
Heart Rhythm Analysis using ECG Recorded with a Novel Sternum
based Patch Technology
A Pilot Study
Dorthe B. Saadi
1,2
, Inge Fauerskov
3
, Armin Osmanagic
3
, Hussam M. Sheta
3
, Helge B. D. Sorensen
2
,
Kenneth Egstrup
3
and Karsten Hoppe
1
1
DELTA Dansk Elektronik, Lys & Akustik, Venlighedsvej 4, 2970 Hørsholm, Denmark
2
Electrical Engineering, Technical University of Denmark, Ørsteds Plads, Bldg. 349, 2800 Kgs. Lyngby, Denmark
3
Department of Medical Research, OUH Svendborg Hospital, Valdemarsgade 53, 5700 Svendborg, Denmark
Keywords: Long-term ECG Monitoring, Home Cardiac Monitoring, Sternum ECG, Patch ECG Recorder.
Abstract: According to the World Health Organization, cardiovascular diseases are the number one cause of death
globally. Early diagnosis and treatment of many of these patients depend on ambulatory electrocardiography
recordings. Therefore a novel wireless patch technology has been designed for easy, reliable long-term ECG
recordings. The device is designed for high compliance and low patient burden. This novel patch technology
is CE approved for ambulatory ECG recording of two ECG channels on the sternum. This paper describes a
clinical pilot study regarding the usefulness of these ECG signals for heart rhythm analysis. A clinical
technician with experience in ECG interpretation selected 200 noise-free 7 seconds ECG segments from 25
different patients. These 200 ECG segments were evaluated by two medical doctors according to their
usefulness for heart rhythm analysis. The first doctor considered 98.5% of the segments useful for rhythm
analysis, whereas the second doctor considered 99.5% of the segments useful for rhythm analysis. The
conclusion of this pilot study indicates that two channel ECG recorded on the sternum is useful for rhythm
analysis and could be used as input to diagnosis together with other clinical tests and medical history.
1 INTRODUCTION
According to the World Health Organization (2013),
cardiovascular diseases (CVDs) are the number one
cause of death globally. They state that CVDs were
responsible for 30% of all deaths in 2008.
CVDs are not only lethal, but they are also
associated with a high economic burden on the
healthcare system. Furthermore, diseases like
ischemic stroke can have high human costs and
decrease significantly the quality of life. Early
diagnosis and treatment of cardiac related diseases is
therefore crucial. For more than hundred years, the
12-lead electrocardiogram (ECG) has served as the
“gold standard” for diagnosis of different heart
conditions, including arrhythmias (Mittal et al.,
2011). The well-chosen and standardized selection
of electrode positions allows a full investigation of
different projections of the electrical activity of the
heart. This allows a careful investigation of the heart
in different “spatial plans”.
However, for some conditions, it is more
important to obtain long-term information about the
general rhythm of the heart from a rhythm analysis.
In this case, an ambulatory long-term ECG
recording is desired. Some examples of conditions
that are not sufficiently managed by baseline 12-lead
ECG recordings are paroxysmal atrial fibrillation
(AF), non-sustained ventricular tachycardia,
unexplained episodes of syncope, and diagnosis of
other cardiac symptoms not explained by a baseline
12-lead resting ECG (Mittal et al., 2011),
(Zimetbaum and Goldman, 2010). It is, however,
important to notice the different possibilities with a
standard 12-lead ECG and an ambulatory recording.
Some of the main advantages of ambulatory ECG
recordings are long monitoring period, detection of
paroxysmal and asymptomatic arrhythmias, remote
monitoring of the patient and correlation between
specific symptoms and the ECG signals.
It is however still important that the ambulatory
long-term ECG recordings have a sufficient quality
for analysis of specific ECG patterns. Some of the
15
Saadi D., Fauerskov I., Osmanagic A., M. Sheta H., B. D. Sorensen H., Egstrup K. and Hoppe K..
Heart Rhythm Analysis using ECG Recorded with a Novel Sternum based Patch Technology - A Pilot Study.
DOI: 10.5220/0004640900150021
In Proceedings of the International Congress on Cardiovascular Technologies (CARDIOTECHNIX-2013), pages 15-21
ISBN: 978-989-8565-78-5
Copyright
c
2013 SCITEPRESS (Science and Technology Publications, Lda.)
key features in rhythm analysis include the
depolarization of the atria (the P-wave) and the
depolarization of the ventricles (the QRS complex).
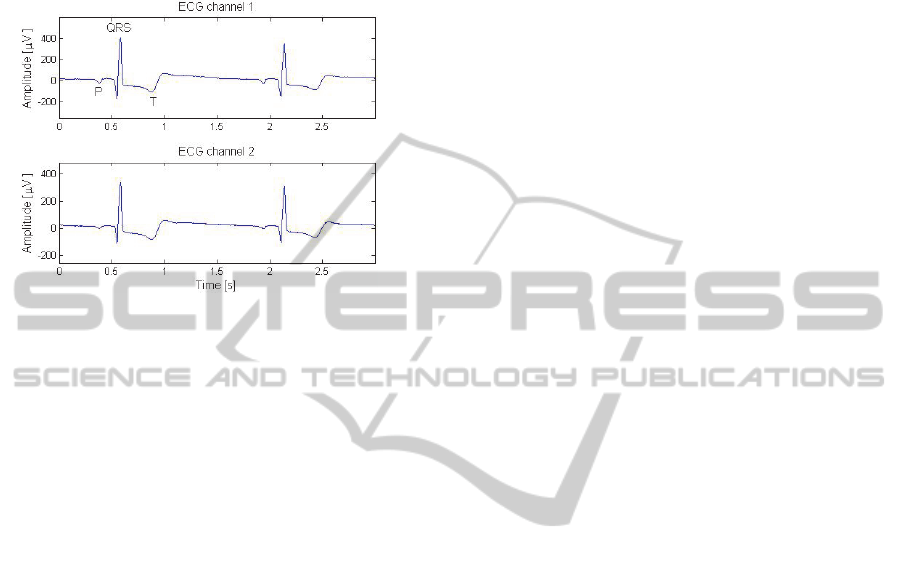
An example of a short unfiltered ECG segment
recorded with the ePatch is provided in Figure 1.
Figure 1: Illustration of a normal sinus rhythm ECG
recorded with the novel ePatch technology. The important
ECG markers are indicated in channel 1 for one heart
cycle. The ECG is raw without any digital filtering.
A number of different long-term ambulatory
monitoring techniques are accepted today. One of
the most commonly applied ambulatory ECG
recorders is the HOLTER monitor.
1.1 Traditional Holter Analysis
The HOLTER monitor typically records 2 – 3 ECG
leads continuously for 24 – 48 hours (Zimetbaum
and Goldman, 2010). During a traditional HOLTER
recording, a medical technician attaches the
electrodes and the HOLTER recorder to the patient.
The electrodes are attached to the recorder through
wires. After the monitoring period, the recorder with
the ECG data is returned to the hospital or healthcare
facility. At the hospital, a specially trained nurse
looks through the recorded data using automatic
software and generates a report for the referring
medical doctor. This report contains a general
description of the rhythm during the recording, any
special findings, and a number of descriptive ECG
“snippets” displaying the different rhythms found
during the recording. The report serves as input to
the diagnosis together with other clinical tests and
the medical history of the patient. If the recording is
of sufficient quality, the following parameters may
be determined based on a traditional HOLTER
recording: Average heart rate and heart rate range,
quantification of atrial and ventricular ectopic beats,
and determination of whether AF is present –
including information about pattern of AF initiation
and termination, shortest and longest duration of AF,
heart rate during AF and AF burden (Mittal et al.,
2011).
However, this monitoring technique possesses a
number of disadvantages including cables that affect
the ability to perform some daily activities during
the recording and the lack of real-time data
transmission and analysis. Furthermore, the
relatively short monitoring duration might not be
sufficient for investigation of infrequent arrhythmias
(Zimetbaum and Goldman, 2010), (Rosenberg et al.,
2013). To account for some of these disadvantages,
a novel wireless ECG patch technology was
designed.
1.2 The ePatch Technology Platform
The ePatch heart monitoring platform is designed
according to a “wear and forget” principle. Thus, the
device is designed to be reliable, safe, comfortable
and easy to use for both the patient and the
healthcare professionals. The ePatch is designed as a
technology platform that can be customised to
account for the needs in a high variety of situations.
Some of the advantages and possibilities with this
novel technology platform are listed below:
Possibility of multi-sensor design with e.g.
accelerometer recordings for activity estimation.
Splash proof design: Patients can shower while
wearing the ePatch.
No cables are needed to connect the electrodes to
the recording device. This highly increases the
patient comfort and decreases the patient burden.
Possibility of wireless data transmission and/or
local data storage. The platform can be adapted
to any desired communication protocol.
Home monitoring of cardiac patients that might
reduce hospitalizations.
Possibility of long-term monitoring due to the
expected higher patient comfort and compliance
with wearing the device.
Module design allows easy adaptation to
different applications.
Real-time embedded signal processing, e.g.
automatic detection of cardiac events.
In this pilot study, the focus is to investigate the
application of the ePatch for heart rhythm analysis.
The ePatch version applied in this study is CE
approved for 24 hour ambulatory ECG recordings,
and the ECG signals are stored locally on an internal
memory. An illustration of the applied ePatch is
provided in Figure 2. As observed from Figure 2, the
ePatch is placed at the sternum.
CARDIOTECHNIX2013-InternationalCongressonCardiovascularTechnologies
16

Figure 2: Illustration of the placement of the ePatch
electrode and sensor on the sternum.
The ePatch system consists of two parts: 1) A
bio-compatible, single-use adhesive electrode with
multiple skin contact points that is attached directly
to the skin surface (this part is termed the ePatch
electrode) and 2) A reusable device that contains a
rechargeable battery, electronic parts, data storage
module, equipment for wireless data transmission,
and a signal processing module (this part is termed
the ePatch sensor). The ePatch sensor is attached
directly on the ePatch electrode. This makes the
system completely free of cables. This is designed so
that patients can perform normal daily activities
during the recording. Furthermore, the ePatch is
easily worn under normal clothing and the cable free
design makes it possible for the patient to easily
change clothes during the recording. This patch
design also facilitates a very small and light weight
construction that minimizes the awareness of the
system while wearing it. The two ECG channels are
measured as bipolar derivations from the multiple
skin contact points, cf. Figure 3.
Figure 3: Illustration of the ePatch electrode and sensor
before assembly. The ePatch version applied in this study
records two ECG channels using bipolar derivations from
the multiple skin contact points in the ePatch electrode.
The placement of the ePatch electrode results in
a shorter distance between the bipolar recording
electrodes. This might influence the quality of the
ECG signal. This reservation toward the quality of
ECG signals recorded using patch technologies with
near-field recording electrodes was also stated by
Mittal et al., (2011). However, Rosenberg et al.,
(2013) compared the ability of a patch type ECG
recorder to recognize episodes of AF with a
traditional 24-hours HOLTER recording. They
found an excellent agreement between the patch
recorder and the HOLTER recorder for both AF
episode detection and AF burden estimation during a
24 hour recording in 74 consecutive patients.
The selected electrode placement furthermore
changes the different projections of the cardiac
vector, and hereby changes the appearance of the
ECG slightly. This might induce issues regarding the
medical professional’s ability to recognize different
heart rhythms and hereby reduce the practicability of
the system. On the other hand, the advantages of this
placement are expected to include the benefits of
reduced artefacts from large muscles and large
movements of electrodes and wires. Furthermore,
several studies have shown promising results with
experimental ECG recorders placed at a midsternal
location. Two research groups, (Janata et al., 2008)
and (Lemmert et al., 2011), conducted studies where
7 seconds noise free HOLTER recordings were
visually compared with 7 seconds noise free ECG
recordings from a prototype device developed by
Phillips Healthcare. Janata et al., (2008) investigated
different placements of the experimental device and
compared the ability to recognize the presence of P
waves, PR time, ventricular morphology (QRS
width ≤ 0.12 seconds or prolonged), and rhythm
diagnosis. They found that for the presence of P
waves, PR time and general rhythm diagnosis, the
device location had a significant influence, and that
a midtsternal location was optimal. They generally
obtain a good agreement between the two devices.
Lemmert et al., (2011) investigated the ability to
visually recognize ventricular ectopic beats (VEBs)
and ventricular fibrillation (VF) with ECGs recorded
with the prototype device and EASI lead. The
authors found a very high accuracy between the two
devices for recognition of VEBs and VEB
configuration counts. The results furthermore
showed a perfect agreement between the two devices
for the recognition of VF. The recognition of pace
spikes was better on the standard device.
Furthermore, studies conducted by Puurtinen et al.,
(2009), indicate that, with respect to P-wave
amplitude, the optimal placement of closely spaced
HeartRhythmAnalysisusingECGRecordedwithaNovelSternumbasedPatchTechnology-APilotStudy
17
bipolar electrodes is diagonally above the standard
12-lead precordial leads V1 and V2.
A review of the literature thus indicates a strong
potential for the recording of relevant ECG signals
on the sternum. However, the described systems are
not completely comparable to the ePatch system and
it is therefore desirable to investigate the practical
usefulness of two ECG channels recorded with the
novel ePatch technology placed at the sternum. This
investigation is thus the focus of this clinical pilot
study. During the study, the analysis of the recorded
ECG signals is performed in a setting fairly similar
to the setting for the traditional HOLTER or
telemetry recordings.
2 METHODS AND DESIGN
This study includes ECG data segments from 25
different hospitalized patients. The choice of
hospitalized patients ensures a realistic amount of
abnormal beat morphologies and abnormal heart
rhythms. Each of the patients was monitored with an
ePatch for approximately 24 hours. All patients were
simultaneously monitored with the regular telemetry
equipment at the hospital department. The ePatch
ECG signals were recorded using a sampling
frequency of 512 Hz and a resolution of 12 bits. In
compliance with IEC 60601-2-47, the ePatch front
end had an analog bandpass filter between 0.67 and
40 Hz. The study was conducted in accordance with
the principles of Good Clinical Practice (GCP)
(Research Ethics Committee ID: S-20120132). All
patients were informed about the study and signed a
written consent form before their inclusion in the
study. The patients were furthermore questioned
about any discomfort and their general satisfaction
with wearing the system. They were asked regarding
their level of satisfaction on an analog scale from
“very satisfied” to “very dissatisfied”. The study
included 15 males and 10 females. The mean Body
Mass Index (BMI) was 27.5 with a standard
deviation of 6.3. The mean age was 71.7 years with
a standard deviation of 13.0 years.
As mentioned, the purpose of the study was to
investigate whether two channel ECG signals
recorded with the ePatch placed at the sternum is
useful for heart rhythm analysis. In a realistic
setting, a medical technician with speciality in
HOLTER or telemetry analysis extracts relevant
ECG segments that are provided to the referring
medical doctor. This step was also performed in this
study. An experienced nurse was asked to extract 7
seconds ECG segments where the interpretation of
the ECG signal was not hindered by noise, in other
words, the data should be of sufficient signal quality.
The definition of sufficient signal quality was thus
based on a subjective judgement by an experienced
ECG analyzer. This is somehow similar to the
extraction of ECG snippets during a traditional
HOLTER analysis. The ECG segments were
provided to both the nurse and the medical doctors
without any form of digital filtering, that is, the
analysis was based on raw ECG signals. A total of 8
segments were extracted from each patient
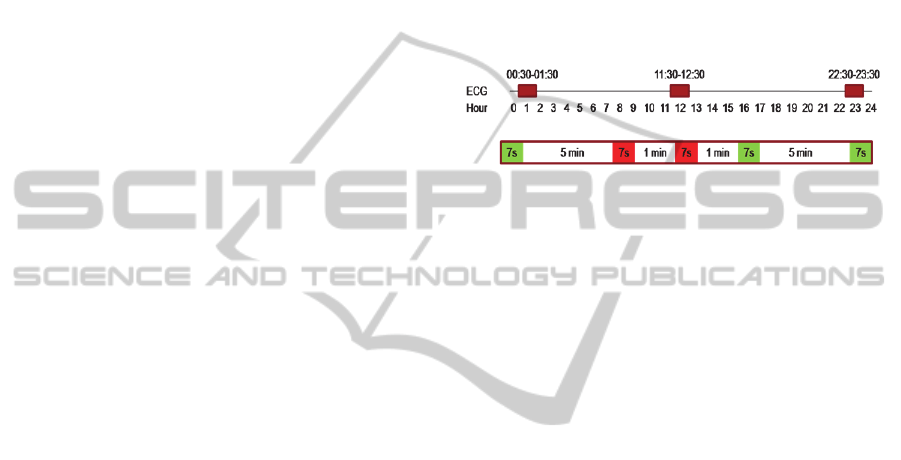
according to the scheme illustrated in Figure 4.
Figure 4: Illustration of the data extraction and selection
process. The red marks on the top panel indicate the three
one hour segments that were extracted for the study for a
recording of exactly 24 hours. The bottom panel illustrates
the process of selection of 7 seconds segments from the
extracted data. Green segments are selected for the study,
whereas red segments are excluded.
For each patient, three hours of data was
considered. The three hours were extracted as 1 hour
in the beginning, 1 hour in the middle, and 1 hour at
the end of the recording. The first and last 30
minutes were, however, not considered to ensure
that artefacts from mounting and removal of
electrodes did not affect the extracted data. The three
hours of extracted data for a recording of exactly 24
hours is illustrated by red colour marks in Figure 4.
This ensures that a patient is only excluded from the
analysis if the general signal quality is insufficient
throughout the recording.
The 7 seconds ECG segments are extracted from
these three hours of data according to the following
scheme: 1) If the current 7 seconds data segment is
considered noise free, it is selected for the study, and
a new 7 seconds segment is investigated 5 minutes
later. 2) If the current 7 seconds data segment is not
considered noise free, it is excluded from the study,
and a new 7 seconds segment is investigated 1
minute later. 3) If it is not possible to extract 8
segments of sufficient signal quality within these
three hours of data, the patient is excluded from the
study.
The data was selected with a custom designed
Graphical User Interface (GUI) using MATLAB
R2012B. The GUI provided an illustration of 7
seconds of two channel ECG data, and the nurse was
asked to use two check boxes to choose between
CARDIOTECHNIX2013-InternationalCongressonCardiovascularTechnologies
18
“noise free segment” and “noise disturbed segment”.
The study included a total of 200 two channel ECG
segments.
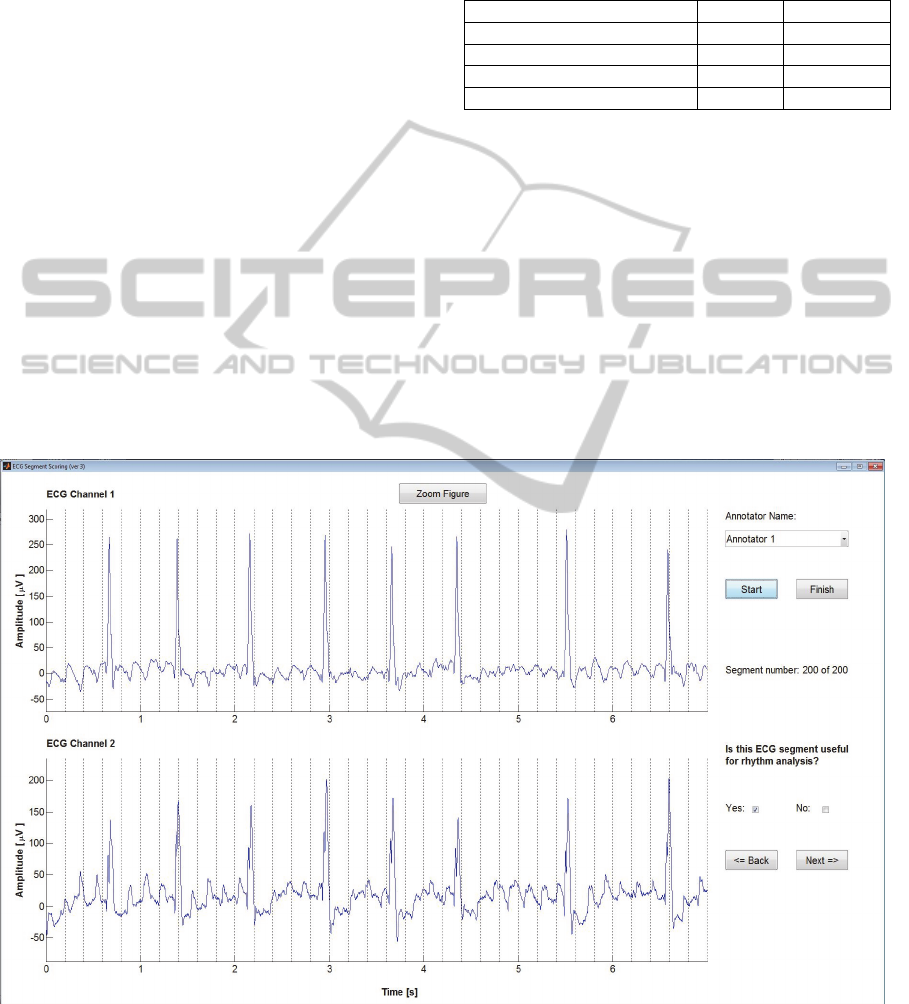
After selection of the 200 ECG segments, two
medical doctors with experience in ECG
interpretation performed an independent individual
evaluation of each of the ECG segments according
to the usefulness for heart rhythm analysis.
The medical evaluation of each segment was
conducted using another GUI designed in MATLAB
R2012B. This GUI is illustrated in Figure 5. The two
channel ECG signal is visualized and the medical
doctor was asked to choose between two check
boxes, indicating the usefulness of the ECG segment
for rhythm analysis.
3 RESULTS
Each ECG segment was evaluated according to the
usefulness for heart rhythm analysis. The score
“good” indicates that the ECG segment was found
useful for heart rhythm analysis, whereas the score
“bad” indicates that the ECG segment was not
considered useful for rhythm analysis. The
evaluation from both medical doctors is illustrated in
Figure 6.
Table 1: Results from the evaluation for ECG segment
relevance for rhythm analysis from the two medical
doctors.
Segments marked as “good” Number Percentage
Medical doctor 1 197 98.5%
Medical doctor 2 199 99.5%
Both medical doctors 196 98%
At least one medical doctor 200 100%
As observed from Figure 6, the doctors did not
agree on the segments that were not useful for
rhythm analysis. This is also illustrated in Table 1
that contains the percentage of “good” ECG
segments for each doctor, the percentage of ECG
segments considered as “good” by both doctors and
the percentage of segments considered as “good” by
at least one of the doctors.
Of the 25 patients, 22 indicated that they were
very satisfied with wearing the device, 1 indicated to
be satisfied, and 2 did not answer the question.
Furthermore, several patients mentioned that they
did not even notice that they were wearing it.
Figure 5: Illustration of the designed GUI used for the medical doctor evaluation of each 7 seconds ECG segment. The two
channel ECG segment was visualized on a computer screen, and the medical doctor was asked to check one of the check
boxes dependent on his evaluation of the relevance of the current ECG segment for rhythm analysis. Note, that this segment
illustrates a case of AF.
HeartRhythmAnalysisusingECGRecordedwithaNovelSternumbasedPatchTechnology-APilotStudy
19
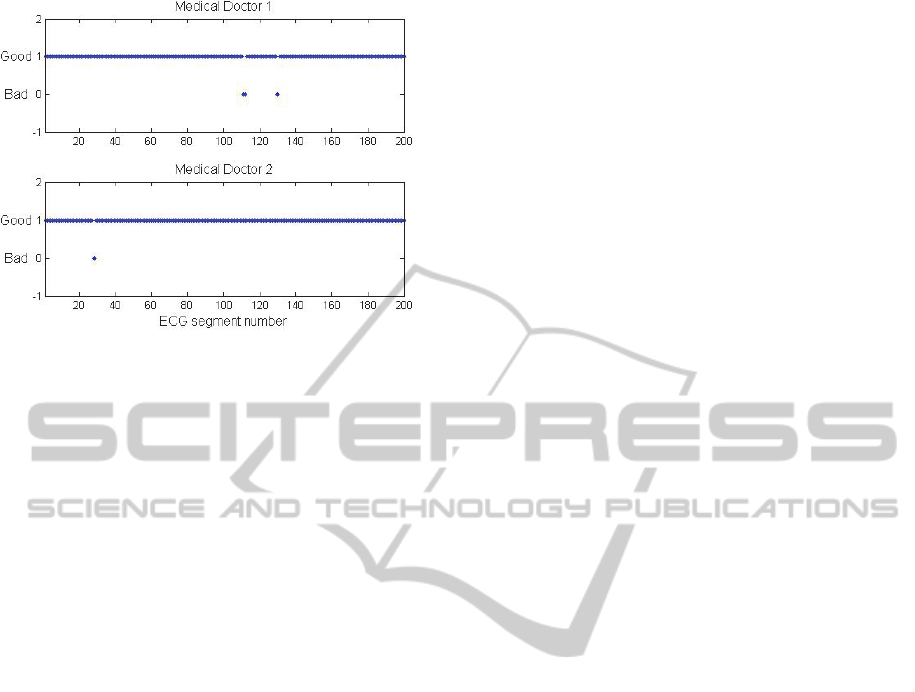
Figure 6: Illustration of the evaluation from both medical
doctors for each of the 200 ECG segments. The score “1”
is “good” and indicates that the ECG segment was
considered useful, whereas the score “0” indicates that the
ECG segment was not considered useful for rhythm
analysis.
4 DISCUSSION
Both medical doctors indicated that more than 98%
of the selected ECG segments were diagnostically
meaningful to them, and that the ECG could help
toward a rhythm analysis and diagnosis of the
patient. It should, of course, be stated that the
diagnosis of the patient would contain results from
other relevant clinical tests, medical history, review
of the entire long-term ECG recording, and general
comments from the nurse preparing the ECG report
for the referring medical doctor. The diagnosis is not
imagined to be based solely on the 7 seconds ECG
segments investigated in this study. However, the
results from this pilot study are very promising and
indicate the potential for this novel device for
ambulatory cardiac monitoring.
The fact that the “bad” segments were not the
same for both medical doctors, could indicate a
certain degree of inter reader variability. The
number of doctors could be increased in a future
study to investigate the true inter reader variability.
For the purpose of this pilot study, it is, however,
considered sufficient with the evaluation by two
medical doctors. It should also be stated that even
using the “worst case” of judging all segments
evaluated as “bad” by at least one of the doctors as a
“bad” segment, still results in 98% of the segments
being useful. Furthermore, a traditional HOLTER
recording might also contain segments of data that is
not useful for rhythm analysis. In a real life
situation, cases of doubt about a diagnosis are solved
by discussion and consensus with other doctors. This
is also expected to be the case when ePatch ECG
signals are applied for rhythm analysis.
Another interesting finding is the generally high
patient satisfaction with wearing the system. This is
one of the expected advantages of this novel
technology. The high patient comfort is expected to
allow very long-term monitoring in the future. This
could increase the likelihood of detecting
paroxysmal and infrequent arrhythmias. The higher
patient comfort is also expected to increase the
compliance with wearing the system, and a high
patient compliance is necessary for reliable
monitoring results (Ackermans, Solosko, Spencer,
Gehman, Nammi, Engel and Russell, 2012).
The focus of this pilot study was to obtain
preliminary knowledge about the overall
applicability of ECG signals recorded with the
ePatch on the sternum. Future studies might include
more direct comparisons between ECG signals
recorded synchronously with the ePatch and
traditional HOLTER recordings. Future studies
might also investigate the ability to correctly detect
specific ECG features, e.g. the presence of the P-
wave.
The future possibilities of this type of long-term
ambulatory ECG recorders seem to be very high in
areas like home monitoring, screenings, and follow-
up consultations. However, the knowledge about the
practical application of these new technologies is
still relatively limited due to the lack of large-scale
applications of the technology in everyday clinical
situations. This study contributes to the currently
limited amount of knowledge about the usability of
these patch type ECG recorders. Further
investigations could be conducted to investigate the
usefulness for specific cardiac conditions on a larger
database. Furthermore, in this study, only noise free
ECG segments were presented to the medical
doctors. This mimics the everyday selection of
representative ECG “snippets” for the referring
medical doctor and serves the purpose of this study.
However, large-scale studies should be conducted to
investigate the general level of artefacts and signal
quality with this new patch technology.
5 CONCLUSIONS
This clinical pilot study indicates the medical
usefulness of two channel ECG signals recorded at
the sternum using the novel ePatch technology for
heart rhythm analysis. Furthermore, the 25 included
patients provided positive declarations regarding
CARDIOTECHNIX2013-InternationalCongressonCardiovascularTechnologies
20

their experience with the device. Further studies
should be conducted to establish possible new
application areas for this new technology and to
determine the general quality of the signal and the
vulnerability to different types of artefacts.
ACKNOWLEDGEMENTS
The clinical study was supported by funding from
the Danish Business Innovation Fund. The authors
wish to thank the clinical staff at the Department of
Medical Research, OUH Svendborg hospital, for
conducting the clinical recordings.
REFERENCES
Ackermans, P. A. J., Solosko, T. A., Spencer, E. C.,
Gehman, S. E., Nammi, K., Engel, J. & Russell, J. K.
(2012). A user-friendly integrated monitor-adhesive
patch for long-term ambulatory electrocardiogram
monitoring. Journal of Electrocardiology, 45(2), 148-
153. doi:10.1016/j.jelectrocard.2011.10.007.
IEC 60601-2-47:2012 Medical electrical equipment – Part
2-47: Particular requirements for the basic safety and
essential performance of ambulatory
electrocardiographic systems.
Janata, A., Lemmert, M. E., Russell, J. K., Gehman, S.,
Fleischhackl, R., Robak, O., Pernicka, E., Sterz, F. &
Gorgels, A. P. M. (2008). Quality of ECG Monitoring
with a Miniature ECG Recorder. Pacing and Clinical
Electrophysiology, 31(6), 676-684. doi:
10.1111/j.1540-8159.2008.01070.x.
Lemmert, M. E., Janata, A., Erkens, P., Russell, J. K.,
Gehman, S., Nammi, K., Crijns, H. J. G. M., Sterz, F.
& Gorgels, A. P. M. (2011). Detection of ventricular
ectopy by a novel miniature electrocardiogram
recorder. Journal of Electrocardiology, 44(2), 222-
228. doi: 10.1016/j.jelectrocard.2010.10.028
Mittal, S., Movsowitz, C. & Steinberg, J. S. (2011).
Ambulatory External Electrocardiographic Monitoring
Focus on Atrial Fibrillation. Journal of American
College of Cardiolog, 58(17), 1741-1749. doi:
10.1016/j.jacc.2011.07.026.
Puurtinen, M., Viik, J. & Hyttinen, J. (2009). Best
Electrode Locations for a Small Bipolar ECG Device:
Signal Strength Analysis on Clinical Data. Annals of
Biomedical Engineering, 37(2), 331-336. doi:
10.1007/s10439-008-9604-y.
Rosenberg, M. A., Samuel, M., Thosani, A. & Zimetbaum,
P. J. (2013). Use of a Noninvasive Continuous
Monitoring Device in the Management of Atrial
Fibrillation: A Pilot Study. Pacing and Clinical
Electrophysiology, 36(3), 328-333. doi:
10.1111/pace.12053.
World Health Organization (March 2013). Cardiovascular
diseases (CVDs). Retrieved June 6, 2013, from
http://www.who.int/mediacentre/factsheets/fs317/en/
Zimetbaum, P. & Goldman, A. (2010). Ambulatory
Arrhythmia Monitoring: Choosing the Right Device.
Circulation, 122(16), 1629-1636. doi:
10.1161/CIRCULATIONAHA.109.925610.
HeartRhythmAnalysisusingECGRecordedwithaNovelSternumbasedPatchTechnology-APilotStudy
21
