
When Smart Home Meets Pervasive HealthCare
Services Using Mobile Devices and Sensor Networks–
Status and Issues
Ti-Shiang Wang
Nokia Research Center
5 Wayside Road, Burlington, MA 01803, USA.
Abstract: In this paper, to deliver healthcare service pervasively, especially to
the home space, we first discuss the status and activities on healthcare infra-
structures and systems using mobile devices and sensor networks. We also pro-
vide the information and illustrate the reasons why home healthcare will be
even more hot space in the near future. With the advance of wireless network,
mobile devices become more demanding for users to communicate each other
either for voice or data service, or both. In addition, as medical record goes to
digital form and will be available any where, any time and used by any kind of
mobile devices, so that mobile healthcare becomes a hot topic and many issues
are currently working on. From the user side point of view, advanced sensing
devices and networks based on them provide rich context and seamless connec-
tion between users and mobile devices so that the personal data or medical re-
cord could be updated as needed and quality of services can be improved. With
the help of smart sensors and sensor networks embedded either on body or in
the home space, the quality of personal healthcare can be improved in lower
cost as well. In this paper, we also address some issues to implement the home-
based pervasive healthcare applications and provide a visionary scenario inte-
grating smart home and healthcare services.
1 Introduction
Healthcare institutions today are attempting to respond to demands to reduce cost and
improve the effectiveness of care delivery. Spurred by a combination of economic
and regulatory pressures (such as Health Information Portability and Accountability
Act, HIPPA) [1], hospitals and healthcare providers want new solutions that can ad-
dress core business needs and manage the huge volumes of time- and security-
sensitive data that they are involved.
With the popularity of mobile devices and pervasive deployment of wireless net-
wo
rks, the gateway of healthcare service become closer to patients so that the patients
can control the autonomy and smart home/healthcare gets involved. In other words,
patients and healthy people can do the basic control and monitoring by themselves.
From mobile device’s point of view, personal digital assistants and mobile phones are
Wang T. (2005).
When Smart Home Meets Pervasive HealthCare Services Using Mobile Devices and Sensor Networks– Status and Issues.
In Proceedings of the 2nd International Workshop on Ubiquitous Computing, pages 67-74
DOI: 10.5220/0002560300670074
Copyright
c
SciTePress

cheap and effective, and run a wide variety of applications. Many people simply bring
their own PDAs to work. As technology continues to reshape the way hospitals de-
liver care, doctors, nurses, and other clinicians need access to patient information
from any location and at any time. Although many hospitals have integrated their
various information systems, delivering clinically relevant patient information, for
example, electronic medical record (EMR) [2], to healthcare professionals – when,
where, and how it is needed – still poses a major challenge. Services from caregivers
to the patients or users are related to the data rate of the services, which is a key crite-
ria used for both wired and wireless network and technology deployed in the health-
care environment. Even with patients (either sick ones or/and healthy ones) have
them for well-being or daily monitoring. The range of data rates of typical devices
used in the telemedicine can be scaled from several kbps up to tens of Mbps [3].
Mobile healthcare encompasses the range of mobile technologies as they are ap-
plied in healthcare, wireless network infrastructure, mobile devices and mobile appli-
cations. It is an extension of, but not a replacement for, desktop computing. The po-
tential benefits of mobile healthcare include point-of-care communication, improve
clinical decision-making, enhanced quality of care, reduced medical errors [4], im-
proved information access and exchange, improved accuracy, diminished redun-
dancy, diminished paperwork, increased time for patient care, and improved integra-
tion. In Addition, mobile healthcare supports public safety initiatives and reduces cost
while improving efficiency. Mobile healthcare aims to give users (either patients or
physicians) a more active role in the healthcare process while at the same time health-
care payers are able to manage costs more directly. The benefits of mobile healthcare
computing are to provide point-of-care communication, to offer information access
and exchange, to diminish paperwork, to improve accuracy and efficiency, to im-
prove clinical decision-making, and to promote integration. XML and web service
technology [5, 6] have also been consider to apply in healthcare sectors to provide
sharing, interoperability and availability of medical data or records.
On the other side, the pervasive computing technologies can be of use on the user
sides not only to support healthcare, health and wellness management, but also to
make healthcare available everywhere and any time, pervasively, especially in the
home. It is envisioned that this concept of computing anywhere can be applied to
support users in their own home environment, so that the activities around the home
can be monitored, under control and make proactive decisions to better serve the
occupants by enabling context-awareness instead of being solely reactive to their
commands. For home-based healthcare, personal wellness systems are not meant to
replace the mainframe system of hospitals, clinics and physicians but rather to put
seniors and activities of daily living more squarely into the healthcare mix. Espe-
cially, systems that encourage seniors to maintain physically fitness, nutrition, social
activities, and cognitive engagement so they can function independently in their own
home for as long as possible can help address the social and financial burdens of an
aging population.
To make the home to be smart to provide suitable services, sensors and sensor
network will play an important role to make it happen. Basically, pervasive healthcare
techniques consist in embedded sensors to continuously monitor people’s home activ-
ity, which is analyzed to provide global health information. Nevertheless, in such
systems, support is limited to a closed environment, and sensing of vital signals is not
68
possible. These signals sensed mostly are physiological information. In the future,
both of physiological rhythms and behaviors of the own of the house will be consid-
ered in the pervasive healthcare. The sensed data can be integrated in the database
and arrange it in a generalized XML format, which allow the exchange with medical
institutions where a system manages the database for each patient’s vital signals, so
that the advanced web service technologies can be applied.
2 Mobile Healthcare Projects/Programs
Mobile healthcare activities have been very active because wireless network is perva-
sively deployed and mobile devices are mature enough to provide an important com-
ponent in healthcare sectors. Mobile healthcare application can be viewed an exten-
sion of the use of telemedicine [7, 8] to support the healthcare in mobile manner and
remotely. In other words, mobile healthcare can be considered the first step towards
pervasive healthcare application, since it is mainly focused from the healthcare or
caregiver side. In this section we list some projects (but not an exhaustive list) that
have been proposed in the area of mobile healthcare applications. In general, sensor
based network with mobile devices (such as mobile phones or PDAs), Internet, wire-
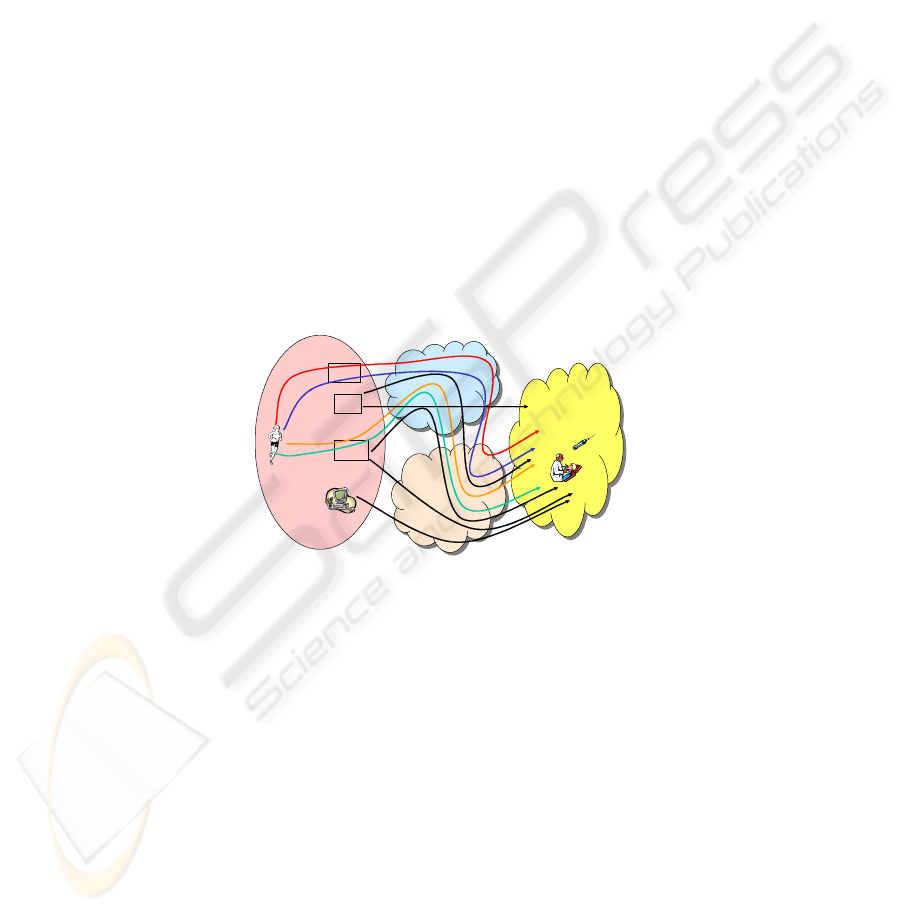
less networks and medical record center are major network components. Fig. 1 is
shown for network domains for mobile healthcare projects discussed in this section.
GSM/GPRS/
UMTS
PDA
MP
Internet
Medical
Data
Center
Host
AMON
A
M
B
U
L
A
N
C
E
MobiHealth
GPRS/TeleMed
DITIS
D
I
T
I
S
DITIS
D
I
T
I
S
DITIS
Fig. 1. Architectures of proposed mobile healthcare projects
Advanced care & alert portable telemedical MONitor (AMON) [10] system is a
wearable personal monitor medical device that evaluates human vital signals using
several kinds of advanced biosensor. The system gathers and analyzes the vital in-
formation and transmits the data to a remote telemedicine center for further analysis
and emergency care, using cellular infrastructure.
MobiHealth project [9] funded by European Commission aims at introducing mo-
bile value-added services in the healthcare using 2.5G (GPRS) and 3G (UMTS) tech-
nologies. A sensor-based network, called body area network (BAN), enabling the
integration of different sensors and actuators, is presented and has been prototyped in
the first phase of the project. The BAN was connected to the public GPRS and UMTS
networks, using iPAQ and Ericsson mobile phone as gateway to connect to Internet.
69

In [11], this project was partially supported via the Cyprus Telecommunication
Authority (CYTA), the Research Promotion Foundation of Cyprus (project IASIS),
and the University of Cyprus. In this project, a practical evaluation of the perform-
ance of the GSM and GPRS systems in the transmission/reception of X-ray images
and videos in emergency orthopedics cases was carried out. The results presented in
this study were carried out using the Compaq iPAQ 3870 handheld PC equipped with
GSM/GPRS expansion pack modem.
In AMBULANCE project [12], it consists of mobile unit and consultation unit.
GSM link was used to connect these units. The device uses GSM links and allows the
collection and transmission of vital bio-signals, still images of the patient, and bi-
directional telephoning capability. The mobile unit mainly consists of two compo-
nents, a Johnson&Johnson Dinamap Plus III bio-signal monitor used for bio-signals
acquisition and a portable PC. The consultation unit mainly consists of a dedicated
workstation as a processing terminal in the hands of the acting expert doctor to sup-
port an emergency case.
DITIS [13] is a member of the MEMO cluster project. DITIS is an Internet (web)
based Group Collaboration system with secure fixed and mobile (GPRS/GSM/WAP)
connectivity. It employs mobile agents, web databases with Java database connec-
tivity for storage and processing of information.
MOMEDA [14] project was focused on the development of a compact personal
information terminal for hospital and home care environment that could be used by
patient and a demonstrator that allows the consulting physician to access electronic
patient record data from outside the hospital, using a handheld companion device
connected to GSM network. This project was sponsored by Nokia, and the Nokia
9110 communicator was used in the test-bed and demonstration.
3 Home-Based Healthcare Services
Compared to hospitals, home is the more comfortable and favorable to the patients or
occupants, and the expense of healthcare services can dramatically be reduced if this
service can be delivered to the home, without interrupting their daily activities. With
Internet, wireless LAN and personal area network technologies, pervasive healthcare
applications at home applications include patient monitoring, mobile/fixed telemedi-
cine, location or proximity services, emergency response and management, and well-
ness fitting/tracking, have been widely deployed and discussed. To break the bounda-
ries in time, space, and organization that healthcare service may face, mobile device
based healthcare application could be one of the candidate solutions thanks to widely
deployment of wireless network.
To bring health care to the home, motivation and availability of technologies to be
used can be seen unchanged, however, the scenarios at home space are different from
the cases in mobile healthcare mentioned above. Depending on the severity of their
diseases, occupants do not need to stay at hospitals, but they will lead a normal life
while their medical data are monitored and analyzed by healthcare professionals. This
situation leads the popularity of smart health at home or called smart home for health-
care services, such as elder care services [15, 16, 17]. Home-domain healthcare envi-
70

ronment gives residents as much autonomy and even responsibility for themselves
and their environment as possible. Pervasive sensors can be used to monitor vital
signs and health indicators. These sensors also include some position sensor to sense
the position of patient and monitor their activities. In other words, pervasive comput-
ing as well as computational technologies will let adults age in place. But few of them
bring the use of mobile phone to the discussion and this remains to future investiga-
tion. Home-based sensor and diagnostic technologies can be installed in the home
space to fit occupant’s need, and could help establish “disease signatures” that show
up physiologically and behaviorally before severe symptoms become readily appar-
ent.
4 Roles of Sensor Networks
Sensor networks have been established not only for sensing the data from the target
environment or objects but also been designed to provide the services for them to
meet some performance criteria or requirements. Especially, bio-signals have been
used to offer health monitoring [18]. Several personal area networks using bio-
sensors have been discussed to monitor some key or vital signals during the daily
activities [19, 20, 21, 22, 23].
Traditionally, personal medical monitors have been used for data acquisition.
With the developments of wireless and mobile technology, wireless sensor network
with intelligence will provide more feasibility to the users. In addition, PDAs and/or
mobile phones have been considered to be an important component as a gateway and
they are portable, so that the sensed data from the sensor networks either can be re-
layed/transmitted to the medical database through Internet or can be proc-
essed/filtered to enhance these medical data for specific further medical activities
around the users. In general, we observe that this type of architecture based on sen-
sors is tree-type and can been seen the first or last hop of entire network. That is, for
example, PDA or mobile phone is used as a central control node to its associated
sensors and to process the sensed signals. The connection between sensors to these
mobile devices could be designed using standardized protocol, for example, IEEE
802.15.1/bluetooth and IEEE 802.15.4/ZigBee.
Telemedicine and monitoring services provided by sensor networks also make
sense to be installed for home-based healthcare services. These services include not
only personal medical data recording but also occupants’ physiological and behav-
ioral monitoring [24, 25]. That is, home-based sensor network and diagnostic tech-
nologies could help establish disease signatures that show up physiologically and
behaviorally before more severe symptoms become readily apparent. However, sev-
eral challenging issues still remain using sensor network technologies. For example,
how to translate the sensor data securely to context-awareness. In addition, based on
the sensed data from the embedded sensors at home, how to estimate some key pa-
rameters confidently from occupants’ behavioral manner and physiological rhythms
at home to provide specific healthcare service is also one of the challenging issues.
Furthermore, requirements will depend on the needs and attitudes of occupants, even
71

in the same home space. How to design a sensor network with an intelligent interface
engine not only sense the data but also analyze the data as well remains to investigate.
5 Future Visionary Scenario: Smart Home plus Pervasive
Healthcare
From home point of view, several smart home activities have been working for years.
To make home be smart and services to be aware to the user/owner, there are several
home network middleware schemes, such as Univeral Plug and Play (UpnP) [26],
Java-based JINI [27], Open Services Gateway Initiative (OSGi), Home Audio/video
Initiatives (HAVi) to control home networks that are composed of computers and
various electronics appliances. In addition to electronic appliances as components of
smart home, other objects, such as a cup or medicine refilled bottles, etc, should be
also been viewed to provide data from healthcare’s point. In other worlds, the
user/owner shall feel confidently and comfortable use mobile devices for his/her daily
life. To achieve this scenario of smart home integrating with pervasive healthcare
services using mobile devices, several challenging issues should be tackled without
the limit to the following. First, generic home network architecture of smart home to
provide healthcare services is a must. That is, this home network architecture should
be built not only by suitable sensors or sensor networks, but also probably with mul-
tiple different service discovery protocols (SDP) to meet the
needs/requirements/services at home. Based on this, the physiological and behavioral
data of user can be recorded and monitored as input to healthcare services. Second,
interoperability is an issue too. Each existing service protocol and middleware
scheme cannot meet all the requirements of this future scenarios. Thus, the interop-
erability of different SDPs at home to provide healthcare service remains as one of
the challenges. Third, as the amount of appliances and objects increases at home, the
scalability will be an unavoidable issue and should be considered. Especially coupled
by the interoperability factor referred by different SDPs, network architecture and
service connection built by some surrogate nodes at home should be carefully
planned and design to meet the requirements of interoperability, scalability and ro-
bustness. Fourth, with mobile devices been used at home, security and user experi-
ence are worth to investigate. How to build a trust domain in a home to meet the
requirements not only from services used at home point of view, but also from
healthcare service point of view. In addition, how to make user be aware of the ser-
vices around the home and live confidently and comfortably using his/her mobile
devices is worth to investigate in the future.
6 Conclusion
With the need of electronic medical records and the deployment of pervasively-built
wireless network including the mobile devices, mobile healthcare systems and ser-
vices have brought more focuses and interests recently. There have been lots of ac-
72

tivities for mobile healthcare vendors to develop suitable products and services to
satisfy their customers, either inpatients or outpatients, or both. These technologies
will not only help physicians to work from any where, and collaborate with other
physicians and specialists on line, it will also save them administrative time, which
will translate into more value added time for healthcare provider and ultimately the
patients. On the other side, as senor networking and pervasive computing technolo-
gies are getting more mature, the support for home based healthcare service will not
be too far and brings the quality of life to the occupants, no matter they are of age or
not. Moreover, emerging net-centric standards for service-registry like Universal
Description, Discovery, and Integration and the standardized Web Services Descrip-
tion Language (WSDL) can be used to integrate the smart devices and services pro-
vided within a smart home with other community services. With the help of sensor
based components and networks, the dream and flexibility of the mobile healthcare
services getting closer to end users (for example, both patients and physicians) at any
where, at any time and using any mobile devices will come true soon. It is conclusive
that some of the current and successful telemedicine systems will be more geared
toward emerging wireless solutions in healthcare scenarios that are not feasible with
current generation of cellular telephonic and Internet services, so as to the user can
also take the benefits and services support by the home to experience a comfortably
daily life.
References
1. Best Practices in Healthcare Information Security for HIPPA Compliance, white paper of
CTG Healthcare Solutions, http://www.ctg.com/
2. Enable Remote Access to Personal Electronic Medical records, E. S. Hall, et al, Engineering
in Medicine and Biology Magazine, IEEE, vol. 22, no. 3, pp. 133-139, May-June, 2003.
3. Telemedicine Technology (Chapter 6), M. Ackerman, et al, Telemedicine Journal and e-
Health, vol. 8, No. 1, p. 71-78, 2002.
4. An introduction to Mobile Health Care, Claudia Tessier, white paper of MOHCA,
http://www.mohca.org.
5. Use of XML Technology in a Virtual Patient Record Infrastructure, A. Berler, et al, Informa-
tion Technology Applications in Biomedicine, 2003. 4
th
International IEEE EMBS Special
Topic Conference, pp. 118-121, April 2003.
6. Integration of distributed Healthcare Records: Publishing Legacy Data as XML Documents
compliant with CEN/TC251 ENV 13606, J. A. Maldonado, et al, Computer-Based Medical
Systems, 2003. pp. 213-218, Proceedings. 16
th
IEEE Symposium, June 2003.
7. Appling Telecommunication Technology to Healthcare Delivery, J. C. Lin, IEEE EMB
Magazine, 18, 4, July/August 1999, pp .28-31.
8. Wireless Telemedicine System: An Overview, C. S. Pattichis, et al, IEEE Antenna’s and
Propagation Magazine, vol. 44, No. 2, pp. 143-153, April 2002.
9. MobiHealth Project- http://www.mobihealth.org/
10. AMON Project - http://www.medictouch.net/amon/
11. Practical Evaluation of GPRS Use in a Telemedicine System in Cyprus, S. Voskarides, et
al, Proc. of the 4
th
Annual IEEE conf. On Information Technology Application in Biomedi-
cine, UK, 2003, p. 39-42
73

12. A Novel Emergency Telemedicine System Based on Wireless Communication Technology
– AMBULANCE, S. Pavlopoulos, et al, IEEE Transaction on Information Technology in
Biomeddicine, vol. 2, no. 4, p. 261-267, December, 1998.
13. DITIS Project - http://www.ditis.ucy.ac.cy/
14. MOMEDA Project - http://www.biomed.ntua.gr/momeda/index.html
15. The concept of the Home Health Monitoring, M. Ogawa and T. Togawa, Proceeding of the
5
th
International Workshop on Enterprise Networking and Computing in Healthcare Industry
(Healthcom), p. 71-73, 2003.
16. Using Pervasive Computing to Deliver Elder Care, Vince Stanford, Pervasive Computing,
IEEE, p. 10-13, vol. 1, Issue 1, January-March, 2002.
17. Aware Technologies for Aging in Place: Understanding User Needs and Attitudes, E. D.
Mynatt, et al, Pervasive Computing, IEEE, vol. 3, Issue 2, pp. 36-41, April-June, 2004.
18. Biosignals offer Potential for Direct Interfaces and Health Monitoring, Vince Stanford,
Pervasive Computing, IEEE, vol. 3, Issue 1, p. 99-103, January-March, 2004.
19. Stress Monitoring Using a Distributed Wireless Intelligent Sensor System, E. Javonov et al,
IEEE Engineering in Medicine and Biology Magazine, p. 49-55, May/June, 2003.
20. Synchronized Physiological Monitoring Using a Distributed Wireless Intelligent Sensor
System, E. Jovanov, et al, p. 1368-1371, Proceedings of the 25
th
Annual International Con-
ference of the EMBS, Cancun, Mexico, September17-21, 2003.
21. Continuous Monitoring of Vital Constants for Mobile Users: the MobilHealth Approach, D.
Konstantas and R. Herzog, p. 3728-3731, Proceedings of the 25
th
Annual International Con-
ference of the EMBS, Cancun, Mexico, September17-21, 2003.
22. Implementation Solutions and Issues in Building a Personal Sensor Network for Health
Care Monitoring, Srdjan Krco, p. 350-353, Proc. of the 4
th
Annual IEEE Conf. on Informa-
tion Technology Applications in Biomedicine, UK, 2003.
23. Personal Wireless Sensor Network for Mobile Health Care Monitoring, Srdjan Krco and
Vlado Delic, p. 471-474, TELSIKS, October 1-3, 2003.
24. Long Term Remote behavioral Monitoring of Elderly by Using Sensors Installed in Ordi-
nary Houses, M. Ogawa, et al, 2
nd
Annual International IEEE-EMBS Special Topic Confer-
ence on Microtechnologies in Medicine & Biology, p. 322-325, May 2-4, 2002.
25. Enabling Location-Aware Pervasive Computing Applications for The Elderly, S. Helal, et
al, pp. 531-536, Proceedings of the First IEEE International Conference on Pervasive Com-
puting and Communications, 2003 (PerCom 2003).
26. UPnP, http://www.upnp.org.
27.Sun Microsystems: Jini technology architecture overview.
http://www.sun.com/jini/whitepapers/architecture.pdf
74
