and without worrying about which device it
is talking to. The main objectives of these drivers are:
- To implement the communication through the se-
rial port (extendable to other communication in-
terfaces).
- To implement the proprietarycommunication pro-
tocol of each medical device.
- To attend to manager entity requests.
- To translate the information provided by devices
into VITAL format.
In this work, a plugin is considered a driver im-
plemented for every type or model of medical device
(the second type of driver seen before), since its com-
pilation is made as plugin libraries that can be loaded
later by an agent entity. These plugins have been de-
veloped using the same interface, so the agent can call
their functions in a homogeneous way and without
the need to know the device with which it works, or
from which manufacturer it is. In this way, the system
is totally scalable in order to increase the number of
medical devices to work with, and it ensures the com-
munication with heterogeneous devices from diverse
models and manufacturers.
When the incorporation of a new medical device
is needed in the ICU, and whenever the new device
presents some external communication port and pro-
tocol, it will be enough to implement the appropriate
driver (filling the specified interface and VITAL rep-
resentation), to generate the plugin library and to in-
form to the agent entity about the new plugin name
and location. Once the plugin is incorporated into the
system, the agent entity will be able to communicate
and extract information from this device.
4 AGENT ENTITY AND ITS
RELATED DATABASE
The agent entity is the element in charge of the com-
munication with the different medical devices (con-
nected to the ICU room PC by the serial ports hub)
through the corresponding plugins. Its main target is
to collect the information as well as the alarms pro-
vided by the different medical devices, to be mon-
itored and validated. Every agent entity communi-
cates with the medical devices assigned to a specific
patient and, with the data provided by them, must fill
in the database named MDIB, and must respond the
requests from a manager entity. Therefore at this level
it is a manager/agent architecture.
The main functionalities of the agent entity are:
- To detect the connection of a new medical device
in the serial port hub assigned to one ICU room
and one patient. This detection is carried out by
the own hub, which is able to send an SNMP trap
to the ICU room PC indicating the status changes
in DCD and DSR signals in each hub’s port.
- To identify the connected medical device, that
is, to detect the type of device the agent entity
must work with to use the suitable plugin. With
this aim, the agent entity loads every plugin and
checks if it exists an appropriated communication
with the device related to the plugin. If the de-
vice responds its plugin will have been detected,
and therefore the agent entity will know the type
of device which it works with.
- The previous items provide the system with a
plug-and-play functionality related to the connec-
tion of medical devices to the system. This func-
tionality simplyfies the connection of these medi-
cal devices to the nursing staff.
- To collect periodically the data provided by these
devices, and update the MDIB with them.
- To detect alarm conditions in the devices using
pull or push methods, according to the behavior
of each one.
- To notify the detected alarms to the adecuated el-
ement of the systems for its processing and broad-
cast.
- To attend the requests of the manager entity, that
must ask for and provide the information from
medical devices to the business logic layer, to be
processed and showed to system users.
The MDIB, database containing the information
provided by medical devices, has an information
model according with a part of the structure and
nomenclature of the VITAL norm. This part is used
to represent the different information objects. Either
the agent entity, or other modules and elements, could
need to access to the MDIB database.
5 MAIN RESULTS
In order to understand the obtained results it has to
be considered the scenario where the project has been
developed:
- Each ICU room has a ICU room PC.
- An ICU room can have more than one patient.
- For each patient there is an agent entity and a
MDIB associated to it. Therefore in each ICU
room PC there will be so many agent entities and
MDIB as patients are in the ICU room.
- All the data gathered during a patient’s stay in the
ICU is stored in the MDIB.
- This MDIB is filled in a periodical way. In every
period the data collected by the drivers is used to
fill the database.
- When a patient leaves the service, and therefore
the system, the data stored in the MDIB relatec to
that patient is erased.
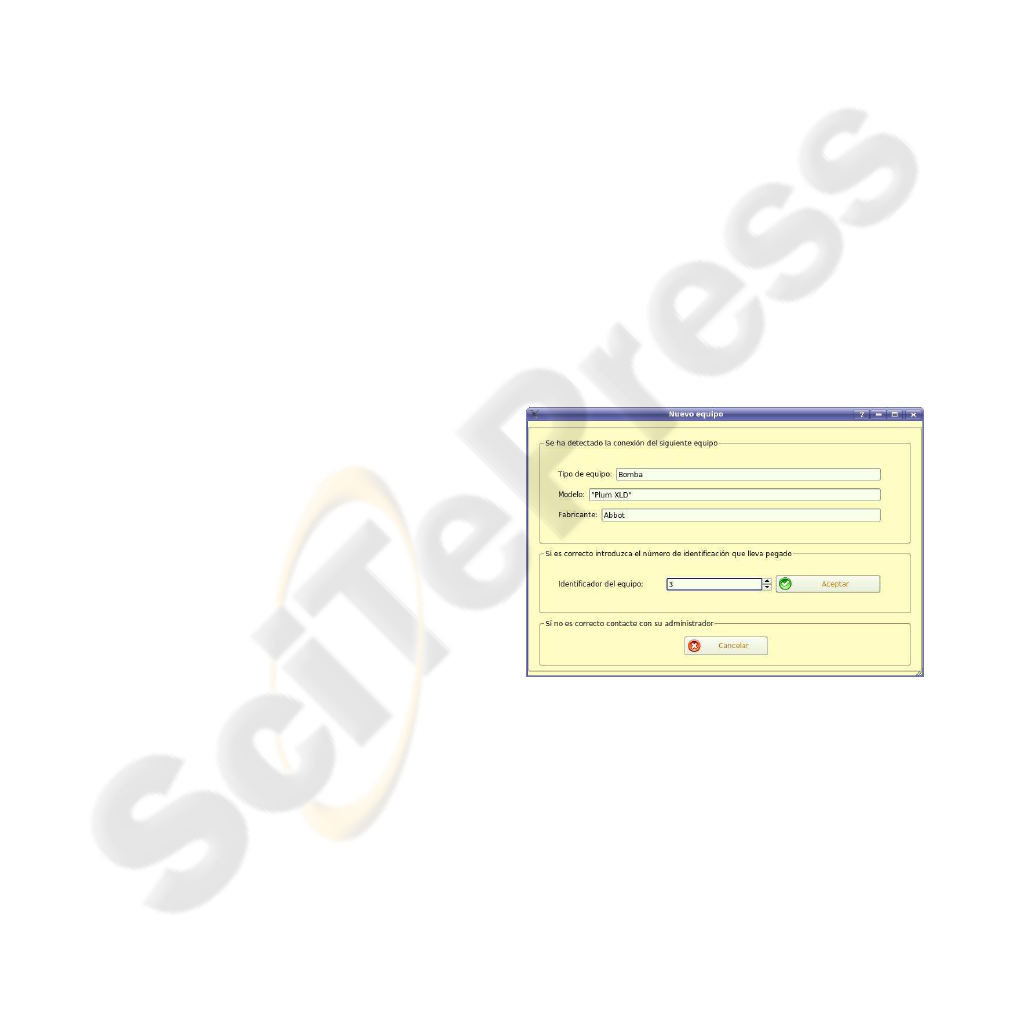
Figure 3: Device identification screen.
- The agent entity must be always active, waiting
for the connection/disconnection of a medical de-
vice, even if there is no patient in the room.
- When there is no patient in the room and a device
is connected, the agent assumes that there is a new
patient in the room.
- Whenever a device is connected, if the agent is
able to recognize it, a screen appears indicating
the device detected (type of device, manufacturer,
etc.). If the displayed data is correct, the user must
introduce the number that identifies that device
univocally, as it is shown in figure 3.
- The agent monitors each device using its sam-
pling period. The data is stored periodically in
the MDIB of the ICU room PC, whereas the de-
tected alarms are sent to the appropriate process
to be handled. An example of an alarm originated
by an infusion pump is shown in the next listing
(taken from the standard output):
Hilo alarmas: Se ha detectado 1 nueva
alarma en el equipo 3
----------------------------------------
Identificador de dispositivo: 3
---> Hilo alarmas: ALARMA 0:
Equipo: Bomba
Modelo: "Plum XLD"
Descripcion: Fallo en cassette.
Tipo de alarma: tecnica
Prioridad: baja
Fecha de produccion: 22/06/2007
Hora de produccion: 08:14:32
----------------------------------------
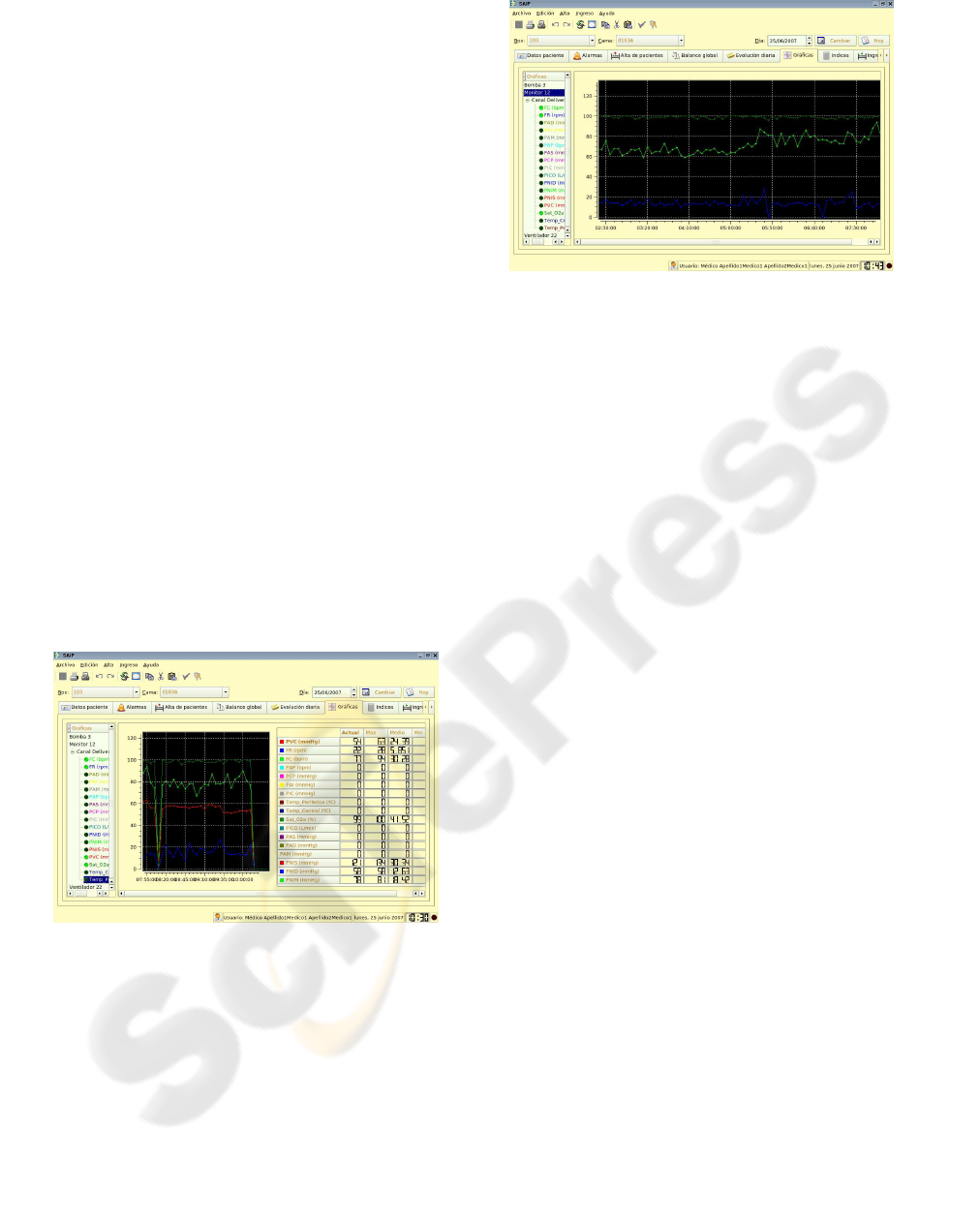
- Once the data is stored in the MDIB, the medical
staff has the possibility of visualizing it as graphs
(trend curves) corresponding to different physio-
logical signs from the medical devices. Two ex-
amples of these trend curves can be seen in figures
4. and 5. Only the vital signs with a green spot are
showed in the graph.
Figure 4: Trend curves from patient monitor data.
- When the patient leaves the service all the medi-
cal devices must be disconnected, while the agent
entity waits for the arrival of a new patient.
During the project, the following medical devices
communication drivers have been developed, tested
and included into the system:
- Lifecare XL Infusion Pump from Abbott Labora-
tories.
- Evita Ventilator from Drager Medical.
- Vital signs monitor from Agilent Technologies.
Figure 5: Detail of trend curves.
The software developed in this project has been
implemented using the C++ language and the Troll-
tech’s QT library (Tro, 2007).
6 CONCLUSIONS
In this paper it has been presented the components
of the SAIP system developed to interact with medi-
cal devices (vital signs monitors, ventilators, infusion
pumps, etc.) in charge of the patient’s vital support in
Intensive Cares Units (ICU). The details of the com-
ponents of the ICU room PC architecture, being part
of the global SAIP system, have been shown. It has
been necessary to develop communications drivers
with a common interface to facilitate the connection
to the different devices in a uniform way, and the ac-
quisition of the data provided by the medical devices
following the indications of the medical staff respon-
sible for the ICU. These communication drivers have
been developed as plugin libraries to allow the SAIP
application to manage them through an agent entity,
while only those corresponding to medical devices
connected to the patient are loaded and used.
On the other hand, once the data of the medi-
cal constants of each device are gathered and trans-
formed into VITAL nomenclature, they are stored in
the MDIB of the corresponding ICU room PC. This
allows to visualize as graphs (trend curves) the values
stored for the different medical devices. These graphs
allow the medical staff to see the evolution of the dif-
ferent medical signs provided by the devices during a
complete cycle of 24 hours, or the ones stored for any
day of the stay of the patient in the ICU.
Considering the implementation and the be-
haviour of this part of the system, the benefits and
remarkable advantages related to the handling of in-
formation provided by the medical devices are:
- Automatic and periodical collection of values of

vital signs, avoiding the manual introduction of
these values in the system.
- Automatic collection of the alarms produced by
these devices and diffusion for the knowledge of
the medical staff of the ICU service.
- Storage of all this information. Capacity to con-
sult data of different stages from the beginning of
the stay of a patient. Usually medical devices do
not have the capacity to store the information gen-
erated during all the stay of the patient in the ICU.
Some of them have buffers of storage, but they are
not big enough to store all the information relative
to the complete entrance of the patient.
- Plug-and-play functionality, that simplifies the
use of the system for communicating with the
medical devices, specially for the nursing staff.
- Automatic collection of the constants indicated in
the treatment, always with the corresponding val-
idation of the nursing staff. Obtaining of nursing
reports relative to these constants.
- Taking of values for semi-automatic generation of
balances.
- Generation of trend curves.
- Compilation of the information in a unique and
standard format that facilitates its integration
and handling and provides a real interoperability
among devices.
- An application that facilitates a joint visualization
for the generation of diagnoses with all the infor-
mation of several medical devices.
As it can be seen, the main purpose of the sys-
tem is to facilitate the collection, storage and subse-
quent processing of the information provided by the
medical devices connected to patients in the intensive
care units in an homogeneous and standard way. The
automation of the collected data has been possible to
make it available to the medical staffin a friendly way,
and a real interoperability among heterogeneous me-
dial devices has been obtained.
ACKNOWLEDGEMENTS
This work has been funded by the SACYL (Sanidad
Asistencial de Castilla y Leon - Health Welfare
of Castilla y Leon), through agreement of collab-
oration between the University Clinical Hospital
(HCU) of Valladolid and the Centre for Automation,
Robotics and Information and Manufacturing Tech-
nology (CARTIF Foundation). We appreciate the col-
laboration of the intensive medicine staff of the HCU
and the CARTIF development team involved in the
project.
REFERENCES
(2007). Open soruce home page. URL:
http://www.opensource.org. Last visit: june 2007.
(2007). Trolltech home page. URL: http://trolltech.com/.
Last visit: june 2007.
Adhikari, N. and Lapinsky, S. E. (2003). Medical informat-
ics in the intensive care unit: overview of technology
assessment. Journal of Critical Care, 18(1):41–47.
Case, J., Fedor, M., Schoffstall, M., and and, J. D. (1990).
RFC 1157 - Simple Network Management Proto-
col (SNMP). Technical report, Network Working
Group. URL: http://www.faqs.org/rfcs/rfc1157.html.
Last visit: june 2007.
CEN (2000). ENV 13735:2000. Health informatics - Inter-
operability of patient connected medical devices. Eu-
ropean prestandard. English version.
CEN (2002). CEN/ISO ENV13734. Health informatics.
Vital signs information representation. European pre-
standard.
CEN/CENELEC (1993). IEC 60601-1. Medical electrical
equipment. General requierements for safety. Euro-
pean standard.
Fraenkel, D. J., Cowie, M., and Daley, P. (2003). Quality
benefits of an intensive care clinical information sys-
tem. Critical Care Medicine, 31(1):120–125.
Frize, M., Trigg, H., Stevenson, M., and Solven, F. G.
(1997). Decision-support systems for critical care.
In American Medical Informatics Association Confer-
ence.
Jose, S. S. (2007). Modelado y desarrollo en software li-
bre de un sistema de analisis integral de pacientes en
unidades de cuidados intensivos. In FSWC 2007: Free
Software World Conference 3.0.
Leinwand, A. and Fang, K. (1995). Network Management,
a practical perspective. Addison Wesley, London, 2nd
edition.
Martin, S., Gutierrez, S., Jose, S. S., and Barrientos, F.
(2004). Sistema de ayuda al analisis integral de pa-
ciente en unidades de cuidados intensivos (SAIP). In
INFORMED 2004, X Congreso Nacional de Informat-
ica Medica. El tratamiento de la informacion, instru-
mento de valor aadido en la practica medica, pages
185–192. SEIS, Sociedad Espaola de Informatica de
la Salud.
Scherrer, J. R. and Spahni, S. (1999). Healthcare infor-
mation system architecture (HISA) and its middle-
ware models. In AMIA Symposium, 1999 - amia.org.
AMIA: American Medical Informatics Association.
Shortliffe, E. H. (2001). Medical Informatics. Com-
puter Applications in Health Care and Biomedicine.
Springer, New York, 2nd edition.
Stallings, W. (1999). SNMP, SNMPv2, SNMPv3, and
RMON1 and 2. Addison Wesley, London, 3th edition.
