
Understanding Trust in Medical Technologies
Wiktoria Wilkowska and Martina Ziefle
Human-Computer Interaction Center, RWTH Aachen University, Campus Boulevard 57, Aachen, Germany
Keywords: Trust, Medical Technology, Ambient Assisted Living, User Diversity, Age, Gender.
Abstract: This paper aims to extend knowledge with respect to trust in health-related technology and deals with an
exploration of this topic and the validation of the findings using multi-method research. The empirical
approach aimed at the evaluation of the opinions and attitudes towards the importance of trust conditions
(reliability, trustworthiness, operability and easing) and trust “mediators” (physician as a role model,
scientific evidence, exchange with peers and hands-on experience), and assessed the relevance of different
system features among different users. User factors such as age, gender and the perceived health condition
were taken under consideration as representative indicators of the diversity among the (potential) users.
Results showed a significant influence of age and gender on the examined trust indicators and underline the
importance of considering the users’ diversity in the research of trusted – and thus accepted – medical
systems in home environments.
1 INTRODUCTION
Electronic health technology (eHealth) in the context
of Ambient Assisted Living (AAL) represents one of
the biggest shifts in healthcare today. Innovative
advancements in digital technology allow healthcare
organizations to change the way healthcare is
delivered, and users to reframe their view on how
they can maintain their health and well-being more
independently. Currently, many institutions and
stakeholders are making efforts to optimize and/or
improve the infrastructure in this regard to ensure
the widespread use of the common health-supporting
technologies at home.
Therefore, health-related technological devices
which monitor the relevant vital parameters and
offer support to manage the well-being of people
outside of traditional medical institutions have a
great potential to rapidly become common tools to
support health-care in people’s homes. However, the
success of the adoption of such ambient medical
technologies largely depends on the extent to which
users trust, and can rely on, the equipment. In
addition, it is crucial to understand how people will
trust in ambient medical technology systems while
achieving and maintaining their privacy (Little et al.,
2007). Especially in the field of medical technology,
it is therefore important to adapt the devices to the
special needs and – if possible – to wishes of the
(potential) users which, naturally, requires a careful
examination of the differences between the users.
1.1 The Phenomenon of Trust
Research with respect to the integration of
information systems indicates that trust plays an
important role in helping users to overcome
perceptions of risk and uncertainty in the use and
acceptance of new technologies (Li et al., 2008;
Pavlou and Grefen, 2004). Despite the broad
consensus that trust in technology is one of the most
important factors in the technology saturated society
(Lewis and Weigert, 1985; Falcone and
Castelfranchi, 2001), the phenomenon of trust is
anything but clear and consistent in the relevant
literature. It does not only concern the different
contexts of the computerized society (e.g.,
information and communication technologies, e-
commerce, intelligent physical environments, virtual
reality, etc.) but also people’s trust in a secure digital
infrastructure, sources of information, data, personal
assistants, and processes and software.
Trust is not easily defined. The extensive amount
of research regarding trust leads to a certain
fuzziness of the definition of trust, resulting in some
difficulties to clearly understand the term. The main
reason for this is its multidisciplinary and multi-
contextual nature. For instance, Boon and Holmes
62
Wilkowska, W. and Ziefle, M.
Understanding Trust in Medical Technologies.
DOI: 10.5220/0006734500620073
In Proceedings of the 4th International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AWE 2018), pages 62-73
ISBN: 978-989-758-299-8
Copyright
c
2019 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

(1991) defined it as “a state involving confident
positive expectations about another’s motives with
respect to oneself in situations entailing risk” (p.
194). Within the field of e-commerce, trust is related
to three perceptual factors that have an impact on
online trust: perception of credibility, ease of use
and risk (Corritore, 2003). Then again, Wang and
Emurian (2005) identify four elements of online
trust regarding interface design features, which
relate to graphic, structure, content and social-cue
design. The evidence that the design of an interface
can significantly impact the perceived
trustworthiness of a system also applies to mobile
technologies (Siau and Shen, 2003). Thus,
researchers often conceptualize trust according to
the features of a particular context (Sillence et al.,
2006).
Studies involved in the development of a
framework for the construct of trust in the context of
medical technology proved that the trust in medical
technology empirically differs from the general trust
in technology (Montague et al., 2009). The
phenomenon of trust seems to be more indispensable
when health-relevant aspects are technology-
mediated (Wilkowska, 2015). The concept is multi-
faceted and includes different factors which might
be important for understanding how the acceptance
and long-term adoption of health-enhancing
technologies can be ensured; these factors concern,
among others, personalization, motivation, expertise,
familiarity, predictability, sensitivity, and the source
of the information.
Because of the rising number of older people,
and thus presumably those with rather frail health,
patient’s trust in medical technology may be an
important factor of functionally working systems;
especially since health care work systems move to a
higher reliance on and use of medical technologies
(Montague, 2010). As a fundamental attribute in the
adoption of health-supporting technologies, trust
refers to a variety of relationships: interpersonal trust
(e.g., in the patient-physician communication), trust
in the environment and in the infrastructure (Falcone
and Castelfranchi, 2001), social trust (e.g., in a
healthcare institution) and the trust in automation
(Muir, 1994).
In the context of emerging AAL-environments,
where technology is meant to assist people in their
everyday life and support them in terms of their
health (e.g., monitoring devices, measurement of
vital parameters, sensors recording fall detection,
etc.), trust is a particularly important phenomenon,
which has been barely researched yet. Individuals
are confronted with situations, in which they have to
trust the medical devices that are incorporated in an
ambient technology system and which, depending on
how much their health impairments have them rely
on this technology, become part of their life. In this
context, trust is more likely to be a dynamic process,
which might change depending on the users’
characteristics (e.g., age, gender), current health
conditions or the changing circumstances of their
lives. Considering the differences between the
(potential) users is, therefore, of utmost importance.
1.2 The Differences in the Users
For a long time, the scientific studies of information
technology have perceived that individual
differences exert a major force in determining its
success (Zmud, 1979). Accordingly, a lot of
scientific evidence shows that differences in socio-
demographic characteristics, computer experience,
cognitive abilities, and personality are significant
factors in explaining both technology acceptance
and user behaviour (e.g., Gefen and Straub, 1997;
Rogers and Fisk, 2000; Ong and Lai, 2006;
Wilkowska and Ziefle, 2009).
Especially age, as a factor of user diversity, plays
an enormous role in the explanation of the
variability in system acceptance and performance.
Not only the users’ belonging to a particular
technology generation (e.g., Sackmann and Winkler,
2013) and the connected know-how, perceived self-
efficacy and attitudes towards technology, but also
the users’ mental and physical state can decisively
influence their trust in, and use of, a certain
technology system. Therefore, the development of
age-sensitive and age-appropriate interfaces is
highly challenging because aging itself is a very
complex and differential process. The same applies
to the users’ gender and the resulting differences
with respect to technology perceptions and
behaviours (e.g., Schumacher and Morahan-Martin,
2001; Broos, 2005; Gaul et al., 2010). Changes in
health conditions or stressful life events can also
have a strong impact on the perception of, and
intention to use, assistive technology (e.g.,
Wilkowska, 2015).
Recent research dealing with the acceptance of
technology in the context of health-supporting
technologies in the domestic settings, increasingly
considers different users and their different needs in
the development and design process (e.g., Demiris et
al., 2004; Klack et al., 2011; Wilkowska and Ziefle,
2011; Ziefle et al., 2016a). Since this technology is
primarily intended for the elderly, disabled and/or
people with a chronic disease, it must be taken into
Understanding Trust in Medical Technologies
63

account that their trust in such an assistive
technology may largely differ from the trust of
younger, healthy and carefree users.
1.3 Questions Addressed
Based on the described considerations, the present
research examined the concept of trust contextually
regarding the increasingly used medical technology
in home environments. The approach was performed
in two empirical steps: First, using a qualitative
research method to explore the topic of trust in the
upcoming context from scratch. For this, participants
should discuss different trust aspects of the
integration of the technology in the living
environment (socio-technical system) and the trust
in a system or institution which manages the health
data (social trust), over the interpersonal trust (e.g.,
in the communication with the physician in charge)
through to the perceived reliability and demands
regarding technical device or system (technological
trust). After that, the qualitative results were
validated using quantitative method to ascertain the
generalisability of the findings. Unlike in the
previous research, special focus was thereby directed
to the user diversity which was assumed to
considerably influence the trust itself.
2 METHOD
The content described in this paper are part of a
wider range of studies conducted to explore the
users’ perceptions and requirements regarding
medical assistive technologies in home
environments (see Wilkowska, 2015).
The concept of the described empirical studies
uses a user-centred design approach, the main goal
of which is to reveal how technical systems must be
designed for, and adapted to, the individual concepts
and mental models of the (potential) users.
In this study on the trust in, and the perception of
privacy towards, electronic health technology,
opinions regarding the characteristics that are
perceived as necessary to the use of (and trust in)
medical devices, as well as conditions for the use of
such devices, were collected. For this purpose, a
multi-method empirical approach was pursued
which is described in more detail hereafter.
2.1 Multi-method Approach
Considering the user-centred design of the
conducted qualitative and quantitative studies,
special attention was paid to user diversity (e.g.,
user’s age, gender, physical/health condition, etc.)
and the dynamics of personal biographies (e.g., the
onset of an illness). Therefore, some of these criteria
were decisive for the composition of the focus
groups which represented the first step of the
empirical procedure.
2.1.1 Focus Groups
Focus groups were arranged to gather qualitative
information about the designated topic. This method
was chosen because group interactions may
accentuate members’ similarities and differences in
a particular context and provide rich information
about the range of perspectives, opinions, cognitive
beliefs and experiences (Lambert and Loiselle,
2008). The idea was to initially explore the topic of
trust and acceptance in the context of the use of
different medical technology devices in a domestic
setting. Therefore, a relevant part – next to the topic
of privacy in the context of eHealth technology –
were the discussions about the aspects which are
relevant, or even indispensable, for a trustable and
accepted (daily) use.
In three focus groups sessions (N=15), women
(60%) and men of different ages (age range: 23-64
years) exchanged their views on the following
questions: “In your opinion, which characteristics of
a health-related technology which is used in a home
environment are essential?” and “Which conditions
would have to be fulfilled for you to use (and trust) a
medical-support device which has to be used at
home?”. Considering the preceding discussions
about the thematically related topics of ’trust’ and
’privacy’ when dealing with health-supporting
equipment, and after the introduction of the related
topics, like chronic diseases (e.g., cardio-vascular
conditions, diabetes, etc.), the process of ageing and
the need for care, participants presented their
requirements, reservations and conditions of usage.
The objective was to find out which basic
characteristics of the devices are expected and which
conditions are required by the (potential) users to trust
and rely on the interaction with such devices, in order
to increase their acceptance and the adoption in the
long run. The resulting expected characteristics of
health-supporting devices which are used in home
environments are summarized in Table 1. In Table 2,
the conditions for trusted usage are presented.
Methodologically, focus groups allow a deeper
insight into the nature of such sensitive and,
somehow, difficult-to-grasp topics. However, the
restrictions of the method refer to a comparably
ICT4AWE 2018 - 4th International Conference on Information and Communication Technologies for Ageing Well and e-Health
64
small sample size and personally coloured results
which are unrepresentative. To scientifically
ascertain the representativeness of the findings, the
outcomes of the focus groups were taken as an
empirical base for the subsequent construction of
survey items to allow further quantitative data
collection with a larger sample.
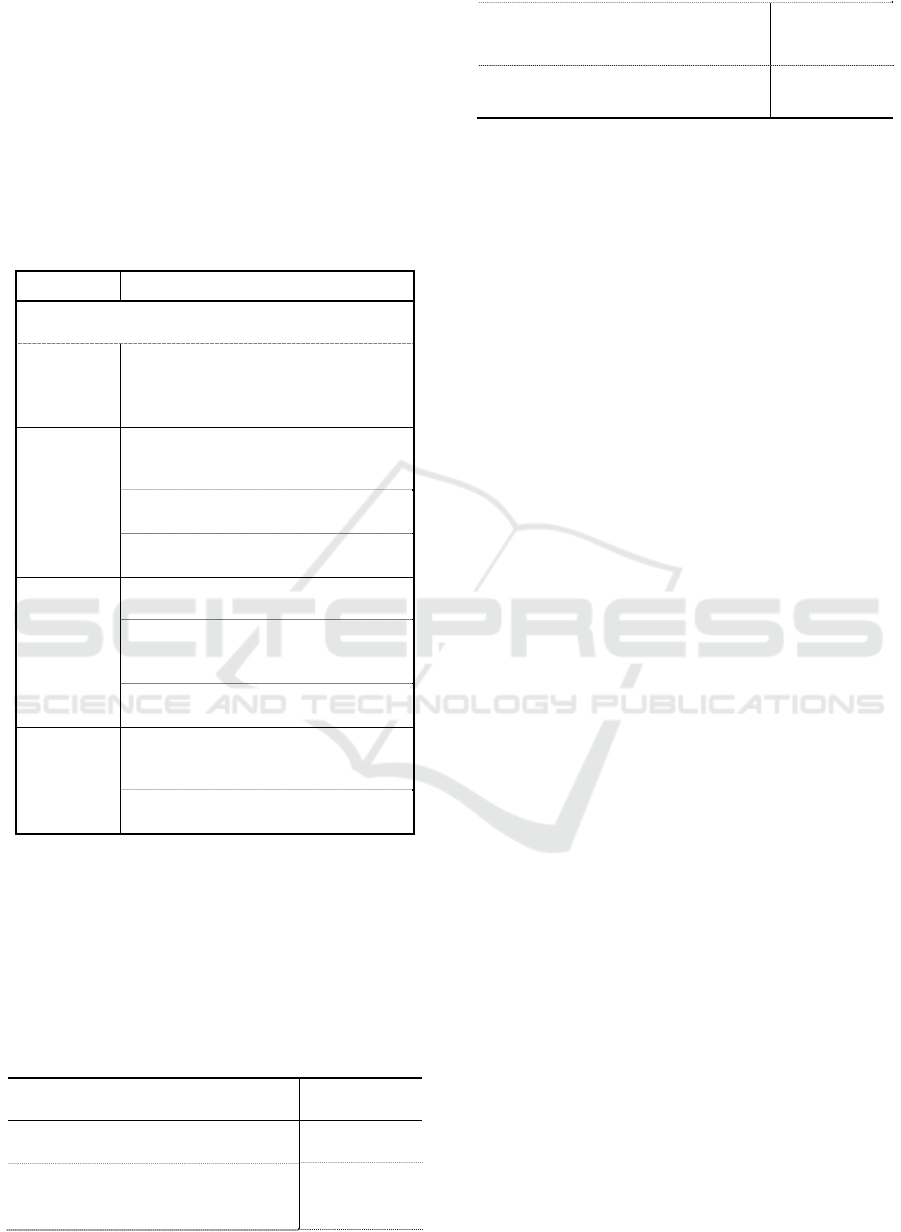
Table 1: Expectations for eHealth devices for domestic
use.
Item description Scale
1. Unconditional reliability
Six-point
Likert scale
ranging
from 1
(‘not at all
important’)
to 6 (‘very
important’)
2. Ease of use
3. Low price
4. Seal of approval / test label
5. Attractive / fashionable design
6. Unobtrusiveness
7. Officially recognized manufacturer
8. Recommendation of the physician
9. Financial support of the health
insurance for procurement,
maintenance, etc.
10. State of the art
11. Strict access control to the health
data (e.g., by fingerprint)
2.1.2 Quantitative Survey
In the next step of the empirical approach a
questionnaire was conducted to quantitatively
validate the most interesting findings.
The questionnaire was divided in three parts: In
the first part, the participants answered questions
about their socio-demographic profiles (e.g., age,
gender, professional background, health condition
etc.). They also reported their experience with
health-supporting devices in their daily lives. The
second part focussed on privacy in the context of
health-supporting technology in domestic
environments, but will not be analysed or discussed
further in the present paper. The last part of the
survey collected data on the trust in eHealth
technology. To do so, respondents had to work on
the following questions: 1) features and
characteristics expected/required for the devices, 2)
trust-conditions that must be met for accepted usage,
and 3) complementary statements, retrieved from the
focus group discussions, about what else makes the
medical technology at home trustworthy.
The participants were recruited through
advertisements in local newspapers, social networks
on the Internet and collaboration with targeted
societal groups (e.g., retirement home). Some of the
respondents were also reached through the authors’
personal contacts. There was an online version and a
paper-based version of the questionnaire (from the
latter especially the older participants benefited). On
average, it took 15-20 minutes to complete the
questionnaire and the data collection lasted for about
four weeks.
2.2 Research Approach
In accordance with the concept of user-centred
design (e.g., Abras et al., 2014; Mao et al., 2005),
the research variables focus on different
characteristics and health biographies of the users on
the one side, and on their expectations and
requirements for trusted health-supporting
equipment at home, on the other.
2.2.1 Independent Variables
Technology users do not only hugely differ in their
socio-demographic characteristics, but also in their
sensory and cognitive skills, physical and motoric
capabilities, and their different requirements (e.g.,
those linked to aging) which complicate an easy-
going interaction with modern technical solutions
(Wilkowska, 2015).
To deepen the understanding of the diversity
among the (potential) eHealth users, as well as of
their different needs and requirements, it is crucial to
consider different points of view regarding the trust
in such a technology. In the present statistical
analyses, three independent variables, which refer to
the participants’ diversity, will be considered:
Age [young (≤44 years; 50%) vs. middle-aged
and older (45 years and older; 50%)];
Gender [women (46%) vs. men (54%)];
Perception of the own health condition [good
(44%) vs. moderate (46%) vs. poor (10%)].
2.2.2 Dependent Variables
The dependent variables refer to the perceived trust
in the eHealth technologies which are used in
people’s home environments for health monitoring,
prevention and rehabilitation.
First, the required features and characteristics
for eHealth devices (see Table 1) are considered as
dependent variables. After that, the conditions of
trust regarding health-supporting technology in
domestic settings are examined. The items were
evaluated using a six-point Likert scale ranging from
1 (‘strongly disagree’) to 6 (‘strongly agree’). For a
better overview, thematically related aspects are
merged into categories (see Table 2). Next to the
device’s reliability, three other main categories of
Understanding Trust in Medical Technologies
65
trust conditions were generated (the internal
consistency of the particular categories is indicated
between brackets):
Trustworthiness (Cronbach’s alpha α=.71;
min=3, max=18);
Operability (Cronbach’s alpha α=.73; min=3,
max=18;
Easing of the burden of the disease (Cronbach’s
alpha α=.83; min=2, max=12).
Table 2: Formed trust categories of eHealth technology.
Category Item description
“I would trust the medical device
if…
Reliability
…it would immediately provide
feedback about incorrect information
and asks me to repeat the
measurement.”
Trust-
worthiness
…I would know that it comes from
an approved and trustworthy
manufacturer.”
…its reliability would be confirmed
by a recognized testing institution.”
…I would rarely have to see the
doctor thanks to the device.”
Operability
…I would intuitively understand how
to handle the device.”
…I would be able to count on
customer service in case I experience
difficulties.”
…it would allow me to take it
anywhere to make measurements.”
Easing
…it would be integrated in my daily
life so that I feel relieved from my
illness.”
…it would give me the feeling of
independence despite my illness.”
Moreover, four additional statements on what else
makes the use of a health-supporting technology at
home trustworthy were added as dependent
variables. Likewise, participants expressed their
level of agreement (6=‘strongly agree’) or
disapproval (1=‘strongly disagree’) regarding the
aspects presented in Table 3.
Table 3: Additional statements regarding trust in eHealth.
Item description
Short
description
“If my doctor relies on medical
technology, I trust it.”
doctor as a
role model
“I consider medical devices whose
quality and functionality are confirmed
by scientific studies to be trustworthy.”
scientific
evidence
“I consider medical equipment, which
functionality I can try out for a while
without paying, to be trustworthy.”
hands-on
experience
“My trust in medical devices would be
greater if I could exchange with peers.”
exchange
with peers
2.3 Participants
The sample intended to cover different population
groups including young, middle-aged and older
people with different skills, professional
backgrounds and levels of experience with
technology.
This study collected and analysed the data of
N=104 participants (ages ranged between 21-98
years). More than 40% of the respondents reported
to suffer from chronic health conditions (e.g.,
cardiovascular diseases, diabetes mellitus, asthma).
Overall, more than half of them reported experience
with health-supporting devices in everyday life: the
most participants used blood pressure meters (32%),
followed by those who used blood sugar meters
(10%) and 9% used heart rate monitors; a few (6%)
also reported to use hearing aids and insulin pumps.
Different professions (including teachers,
engineers, economists, psychologists and
mechanics) and different educational levels were
represented in the sample; there was a quite high
average level of education though. The participation
in the study was voluntary and respondents were not
compensated for participating.
3 RESULTS
For the statistical examination of the independent
variables’ significant influence on trust, multiple
analyses of variance (MANOVA) were executed and
the significance of omnibus F-Tests was taken from
Pillai values. For descriptive analyses, the means
(M) and standard deviations (SD) are reported, and
the parameter partial eta squared (
η
2
) was calculated
for the effect sizes according to Cohen (1988). For
the continuous trust variables, Pearson’s product-
moment correlations (r) were calculated. The level
of statistical significance (p) was set at the
conventional 5%.
3.1 Expected Features for eHealth
In the first step, the influence of independent
variables on the expected trust characteristics is
statistically examined. A multivariate analysis of
variance revealed a significant omnibus effect of age
ICT4AWE 2018 - 4th International Conference on Information and Communication Technologies for Ageing Well and e-Health
66
[F(11,76)=2.1, p=0.033;
η
2
=.23] and gender
[F(11,76)=2.6, p=0.007;
η
2
=.27].
The effects of age on the between-subject level
resulted for the following characteristics: ease of use
[F(1,98)=7.6, p=0.007;
η
2
=.08], low price
[F(1,98)=5.9, p=0.017;
η
2
=.06], officially recognized
manufacturer [F(1,98)=7.3, p=0.008;
η
2
=.08] and the
state of the art [F(1,98)=6.9, p=0.01;
η
2
=.07]. The
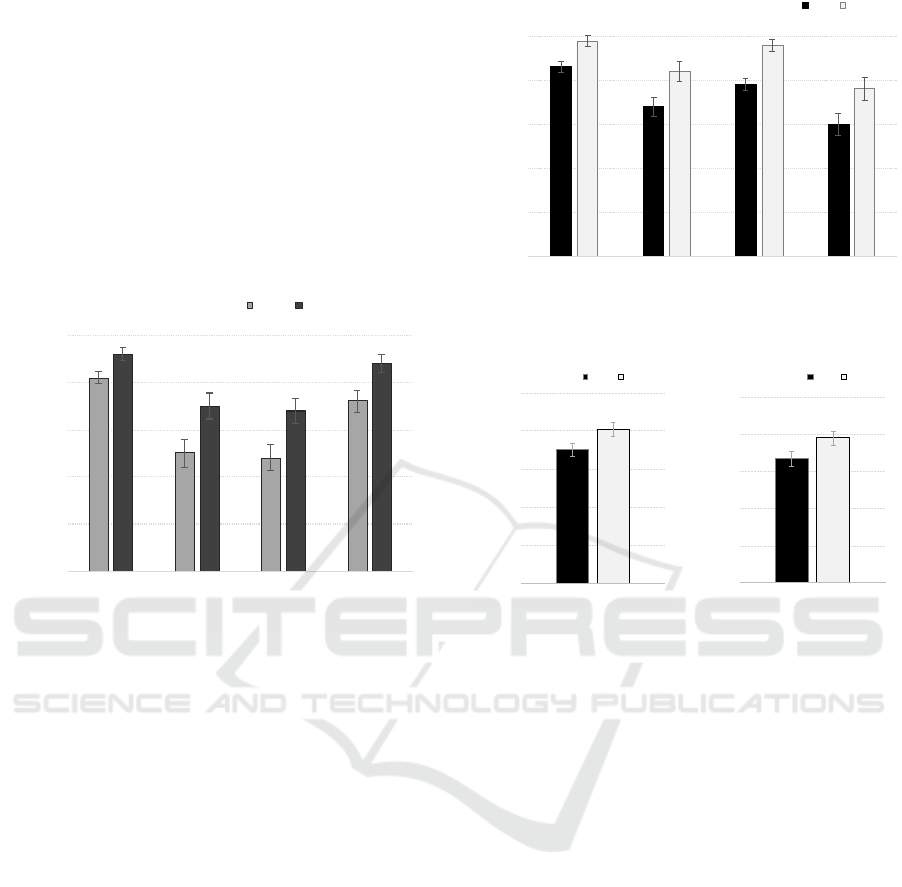
resulting means are depicted in Figure 1. It is evident
that the middle-aged and older participants expect
significantly higher standards for medical equipment
in domestic settings than the young participants.
1
2
3
4
5
6
Ease of use Low price Officially
recognized
manufac
t
ure
r
State of the
art
Attributed Importance (max=6)
Young Middle-aged and old
Figure 1: Effect of age on expectations regarding eHealth
technology in home environments.
Considering the impact of gender the on expectations,
the particular effects on the between-subject level
result for unconditional reliability [F(1,98)=4.6,
p=0.035;
η
2
=.05], seal of approval [F(1,98)=7.7,
p=0.007;
η
2
=.08], ease of use [F(1,98)=20.1,
p≤0.001;
η
2
=.19] and recommendation of physician
[F(1,98)=5.6, p=0.021;
η
2
=.06]. Descriptive data
(Figure 2) demonstrate that women have higher
expectations regarding health-supporting devices
than men. According to the effect sizes, the impact
of gender is especially meaningful for the ease of
use of the medical technology.
3.2 Trust Conditions for eHealth
In the next step, the independent variables’ influence
on the usage conditions of health-supporting
technologies in domestic settings were examined.
Analyses of variance revealed a significant main
effect of gender on the condition of flawless
operability of the digital medical technology in an
AAL environment [F(1,101)=4.2, p=0.043;
η
2
=.04].
The influence of gender on the trust condition of
operability is evident in Figure 3 (left).
1
2
3
4
5
6
Unconditional
reliability
Seal of approval Ease of use Recommendation
of physician
Attributed Importance (max=6)
Men Wo
m
e
n
Figure 2: Effect of gender on expectations regarding
eHealth technology in home environments.
3
6
9
12
15
18
Degree of Agreement (max=18)
Operability
Me
n
Wom e
n
3
6
9
12
15
18
Degree of Agreement (max=18)
Thrustworthiness
Me
n
Wom
e
n
Figure 3: Main effect of gender on the conditions of
operability (left) and trustworthiness (right) when using
eHealth technology in home environments.
A similar pattern is noticeable regarding the
conditions that form the trustworthiness
[F(1,100)=4.4, p=0.039; partial
η
2
=.05]. The mean
values are depicted on the right in Figure 3. Even
when, according to the rather small effect sizes, the
impact of gender is minor in both cases, the results
indicate that women demand more stringent
conditions for medical equipment than men.
In addition, the univariate ANOVA revealed
moderate interacting effects of age and gender
[F(1,100)=8.7, p=0.004; partial
η
2
=.09], as well as
of gender and perceived health conditions
[F(2,100)=4.4, p=0.014; partial
η
2
=.09], on the
trustworthiness in health-supporting technology.
Especially in the younger age group, men (M=11.1,
SD=0.8) and women (M=15.1, SD=0.8) differ
significantly, whereby women demand higher
standards of trustworthiness in this context. As
opposed to this, the differences in the group of
middle-aged and older participants are not so evident
between women (M=14.3, SD=0.8) and men (M=15,
SD=0.7). The interaction is presented on the left in
Figure 4. Moreover, visible at the right side of
Understanding Trust in Medical Technologies
67
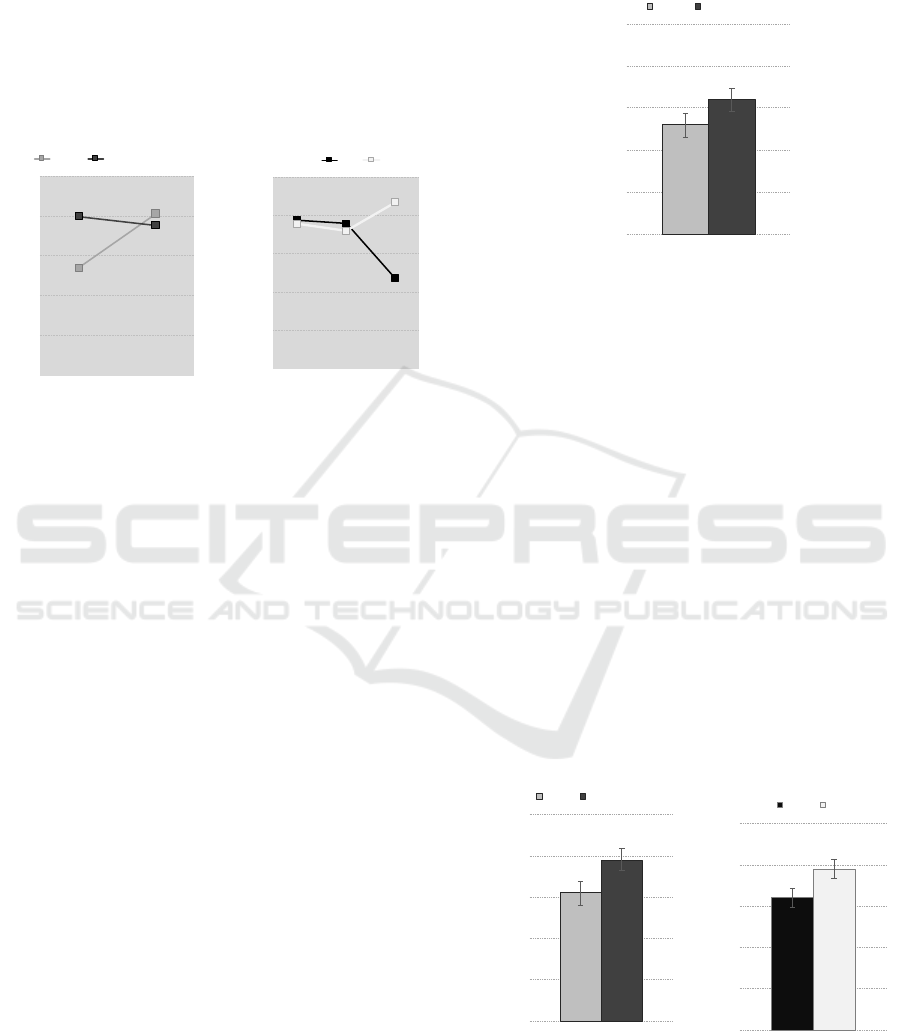
Figure 4, the additional influence of health condition
especially splits the opinions of those who report
bad health: Whereas women require very high
standards of trustworthiness (M=16, SD=1.5), men
with poor health do not pay as much attention to this
condition (M=10.1, SD=1.3). On the contrary, in the
groups of good and moderate health both genders do
not significantly differ in their opinions, both
reaching high means for the condition of
trustworthiness.
3
6
9
12
15
18
Men Women
Degree of Agreement (max=18)
Young Middle-aged and old
3
6
9
12
15
18
Good Moderate Poor
Degree of Agreement (max=18)
Health Condition
Men Wo me n
Figure 4: Interaction effects on the conditions of
trustworthiness: age and gender (left), gender and health
condition (right).
Furthermore, the statistical analyses of the trust
conditions of reliability and of the easing of the
burden of the disease, yielded no significant
influences of age, gender or health condition.
According to this, independent from the user
diversity, all participants wished for highly reliable
medical equipment which serves the purpose of
exoneration.
3.3 Additional Aspects of Trust for
eHealth
To complete the analyses related to trust in the
context of health-supporting technologies at home,
additional aspects which resulted from the
aforementioned group discussions (see Table 3)
were taken under consideration. The technique of
three-way analysis of variance was chosen for the
statistical evaluation.
Considering the aspect ‘doctor as a role model’
as relevant for the trust in medical devices, an
ANOVA with the factors age, gender and health
condition revealed a significant effect of the
participants’ age [F(1,102)=4.1, p=0.046;
η
2
=.04].
Figure 5 shows the differences between the average
values reached for both age groups. Even if the
differences in the perceptions are small, the outcome
shows that the middle-aged and older (M=3.6,
SD=1.5) confide in the opinion of the doctor, who
relies on the technology, more than young people
(M=4.2, SD=1.5).
1
2
3
4
5
6
Degree of Agreement (max=6)
Young M
i
ddle-aged and ol
d
Figure 5: Main effect of age on the trust aspect ‘doctor as
a role model’ for using eHealth technology at home.
In addition, for the aspect of ‘scientific evidence’ the
analysis of variance showed a moderate and strong
influence of the user factors: (1) main effect of age
[F(1,101)=6.1, p=0.015;
η
2
=.06]; (2) main effect of
gender [F(1,101)=4.5, p=0.036;
η
2
=.05]; and (3) an
interacting effect of gender and health condition
[F(1,101)=6.1, p=0.003;
η
2
=.12]. The descriptive
data for both main effects are depicted in Figure 6.
The moderate effect of age (on the left side of the
graph) shows that middle-aged and older people
(M=4.9, SD=1.2) perceive medical devices whose
quality and functionality is confirmed by scientific
studies as more trustworthy than the younger
participants (M=4.1, SD=1.4). Regarding the
influence of gender (on the right in Figure 6),
women’s average values (M=4.9, SD=1.2) exceed
those of men (M=4.1, SD=1.5), meaning that
women’s trust in medical equipment at home is
slightly more shaped by scientific studies.
Figure 6: Main effect of age (left) and gender (right) on
the trust aspect ‘scientific evidence’ for using eHealth
technology at home.
1
2
3
4
5
6
Degree of Agreement (max=6)
Young Middle-aged and old
1
2
3
4
5
6
Degree of Agreement (max=6)
Men Wo me n
ICT4AWE 2018 - 4th International Conference on Information and Communication Technologies for Ageing Well and e-Health
68
Next to the influence of age and gender, an
interacting effect of gender and the perceived health
condition resulted for the aspect of ‘scientific
evidence’; Figure 7 depicts the means of the
particular groups. Interestingly, for both genders the
biggest differences in this regard result for those,
who report poor health conditions, whereby women
with poor health (M=5.7, SD=0.5) attach
significantly higher importance to scientific
evidence than men (M=3, SD=2) with the same
health status.
1
2
3
4
5
6
Good Moderate Poor
Degree of Agreement (max=6)
Health Condition
Men Wom en
Figure 7: Interacting effect of gender and health condition
on the trust aspect ‘scientific evidence’ for using eHealth
technology at home.
Finally, a significant interaction effect of gender and
health condition results for the trust aspect of
‘exchange with peers’ [F(2,102)=4.3, p=0.016;
η
2
=.09]. The pattern is similar to the previous
analysis: Compared to people with good and
moderate health conditions in both genders, the
opinions change for men and women with poor
health conditions. Thereby, women (M=5, SD=0.8)
consider it to be more important to exchange their
opinions with peers than men (M=2.9, SD=1.6). The
mean differences are showed in Figure 8.
1
2
3
4
5
6
Good Moderate Poor
Degree of Agreement (max=6)
Health Condition
Men Wo me n
Figure 8: Interacting effect of gender and health condition
on the trust aspect ‘exchange with peers’ for using eHealth
technology at home.
For the aspect of ‘hands-on experience’ the results
are neither age-, gender-, nor health status-specific.
3.4 Special Case of Trust – the
Reliability
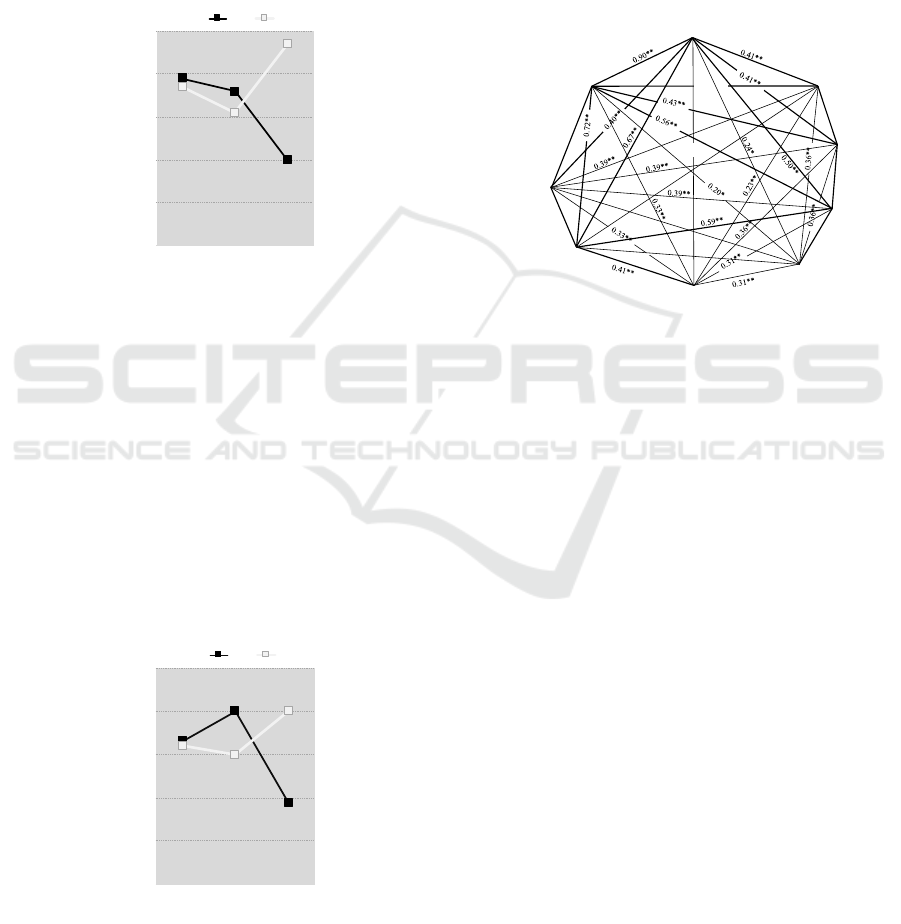
In the final step of the statistical analyses, the
interrelations between the researched trust variables
and their association with the perceived usefulness –
as a correlate of acceptance – of health-supporting
technologies in home environments are presented.
0.71**
Trustworthiness
Reliability
Scientific
Evi dence
Perceived Usefulness
Operability
H ands-on
exper i ence
Exchange
with peers
0.31*
0.54**
0.58**
Easing of the
Bur den of
the Disease
0.41**
0.57**
0.51**
0.34**
Doctor as a
Role M odel
Figure 9: Interrelations of the research variables with the
perceived usefulness.
As the previous analyses showed, the condition of
reliability was not influenced significantly by the
independent variables (i.e., age, gender and health
condition). However, the results of the correlation
analysis showed strong and moderate associations
with the other trust factors mostly ranging from
r=.40 (e.g., for the easing of the burden of the
disease), to r=.67 (for operability), to r=.90 (for
trustworthiness).
In the correlation analysis we additionally
included the variable ‘perceived usefulness’ of
health-related technologies to see how this
acceptance indicator is connected to the trust
variables elaborated in the presented studies. The
results are astonishing, showing rather weak
coefficients oscillating around r=.3 (e.g., with
trustworthiness, reliability, scientific evidence).
These findings suggest that trust in medical
technology does not mean that people accept it, but
– in accordance with relevant literature in this
context – additional components are necessary for a
high user acceptance.
Understanding Trust in Medical Technologies
69

4 DISCUSSION
In the present research, we focused on understanding
the trust in and trustworthiness of medical
technology which is increasingly used in home
environments. However, this topic is part of a
broader subject matter, regarding the acceptance of
medical technology. Facing the demographic change
and the increasing prevalence of medical technology
integrated into people’s lives and private spheres it
is of utmost importance that users really do accept
these technologies. However, acceptance is a truly
complex issue, which – especially in this sensitive
context – might not be easily described by the
traditional factors of technology acceptance (Davis
et al., 1989; Venkatesh, 2000). Plenty of usage
motives as well as usage barriers in the context of
medical technology are rather prevailing. In
addition, the motives and barriers heavily depend on
the situational context (e.g., when the medical
technology is life-saving with no usage alternatives),
the health status of the users (i.e., how severe is the
disease for which the medical technology is used),
and the personality of the user, including risk taking
behaviour, coping strategies, technical self-
confidence, media competence, etc. Moreover, as
outlined before, it has been shown that demographic
variables such as age, gender and education also
considerably impact the extent to which people are
willing to adopt and use medical technology.
Recent research uncovered the trust in, and
trustworthiness of, medical devices as major facets
of the acceptance of technology in the area of
medical technology. On the one hand, this is obvious
as the medical technology relates to sensitive and
fragile health constitutions which rely on a high trust
of users (Montague et al., 2009; Ziefle et al., 2011).
On the other hand, especially for older and
experienced people, one could assume that seniors
might be less sensitive in terms of acceptance of
technology, since they typically have no choice but
to use it. Still, the nature of the perception of the
trust in the area of medical technology and the
question on which requirements and usage
conditions might contribute to the perceived trust
and trustworthiness, is underdeveloped so far.
In the presented empirical studies, users of
different ages, of both genders and with different
health conditions shared their opinions and attitudes
towards the importance of trust “markers”
(reliability, trustworthiness, operability and easing)
and trust “mediators” (doctor as a role model,
scientific evidence, exchange with peers and hands-
on experience) and assessed the relevance of
different system features. Overall, the studies
disclosed findings, which turned out to be
insensitive to user diversity as well as findings in
which user profiles played a significant role.
Regarding the differences between the genders,
women attached a higher value to the ease of using
medical technology in contrast to men. Moreover,
women’s trust in medical technology at home relies
much more on scientific evidence, thus women
shape their trust in line with the validation by
science. When it comes to the impact of age, it was
found that middle-aged and older participants
significantly expect higher standards for medical
equipment than younger users. In addition, middle-
aged and older people confide in the opinion of the
doctor, who relies on the technology, to a higher
extent than younger people. An interesting finding
referred to the fact that especially women with a
poor health status report to rely on the exchange
with peers, while in the opinion of men the peer-
exchange is not that important for trustworthiness.
The findings for the trust conditions of reliability
and the easing of the burden of the disease yielded
no significant influences of age, gender or health
status. Apparently, there are deeply engrained
attitudes that are not formed by the diversity of
biographies and the change of values over the life-
span.
On a higher level, the presented outcomes
corroborate that user diversity, especially ageing and
frailness, should be a benchmark for the
development of medical technology. Technical
design, especially in the field of medical technology
field, should be aligned with the needs of the
respective end users. This does not only include an
understanding of the functional requirements of
medical technologies, but also the reframing of
traditional acceptance and usability benchmarks
(mostly concentrating on ease of use and
usefulness). In line with this, the perspective should
be broadened by including intimacy and trust
cognitions as a dictum for the design of a socially
responsible medical technology.
Of course, the empirical approach also has some
limitations which should be considered. The
perception of trust is a highly complex topic, and the
dimensions and facets which have been included in
our empirical approach are only a quite arbitrary
selection of attributes. It is obvious that there are
many more aspects which require a closer analysis
in future work.
Another limitation regards the impact of
demographic variables on the perception of trust.
Strictly speaking, one could argue that we only
ICT4AWE 2018 - 4th International Conference on Information and Communication Technologies for Ageing Well and e-Health
70

superficially analysed the impact of the demographic
variables on the perception of trust and
trustworthiness in the area of medical technology.
Even though the results provide interesting insights,
age, gender and health condition are quite rough
categories that need a closer look. Characteristically,
the user factors age and gender are carriers for other
factors, like social and societal attitudes, life
experience, domain knowledge, skills and expertise,
and general wisdom (Ziefle and Schaar, 2011)
which, likewise, might be promising candidates
which shape the trust in the health-supporting
technology. Moreover, age is also connected to
different values on and perspectives of culturally and
societally anchored aging concepts. The moment
users feel old, and the moment they are old might
largely differ, depending on individual perspectives,
but also on cultural and economic dimensions
(Thiede, 2005; Hallenbeck, 2001).
Another limiting factor is the comparably small
sample size. Even though the sample size might be
methodologically and statistically appropriate for the
carried-out analyses, it is still clear that trust and
trustworthiness are inevitably intermingled with
lifelong-learning and the understanding of broader
user groups and cultural diversity. Future studies
should therefore concentrate on more aspects of
trust, using a larger sample size and addressing the
understanding of trust in an intercultural setting.
Last but not least, we should also be aware that
trust in medical technology and care has a policy
component (Mechanic, 1998). In this context, it
should be examined if the perceptions of trust and
trustworthiness also include the competence of the
medical treatments and the education of medical
professionals, the individuals’ confidence in the
national or international efforts for ethical human
care, and the diversity-fair treatment of patients at an
older age (Wilkowska et al., 2018).
5 RESEARCH DIRECTIONS
The mentioned limitations are necessary to outline
some research directions regarding the field of trust
in health-supporting technologies in home
environments.
Decidedly, patients’ trust is an inevitable
component of the future development of medical
innovations that are increasingly implemented in
domestic settings. Health and disease are inherent
parts of humankind, which directly affect people’s
well-being, personal identity formation and life-span
development. Therefore, any technology that seeks
to be supportive for medical treatment and care
needs to consider highly sensitive social issues,
regarding both, physical and mental conditions.
In many cultures being old and ill is perceived as
a stigma (Ziefle and Schaar, 2011) and is directly
related to ageism—the negative societal framing of
age and aging which is difficult to accept. Moreover,
the combination of old age and chronic disease is
closely related to end-of-life emotions, which are
personality issues the patients are highly sensitive to;
however, these also depend on different coping
strategies, framed by societal and cultural values
(Hamel et al., 2017).
In times of big data and the emerging relevance
of the transportation and storage of medical/health
data, electronic services and medical technology
evolve to an enormous marketing good which
contributes to the gain of knowledge on the one, and
marketing success on the other, hand (Vervier et al.,
2017; van Heek et al., 2018). The decision to share
private medical data is therefore a delicate question
for patients who need to weigh up between sharing
their health-related data (and thereby support the
societal medical gain of knowledge) and hiding their
personal data and thus preserving their privacy and
personal identity (Calero Valdez and Ziefle, under
revision; Ziefle et al., 2016b).
Against this background, the present study is
naturally only one drop in the ocean: Digital
medicine and electronic technologies which are
increasingly supporting people in domestic settings
should perpetuate research on trust, privacy, disease
management and aging and could include the
following important research topics:
1) Understanding the different perspectives of
stakeholders. This topic regards consideration of the
entire caring situation, and the different people and
roles as an integral part of it. So far, research
regarding the trust in medical technology mostly
considers the perspective of patients (e.g., Montague
et al., 2009; Wilkowska and Ziefle, 2011,
Wilkowska, 2015). However, the perspective of the
caring personnel, be it of the family or the
professionals, also represents an important point of
view which needs to be integrated in the concept of
trust towards medical technology and treatment.
2) Understanding the impact and course of
disease. The openness to trust and accept medical
technology necessarily depends on the health status.
In addition, it might be essential to consider different
types of disease and etiopathologies. Especially
patients who suffer from chronic and serious
diseases need to cope with the severity of the illness,
the frailness and the end-of-life cognitions in a much
Understanding Trust in Medical Technologies
71

deeper and complex manner than patients with a
temporary need for medical technology.
3) Understanding age and aging. Over time,
cultures form individual and societal values of
aging. These values change in line with economic,
political and societal changes. Therefore, trust in a
technology that supports caring naturally depends on
the societal framing of the value of aging and the
consideration of life-span developments. A recent
study (Hamel et al., 2017) showed that acceptance
patterns of, and trust in, medical care depend on the
culture and the country, the different trade-offs
between societally acknowledged caring mission of
the very old, as well as the aspect of their life-end
decisions (Bowling et al., 2002).
4) Personality of patients. Trust in the medical
technology does not only depend on the caring
context, the nature of the disease and the patients’
age. The ability to trust is also associated with the
personality and the available coping mechanisms of
the concerned person. This part of the research
agenda therefore addresses the patient’s personality
profiles towards trust and their openness for
technical innovations. Particularly, it should be
worked out whether these personal profiles are quite
stable over the life course, or, are rather changing
with age (Knowles et al., 2017).
ACKNOWLEDGEMENTS
The authors thank all participants for their patience
and openness to share opinions on trust in medical
technology. This work has been funded by
Excellence Initiative of Germany’s Federal Ministry
of Education and Research and the German
Research Foundation.
REFERENCES
Abdul-Rahman, A., 2005. A framework for decentralised
trust reasoning. PhD thesis, University College
London, London.
Abras, C., Maloney-Krichmar, D., Preece, J., 2004. User-
centered design. Bainbridge, W. Encyclopedia of
Human-Computer Interaction. Thousand Oaks: Sage
Publications, 37(4), 445-456.
Boon, S. D., Holmes, J. G., 1991. Cooperation and
prosocial behavior, Cambridge University Press.
Cambridge, 1
st
edition.
Bowling, A., Banister, D., Sutton, S., Evans, O., Windsor,
J., 2002. A multidimensional model of the quality of
life in older age. Aging Ment. Heal. 6(4), 355–371.
Broos, A., 2005. Gender and information and
communication technologies (ICT) anxiety: Male self-
assurance and female hesitation. Cyber Psychology &
Behavior, 8(1), 21–31.
Calero Valdez, A., Ziefle, M., under revision. The Users’
Perspective on Privacy Trade-offs in Health
Recommender Systems. International Journal of
Human-Computer Studies.
Cohen, J., 1988. Statistical power analysis for the
behavioral sciences. Hillsdale, NJ: Erlbaum.
Corritore, C.L., Kracher, B., Wiedenbeck, S., 2003. On-
line trust: concepts, evolving themes, a model.
International Journal of Human-Computer Studies,
58(6), 737–758.
Davis, F.D., Bagozzi, R.P., Warshaw, P.R., 1989. User
acceptance of computer technology: a comparison of
two theoretical models. Management science, 35(8),
982–1003.
Demiris, G., Rantz, M.J., Aud, M.A., Marek, K.D., Tyrer,
H.W., Skubic, M., Hussam, A.A., 2004. Older adults'
attitudes towards and perceptions of ‘smart home’
technologies: a pilot study. Medical informatics and
the Internet in medicine, 29(2), 87-94.
Falcone, R., Castelfranchi, C., 2001. The Socio-cognitive
Dynamics of Trust: Does Trust Create Trust? Trust in
Cyber-societies, 2246, 55–72.
Gaul, S., Wilkowska, W., Ziefle, M., 2010. Accounting for
user diversity in the acceptance of medical assistive
technologies. In Proceedings of the 3
rd
International
ICST Conference on Electronic Healthcare for the 21
st
Century, 175–173.
Gefen, D., Straub, D.W., 1997. Gender differences in the
perception and use of e-mail: An extension to the
technology acceptance model. MIS quarterly, 21(4),
389–400.
Hallenbeck, J.L., 2001. Intercultural differences and
communication at the end of life. Primary Care:
Clinics in Office Practice, 28(2), 401-413.
Hamel, L., Wu, B., Brodie, M., 2017. Views and
experiences with end-of-life medical care in the US
[Internet]. Kaiser Family Foundation.
Harrison, A. W., Rainer Jr., R. K., 1992. The influence of
individual differences on skill in end-user computing.
Journal of Management Information Systems, 9(1),
93–112.
Klack, L., Schmitz-Rode, T., Wilkowska, W., Kasugai, K.,
Heidrich, F., Ziefle, M., 2011. Integrated home
monitoring and compliance optimization for patients
with mechanical circulatory support devices. Annals of
biomedical engineering, 39(12), 2911-2921.
Knowles, S.R., Tribbick, D., Connell, W.R., Castle, D.,
Salzberg, M., Kamm, M.A., 2017. Exploration of
health status, illness perceptions, coping strategies,
psychological morbidity, and quality of life in
individuals with fecal ostomies. Journal of Wound
Ostomy & Continence Nursing, 44(1), 69-73.
Lambert, S.D., Loiselle, C.G., 2008. Combining individual
interviews and focus groups to enhance data richness.
Journal of Advanced Nursing, 62(2), 228–237.
ICT4AWE 2018 - 4th International Conference on Information and Communication Technologies for Ageing Well and e-Health
72

Lewis, J.D., Weigert, A., 1985. Trust as a social reality.
Social Forces, 63(4), 967-985.
Li, X., Hess, T.J., Valacich, J.S., 2008. Why do we trust
new technology? A study of initial trust formation
with organizational information systems. The Journal
of Strategic Information Systems, 17(1), 39-71.
Little, L., Marsh, S., Briggs, P., 2007. Trust and privacy
permissions for an ambient world. In Trust in e-
services: Technologies, practices and challenges, pp.
259-292. IGI Global.
Mao, J.Y., Vredenburg, K., Smith, P.W., Carey, T., 2005.
The state of user-centered design practice.
Communications of the ACM, 48(3), 105-109.
Mechanic, D., 1998. The functions and limitations of trust
in the provision of medical care. Journal of Health
Politics, Policy and Law, 23(4), 661-686.
Montague, E.N., Kleiner, B.M., Winchester, W.W., 2009.
Empirically understanding trust in medical
technology. International Journal of Industrial
Ergonomics, 39(4), 628-634.
Montague, E.N., 2010. Validation of a trust in medical
technology instrument. Applied ergonomics, 41(6),
812-821.
Muir, B., 1994. Trust in automation: Part 1. Theoretical
issues in the study and human intervention in
automated systems. Ergonomics, 37, 1905–1923.
Ong, C.-S, Lai, J.-Y., 2006. Gender differences in
perceptions and relation- ships among dominants of e-
learning acceptance. Computers in Human Behavior,
22(5), 816–829.
Pavlou, P.A., Gefen, D., 2004. Building effective online
marketplaces with institution-based trust. Information
systems research, 15(1), 37-59.
Rogers, W.A., Fisk, A.D., 2000. Human factors, applied
cognition, and aging. Lawrence Erlbaum Associates
Publishers.
Sackmann, R., Winkler, O., 2013. Technology generations
revisited: The internet generation. Gerontechnology,
11(4), 493–503.
Schumacher, P., Morahan-Martin, J., 2001. Gender,
internet and computer attitudes and experiences.
Computers in human behavior, 17(1), 95–110.
Siau, K., Shen, Z., 2003. Building customer trust in mobile
commerce. Communications of the ACM, 46(4), 91–94.
Sillence, E., Briggs, P., Harris, P., Fishwick, L., 2006. A
framework for understanding trust factors in web-
based health advice. International Journal of Human-
Computer Studies, 64(8), 697-713.
Thiede, M., 2005. Information and access to health care: is
there a role for trust? Social science &
medicine, 61(7), 1452-1462.
van Heek, J., Himmel, S., Ziefle, M., 2018. Caregivers’
Perspectives on Ambient Assisted Living
Technologies in Professional Care Contexts. 4th
International Conference on Information and
Communication Technologies for Ageing Well and e-
Health (ICT4AWE 2018). SCITEPRESS.
Venkatesh, V., 2000. Determinants of perceived ease of
use: Integrating control, intrinsic motivation, and
emotion into the technology acceptance model.
Information systems research, 11(4), 342–365.
Vervier, L., Zeissig, E.-M., Lidynia, C., Ziefle, M., 2017.
Perceptions of Digital Footprints and the Value of
Privacy. In Proceedings of the International
Conference on Internet of Things and Big Data
(IoTBD 2017), pp. 80-91. SCITEPRESS.
Wang, Y.D., Emurain, H.H., 2005. An overview of online
trust: Concepts, elements and implications. Computers
in Human Behavior, 21, 105-125.
Wilkowska, W., Ziefle, M., 2009. Which factors form
older adults’ acceptance of mobile information and
communication technologies? HCI and Usability for
e-Inclusion, 81-10, Springer.
Wilkowska, W., Ziefle, M., 2011. User Diversity as a
Challenge for the Integration of Medical Technology
into Future Smart Home Environments. In Human-
Centered Design of E-Health Technologies, Hershey
PA, 95-126.
Wilkowska, W., 2015. Acceptance of eHealth Technology in
Home Environments: Advanced Studies on User
Diversity in Ambient Assisted Living. Apprimus,
Aachen.
Wilkowska, W., Brauner, P., Ziefle, M., 2018. Rethinking
Technology Development for Older Adults. A
responsible research and innovation duty. In Aging,
Technology, and Health. Elsevier North Holland.
Ziefle, M., Schaar, A.K., 2011. Gender differences in
acceptance and attitudes towards an invasive medical
stent. Electronic Journal of Health Informatics, 6(2),
e13.
Ziefle, M., Röcker, C., Holzinger, A., 2011. Medical
technology in smart homes: exploring the user’s
perspective on privacy, intimacy and trust.
In Computer Software and Applications Conference
Workshops (COMPSACW), IEEE 35th Annual, pp.
410-415.
Ziefle, M., Brauner, P., van Heek, J., 2016a. Intentions to
Use Smart Textiles in AAL Home Environments:
Comparing Younger and Older Adults. In
International Conference on Human Aspects of IT for
the Aged Population, Springer International
Publishing.
Ziefle, M., Halbey, J., Kowalewski, S., 2016b. Users’
willingness to share data in the Internet: Perceived
benefits and caveats. In Proceedings of the
International Conference on Internet of Things and
Big Data (IoTBD 2016), pp. 255-265. SCITEPRESS.
Zmud, R.W., 1979. Individual differences and MIS
success: A review of the empirical literature.
Management Science, 25(10), 966–979.
Understanding Trust in Medical Technologies
73
