
Insufficient Behavioral Change Skill Hampers Adoption of Ehealth
Services
Miriam Vollenbroek-Hutten
1,2
, Tess Goolkate
2
, Michele Lankheet
2
, J. H. (Han) Hegeman
1
,
Gozewijn Dirk Laverman
1
and Bert-Jan van Beijum
2
1
ZiekenhuisGroep Twente, Zilvermeeuw 1, Almelo, The Netherlands,
2
University of Twente, Drienerlolaan 5, Enschede, The Netherlands
{g.laverman, h.hegeman}@zgt.nl
Keywords: Behavioural Change, Self Management, ICT Tools, Development, Implementation.
Abstract: This study aims to get, starting from behavioural change theories, a better understanding of the perceptions
of patients regarding their own responsibility for promoting their health and to translate this into
requirements for development and implementation of eHealth services. Nineteen patients with Diabetes
Type 2 and nine older adults (>65 years) with lower limb or hip fracture were interviewed. The topic list
was based on the Self-Determination Theory, the Theory of Change and the Social Cognitive Theory and
included Autonomy, Relatedness, Competence, Motivation, Skills and Knowledge. Results show that both
patient groups have insufficient knowledge about proper health management. In addition, patients with
Diabetes Type 2 appear to be insufficiently motivated for life style changes with outcomes that become
apparent mainly in long-term. Patients with lower limb or hip fractures are in contrast highly motivated but
lack autonomy, competence and skills. Both patients groups feel positively influenced by relatives, rely to a
large extent on or have a wish for more in depth involvement of the professionals. These issues will
probably hamper patients from becoming proactive in improving their health and using technology but are
expected to be solvable when addressed in the development of the technologies as well as with
implementing in daily health care.
1 INTRODUCTION
The increasing number of older adults as well as our
unhealthy lifestyle put an increasing pressure on our
western health care systems, both in terms of
demand for care and costs. In addition, due to the
dejuvenation the labour capacity in health care is
expected to decrease. These trends make that there is
an urgent need to find solutions that keep our health
care sustainable and affordable. Solutions are sought
in the field of prevention, improving self-
management of patients, technological innovations
or a combination of these. eHealth services are
considered promising in this respect. eHealth is
defined (WHO) as the use of information and
communication technologies for health. However,
the term characterizes not only a technical
development, but also a state-of-mind, a way of
thinking, an attitude, and a commitment for
networked, global thinking, to improve health care
locally, regionally, and worldwide by using
information and communication technology
(Eysenbach, 2001). Examples of eHealth are digital
information provision, remote monitoring, remote
treatment, e-consultation and online patient-to-
patient or professional to professional contact.
In contrast to the huge amount of eHealth
products developed and tested in research projects,
the penetration of eHealth into daily care practice is
still very limited. Partly motivated by this,
acceptance of technology has been studied to a large
extent and has resulted in several theoretical
frameworks. These frameworks state that technology
acceptance is influenced by various factors.
Technology acceptance that refers to an attitude
towards a technology is different from technology
adoption. Technology adoption is a process –
starting with the user becoming aware of the
technology, and ending with the user embracing the
technology and making full use of it. Someone who
has embraced a technology is likely to replace the
item if it breaks, find innovative uses for it, and
Vollenbroek-Hutten, M., Goolkate, T., Lankheet, M., Hegeman, J., Laverman, G. and van Beijum, B.
Insufficient Behavioral Change Skill Hampers Adoption of Ehealth Services.
DOI: 10.5220/0006675501190125
In Proceedings of the 4th International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AWE 2018), pages 119-125
ISBN: 978-989-758-299-8
Copyright
c
2019 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
119

cannot contemplate life without it. Adoption as such
can only be studied after implementation. In
community-dwelling older adults this research is
still scarce (Peek et al., 2014). (Heart and Kalderon,
2013) showed that modern technologies have been
adopted (albeit selectively) by older users, who were
presumably strongly motivated by perceived
usefulness They showed that, concerning health
related ICT, adoption of technology by older adults
is still limited, though it has increased. Particularly
worrying are the effects of health, perceived
behavioural control, and the fact that many older
adults do not share the perception that ICT can
significantly improve their quality of life. As such,
health-related ICT should be kept simple and
demonstrate substantial benefits, and special
attention should be paid to training and support and
to specific personal and cultural characteristics.
This latter is indeed is considered important as a
lot of eHealth services requires the patient to take
action and become pro-active. Something they
probably did not do before in relation to receiving
care. Obvious advantages of this approach are a
more equivalent position of patients with respect to
health care professional and patients get more
possibilities to influence their own care process and
their quality of life. However in clinical practice
doubt often rises whether patients have the capacity
to take this responsibility. We assume we can learn
here from behavioural sciences by the fact that
taking a pro-active role when not having done this
before can be considered a behavioural change. We
all know that changing behaviour is notoriously
difficult. There are several theories that try to
understand the process of behavioural change.
Examples are; the Transtheoretical Model
(Prochaska and DiClemente, 2005) which assumes
that in the behavioural change process various stages
are discerned, i.e. precontemplation, contemplation,
preparation, action, maintenance and termination;
the Social Cognitive Theory (Bandura, 1977) in
which one the main constructs is self-efficacy. Self-
efficacy focuses on an individual’s belief in one’s
capability for change; and the Self-Determination
Theory (Ryan and Deci, 2000) which is a theory of
motivation and is concerned with supporting our
natural or intrinsic tendencies to behave in effective
and healthy ways. This theory differentiates between
intrinsic and extrinsic motivation and proposes three
main intrinsic psychological needs that motivate the
self to initiate behaviour. These include the need for
competence, autonomy, and psychological
relatedness (Ryan and Deci, 2000). Taking these
theories together, changing behaviour occur along
different stages. People move from one stage to the
other but can also fall back. Changing behaviour will
be enhanced when patients are motived and this is
more likely when this changed behaviour contributes
to competence, autonomy and relatedness. However,
merely motivation is not sufficient. To be able to
change successfully, patients must be convinced of
the need to change and feel that they can show the
desired behavior.
So far, hardly any attention has been devoted to
the behavioural change readiness of older adults to
adopt eHealth technology as well as to its
consequence for the development and
implementation of eHealth. We hypothesize that
adoption of eHealth services by older adults is
hampered as they are insufficiently equipped to
change their behaviour. Assumptions for this come
from literature that states that older adults might
experience problems in recognising relevant issues
and act in advance and care dependency rises when
people grew old (World Health Organization, 2015).
In addition, literature shows that older adults seemed
to eschew pro-active coping by prioritizing present
emotional well-being and avoiding thoughts of
future risks, (Gould et al., 2015). Not all of them are
future oriented or inclined to prepare themselves for
potential goal threats to the same extent (Ouwehand,
de Ridder and Bensing, 2008).
The aim of this study was to get, starting from
behavioural change theories, a better understanding
of the perceptions of patients regarding their own
responsibility for promoting health and translate this
into requirements for the development and
implementation of eHealth services. We performed a
qualitative study in two separate populations, 1)
patients with complicated Diabetes Mellitus type 2
treated at the outpatient clinic of a hospital and 2)
older patients (age >65 years) with a lower limb or
hip fracture who, after surgery, had been dismissed
from the hospital to a geriatric rehabilitation ward or
a nursing home.
2 METHODS
A qualitative research was conducted.
2.1 Participants
Diabetes Patients. Patients with diabetes type 2
visiting the outpatient clinic of Internal Medicine
were asked to participate. Patients were included if
1) diagnosed with diabetes type 2, 2) aged 18 years
or older and 3) follow-up is taking place in the
ICT4AWE 2018 - 4th International Conference on Information and Communication Technologies for Ageing Well and e-Health
120
outpatient clinic in the hospital. Participants were
excluded if they: 1) had severe general disease or
mental disorders making participation impossible
and 2) suffer from drug abuse. During the time
period set for inclusion of patients for this research,
28 patients were approached for inclusion. Of these
28 patients, 9 were hindered due to personal
circumstances or illness. In total, 19 patients
participated.
Older Adults with Lower Limb or Hip Fracture.
Participants were recruited from four nursing homes
working together with the hospital where patient
underwent the surgery. Patients were included if
they 1) were 65 years of age or older, 2) were
diagnosed with a lower limb or hip fracture, 3)
treatment goal was to return to their own living
situation before fracture, 4) were able to
communicate in Dutch, 5) had no marked cognitive
impairment(s). Participants were excluded if they 1)
had progressive neurological disease (e.g.,
Parkinson’s disease), 2) had severe multi-morbidity
(somatic, psychiatric and/or psycho-geriatric). A
total of 9 participants participated in this study. The
study is registered as non-WMO research and got a
feasibility approval from the hospital.
All participants signed informed consent prior to
participating in this study.
2.2 Interview
Semi structured interviews were performed at
premises of the health care institute. The topic list
for the interviews was derived based on the Self-
Determination Theory, the Theory of Change and
the Social Cognitive Theory and developed in
brainstorm sessions with social researchers. The
topic list included the following items: autonomy,
relatedness, competence, motivation, skills,
knowledge and use of technology.
2.3 Analysis
The interviews were recorded and afterwards
transcribed in Microsoft Word. The analysis of the
interviews was performed differently for both cases.
For the diabetes patients, the transcribed
interviews were uploaded in Atlas.ti 8.0 and coded
by means of a coding scheme. One researcher coded
the interviews. Each code was based on the topics
included in the interviews, as mentioned above.
Hereby for each topic the codes were divided into
the different answer possibilities, negative or
positive, in order to allow evaluation of the codes
based on their frequency, per code. Sentences
corresponding with more codes were coded double,
so that each of the codes is covered. When in doubt,
a code was not assigned to a sentence.
For the patients with a lower limb or hip fracture
it was difficult to follow the structure of the
interview as defined. Patients were not always able
to interpret the questions correctly and began to talk
about common things. However, with help of the
topic list, face-to-face contact and observation of the
patient, interesting information could be distilled
regarding the topics of interest. A thematic analysis
(Braun and Clarke, 2006), a method for identifying,
analysing, and reporting patterns (themes) within
data, was carried out according the following steps.
First the transcripts were read and re-read and
checked for patterns of themes among the data. It
was decided to remove all information deemed
unnecessary from the interviews. The unnecessary
information consisted mainly of answers that were
not related to the various components. The result
was a list including all important quotes. For every
important quote we checked whether it was related
with an item of the topic list: autonomy,
competence, relatedness, knowledge, skills,
motivation, and technology or not. It was possible
that in certain quotes several components were
involved.
3 RESULTS
3.1 Patient Characteristics
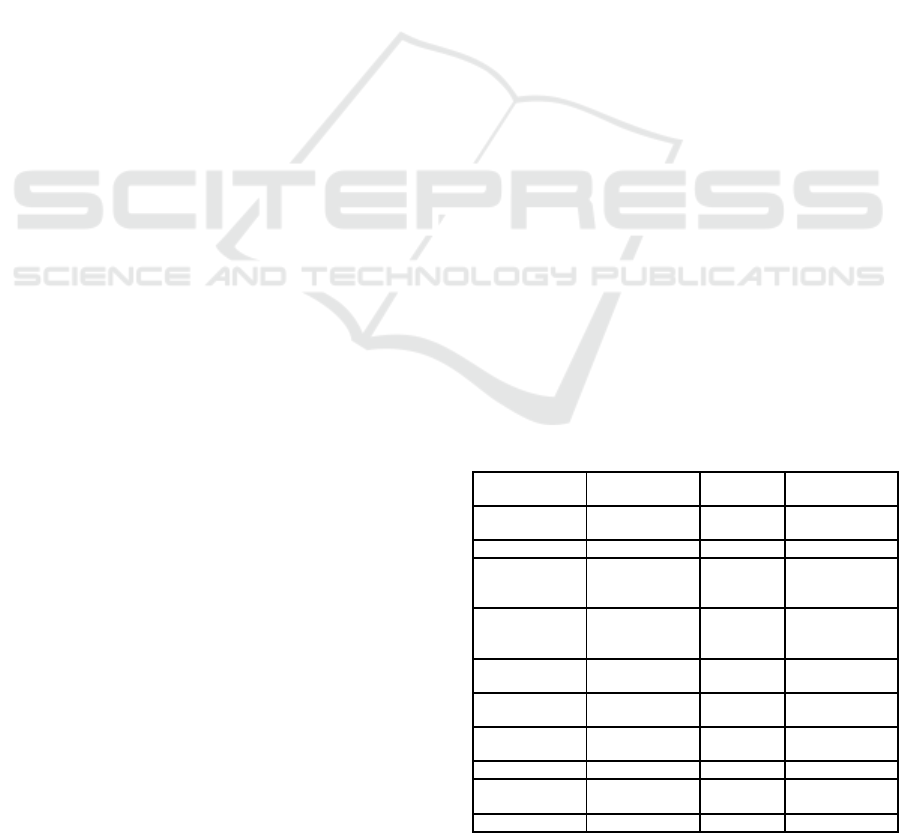
Table 1 presents the characteristics of the patients
that participated in this study.
Table 1: Patient characteristics.
Characteristics Diabetes
(N = 19)
Lower limb or hip
fracture (N=9)
Gender
number (%)
Male 12 (63) 1 (11)
Female 7 (37) 8 (89)
Age
average (standard
deviation)
64 (11) 86 (4)
Diabetes
Complications
number (%)
Any type of
complication
14 (74)
Macrovascular
complications
5 (26)
Microvascular
complications
13 (69)
Fracture
number (%)
Hip fracture 7 (78)
Pelvic fracture 2 (22)
Cognitive
impaired (yes/no)
Yes 3 (33)
No 6 (67)
Insufficient Behavioral Change Skill Hampers Adoption of Ehealth Services
121

3.2 Interview Results
3.2.1 Diabetes
Autonomy. Almost all patients mentioned to be
able to make their own choices with regard to their
diabetes control as well as with respect to treatment
choices like medication, doctors, contact moments,
healthy exercise, nutrition, et cetera. Only a small
part of the patients reported not to be so sure about
the ability to make own choices and they just do
what the doctor says.
Competence. When we talk about competence, we
refer to self-efficacy, which means in this study:
one’s belief in their ability to succeed in taking own
responsibility or accomplish a task or activity.
Nearly all patients stated to be positive about their
capabilities and mentioned that they do not need any
support to further improve.
Motivation. A majority of the patients is
intrinsically motivated to perform actions that
improve their diabetes outcomes on short notice i.e.
their blood glucose levels and/or general feeling of
wellbeing. Concerning lifestyle habits, patients want
to change their lifestyle but only in case this
immediately affects their diabetes or fitness level.
Though patients in general have insufficient
knowledge whether and which habits do have
positive influences. In addition, they state to have
difficulties to maintain these healthy habits.
Relatedness. Most patients are positive about
support by relatives like family and friends.
Concerning caregiver support, patients mentioned to
be positively informed by their diabetes doctor,
diabetes nurse, or dietician. However, patients
consider professional support only minimal, and not
very in-depth
Knowledge. Patients were asked to answer 12
questions about the impact of nutrition and exercise
on diabetes and its complications. Results showed
that most of the patients showed insufficient
knowledge (less than 6 questions properly answered)
concerning health lifestyle.
Skills. A majority of the patients indicate to have
sufficient skills to adequately deal with their
diabetes. The minority which is not, mentioned
problems with medication, blood glucose
measurements, insulin injections, healthy exercise
and nutrition. Concerning exercises the majority of
the patients is able to perform exercises. Those who
are not mentioned external factors or other diseases
withholding them to do so.
3.2.2 Lower Limb or Hip Fracture
Autonomy. All patients with lower limb or hip
fracture lived in their own home before admission to
the geriatric rehabilitation ward of the nursing home.
Some needed help from home care and/or lived in a
sheltered housing accommodation. Once in
rehabilitation patient often referred to the home
situation before admission. They were fine with this
situation and hope to return to this situation again.
After the fracture almost all participants experience
less or no autonomy. Autonomy increases during
rehabilitation for all participants, however, each at
their own pace and to their own degree. The
autonomy of patients for their own rehabilitation
program is rather low. With the help of the
physiotherapist the exercises can be performed, but
the exercises are barely pursued independently. No
or only little own initiative was taken to fulfil
exercises or a activity such as walking around the
corridor.
Competence. After the fracture, the level of
confidence is rather low in almost all patients. Most
of them report to be afraid to fall again. As a
consequence, they fully rely on the care
professionals to tell them what they are allowed to
do.
Relatedness. The participants feel very related to
the nursing staff, and other professionals who are
helping them during the rehabilitation process. This
is not unexpected because of their increased
dependency after the fracture. However, this
dependency creates a certain hierarchy between the
nursing staff and patients that hampers the patient to
take initiative or ask something. Another aspect that
appears to be important here is support from family
which strongly motivates the patient. In addition
they also give the patient a feeling that their
competence and skills are sufficient to take own
responsibility.
Motivation. Many participants have already
reached a certain age and are satisfied with what
they did. They are intrinsically motivated to recover
because they want to go home again and do the
things they did before, like doing the groceries and
other household chores.
ICT4AWE 2018 - 4th International Conference on Information and Communication Technologies for Ageing Well and e-Health
122
Knowledge. Most participants have very limited
knowledge about the rehabilitation process. They do
not understand that all activities they perform during
the day is actually rehabilitation. In addition they
have limited knowledge about the exercises offered
in terms of why and how they need to be performed.
The participants do the exercises that they have to do
only during the physiotherapy
Skills. Skills are present to perform the exercises
at the physiotherapy. However, cognitive skills are
often low which hampers executing exercises,
independently. In addition, physical condition is
often reduced meaning that skills needed to go for a
'long' walk are absent.
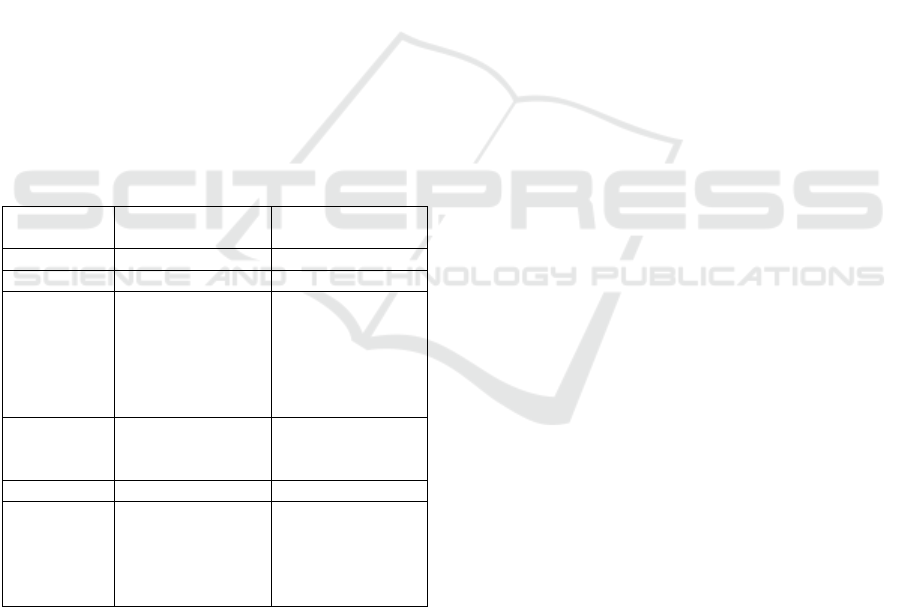
The results presented above are summarized in
table 2. It becomes clear that both patients with
diabetes type 2 and patients with a lower limb or hip
fracture are insufficiently equipped on one or more
behavioural change aspects. For patient with
diabetes type 2 this concerns knowledge and
motivation. For patients with lower limb fracture all
aspects, except motivation, are insufficiently
present.
Table 2: summary of the interview results.
Topic Diabetes Lower limb or hip
fracture
Autonomy Sufficient Low
Competence Sufficient / variable Low, fear of falling
Relatedness Positive for
relatives/health
professionals. Wish
for more in depth
support from health
professionals
Dependency of
health professionals.
Relatives important
to enhance all other
factors
Motivation Sufficient when
direct effects. Low
for long term
High intrinsic
motivation
Knowledge Insufficient Insufficient
Skills Variable due to
other health
problems
Insufficient
Variable due to
cognitive problems
or other health
problems
3.3 Requirements for Development and
Implementation of Ehealth Services
Those behavioural change aspects that are
insufficiently present will probably impede patients
in deploying a proactive behaviour in their health
management. It will also hinder the adoption of
eHealth services that are developed for this purpose
in case these aspects are insufficiently addressed
during its development and implementation. Our
finding that the two patient groups score different on
the respective elements demonstrates that the
requirements for development and implementation
of eHealth services are also different to some extent.
3.3.1 Development
Diabetes patients will be capable of using
technologies. Technologies that support them in
lifestyle choices thereby improving their short-term
diabetes outcomes will have the highest chance on
adoption. In contrast, technologies that support
them in lifestyle choices that aim at long term
outcomes will probably not be used or lose attention
after a period of time. One aspect that needs to be
considered here is patients’ knowledge regarding the
importance of healthy lifestyle. As this is
insufficient they are unable to fully understand its
importance. Knowledge transfer is as such a
prerequisite for future technologies. The fact that
patients are motivated to come into action when
direct effects on their diabetes outcome are
experienced, requires the technology to incorporate
motivational strategies with feedback on short term
outcomes. Feedback on blood glucose levels when
focusing on active lifestyle will as such be more
suitable than feedback on steps taken. Patients feel
instantaneously better by proper blood glucose
levels but proper blood glucose regulation is also
positive for outcomes on long term. As patients
differ in knowledge level and skills, technology
should be personalized and it should incorporate
small incremental goal setting possibilities.
The patient with a lower limb or hip fracture will
probably not be able start using technology by
themselves. As they are intrinsically highly
motivated to go back to their home situation and rely
on the health professionals they will probably adopt
and start using technologies when others ‘prescribe’
or use the technology with them. In this case
technology that starts the interaction might be very
useful. In addition, the technology for this patient
group should focus on enhancing competence,
knowledge and skills. For competence, technology
should convince the patient that they can act safely
or technology should act like the nursing staff and
relatives are doing and give the patient the feeling
that they can rely on it. An example of this is
incorporating affirmative cues when being used or a
virtual presentation of the person(s), patients rely
on. Knowledge transfer is considered to be
important to overcome their knowledge gap but
Insufficient Behavioral Change Skill Hampers Adoption of Ehealth Services
123

since cognitive skills are often insufficient for this
purpose, technology that acts as an extension of the
patient’s cognition is expected to be more effective.
This holds true for example when the technology
acts as a memory (provides reminders or provides a
schedule), guides and coaches the patients when
performing a complex task. Again, there is high
between-patient variability in feeling of competence,
the cognitive and physical skills, which warrants the
technology to be personalized.
3.3.2 Implementation
Next to the impact on development, the results do
also have consequences for the implementation of
eHealth services in daily care practice. As most
diabetes type 2 patients and patients with lower limb
or hip fracture have insufficient knowledge, patients
need additional support to gain this knowledge. It is
doubtful whether this can be reached by technology
solely. So in this respect it is important that
professionals support patients to gain more in depth
knowledge. This knowledge is necessary before start
using technology but probably also during the usage
of technology. As such, technology should be
implemented as a blended care concept. As patient
and especially patients with lower limb or hip
fracture rely to a large extent on health care
professionals, it is important that the health care
professionals become more aware of this and either
‘prescribe’ the technology but even better guide the
patient in the process to come to shared decision
making. In this shared decision making the caregiver
supports the patient in becoming well-informed on
the subject of their illness and possible options for
improvement. In this improvement plan, it is again
important that the professionals support the patient
in adequate goal setting in which the patient’s
preferences and possibilities are carefully
considered. Here it is also important to discuss what
is expected from the patient and what can be
expected from the professional. Both patients with
diabetes type 2 and patients with lower limb or hip
fracture feel positively supported by relatives. For
patients with lower limb fracture this even goes one
step further as the closest family is considered an
extended self for each of the behavioural change
elements. Based on this it is very important that
relatives are explicitly involved in the
implementation process.
4 DISCUSSION
The aim of this study was firstly to get, starting from
behavioural change theories, a better understanding
of the perception of older patients regarding their
own responsibility for promoting their health.
Secondly, to translate this into requirements for
development and implementation of eHealth
services. Results show that both patients with
diabetes type 2 and patients with a lower limb or hip
fracture, are insufficiently equipped to become
proactive in improving their health as well as in
using technology for this purpose. These problems
can be addressed and solved when explicitly
considered in the development of the technologies as
well as taken into account when implementing these
technologies in daily health care work flows and
processes.
An important finding of this study is the
difference between the patient groups. Where
patients with diabetes type 2 score low on
knowledge and motivation and to some extent on
skills, patients with lower limb or hip fracture are
highly motivated but have low levels of autonomy,
competence, knowledge and skills. These
differences can partly be explained by intrinsic
differences between the patient groups. The diabetes
type 2 patients investigated here suffer from this
disease usually more than ten years and have a
history of disappointments from previous initiatives
aimed to improve their lifestyle, such as weight-loss.
This significantly affects their motivation. Patients
with a lower limb or hip fracture, in contrast, are
dealing with the consequence of a sudden single
event that can heal again. As such they are highly
motivated to contribute to this. Another difference
between both groups is the age. The high age of the
patients with lower limb or hip fracture probably has
affected their competence, skills and knowledge.
These differences also result in different
requirements for the technology but remarkably not
for the implementation in daily practice
Concerning the development, technology should
have a function as information channel for both
patient groups. For patient with diabetes, special
attention should be paid to motivational strategies.
Currently, various motivational strategies are being
developed like short feedback loops with
motivational messages (Achterkamp, Hermens and
Vollenbroek-Hutten, 2016) and gamification (de
Vette et al., 2015). As patients will be most
motivated when they see or feel direct benefits,
feedback on blood glucose level is considered to be
most effective. For patients with lower limb fracture
ICT4AWE 2018 - 4th International Conference on Information and Communication Technologies for Ageing Well and e-Health
124

it is suggested that technology that acts as extended
self could be an option. The thought behind this is
comparable with a detachable or permanent
prosthesis (Murray, 2004) that is accepted as part of
their body and in this case as a cognitive prosthesis.
A cognitive prosthesis implies that the information
gathered is an extension of the individual’s cognitive
understanding, can be used to outsource work (de
Preester and Tsakiris, 2009) and make the job done
easier. Another way forward in the development for
this patient group might be technology that is a
virtual representation of those they rely on being
health professional or relatives and speak and deal
with the patients as natural persons do.
Concerning implementation aspects that need to
be considered are more equal between both patient
groups and concern: implementation as blended care
concept, working to shared decision with optimal
involvement of relatives. This will urge our health
care system to educate health care professionals in
doing so.
5 CONCLUSION
Uptake of eHealth services by patients is hampered
by the fact that patients are insufficiently equipped
for this. The age of patients and the disease history
are partly responsible for this. In addition the pro-
active role being asked for is also considered a
phenomenon patients are not used to. Uptake of
eHealth can be enhanced when these behavioural
changes elements are explicitly considered in the
development of the technologies as well as when
implementing these technologies in daily health care
work flows and processes.
REFERENCES
Achterkamp, R., Hermens, H. J. and Vollenbroek-Hutten,
M. M. R. (2016) ‘The influence of vicarious
experience provided through mobile technology on
self-efficacy when learning new tasks’, Computers in
Human Behavior. Elsevier Ltd, 62, pp. 327–332. doi:
10.1016/j.chb.2016.04.006.
Bandura, A. (1977) ‘Self-efficacy: Toward a unifying
theory of behavioral change’, Psychological Review,
84(2), pp. 191–215. doi: 10.1037/0033-295x.84.2.191.
Braun, V. and Clarke, V. (2006) ‘Using thematic analysis
in psychology’, Qualitative Research in Psychology,
3(2), pp. 77–101. doi: 10.1191/1478088706qp063oa.
Eysenbach, G. (2001) ‘What is e-health?’, Journal of
Medical Internet Research.
Gould, O. N. et al. (2015) ‘Hoping for the Best or
Planning for the Future’, Journal of Applied
Gerontology, p. 73346481559121. doi: 10.1177/07334
64815591213.
Heart, T. and Kalderon, E. (2013) ‘Older adults: Are they
ready to adopt health-related ICT?’, International
Journal of Medical Informatics, 82(11). doi:
10.1016/j.ijmedinf.2011.03.002.
Murray, C. D. (2004) ‘An interpretative phenomenological
analysis of the embodiment of artificial’, Disability
and rehabilitation, 26(16), pp. 963–973. doi:
10.1080/09638280410001696764.
Ouwehand, C., de Ridder, D. T. D. and Bensing, J. M.
(2008) ‘Individual differences in the use of proactive
coping strategies by middle-aged and older adults’,
Personality and Individual Differences, pp. 28–33.
doi: 10.1016/j.paid.2008.02.013.
Peek, S. T. M. et al. (2014) ‘Factors influencing
acceptance of technology for aging in place: A
systematic review’, International Journal of Medical
Informatics, pp. 235–248. doi: 10.1016/j.ijmedinf.
2014.01.004.
de Preester, H. and Tsakiris, M. (2009) ‘Body-extension
versus body-incorporation: Is there a need for a body-
model?’, Phenomenology and the Cognitive Sciences,
8(3), pp. 307–319. doi: 10.1007/s11097-009-9121-y.
Prochaska, J. and DiClemente, C. (2005) ‘The trans-
theoretical approach’, Handbook of Psychotherapy …,
pp. 147–171. doi: 10.1002/ejoc.201200111.
Ryan, R. and Deci, E. (2000) ‘Self-determination theory
and the facilitation of intrinsic motivation, social
development, and well-being.’, The American
Psychologist, 55(1), pp. 68–78. doi: 10.1037/0003-
066X.55.1.68.
de Vette, F. et al. (2015) ‘Engaging Elderly People in
Telemedicine Through Gamification’, Journal of
Medical Internet Research Serious Games, 3(2), p. e9.
doi: 10.2196/games.4561.
Insufficient Behavioral Change Skill Hampers Adoption of Ehealth Services
125
