
MOVING FROM REMOTE PATIENT MONITORS TO
CLOUD-BASED PERSONAL HEALTH
INFORMATION SYSTEMS
A Way to Practicing Patient-centered Chronic Care Model
Juha Puustjärvi
1
and Leena Puustjärvi
2
1
Department of Computer Science, University of Helsinki, P.O. Box 68, Helsinki, Finland
2
The Pharmacy of Kaivopuisto, Neitsytpolku 10, Helsinki, Finland
Keywords: Remote patient monitoring, Personal health systems, Healthcare models, Cloud computing, Semantic Web,
Ontologies, OWL, RDF.
Abstract: Recent advances in remote patient monitoring allow patient to transmit vital health data from their home to
physicians’ offices and receive health coaching from their healthcare providers based on the clinical data
they have sent. Unfortunately such a remote monitoring technology only provides the connection between
patients and healthcare providers and thus does not support new emerging healthcare models such as
patient-centered care, pharmaceutical care or chronic care models. These healthcare models need
technology solutions that (i) support the co-operation within patient’s healthcare team (i.e., connect patients,
patient’s family members and healthcare professionals), (ii) provide a platform for sharing patient’s
healthcare data among the healthcare team, and (iii) provide a mechanism for disseminating relevant
educational material for the patient and the healthcare team. In this paper, we describe our work on
designing a personal health information system, which supports patient remote monitoring and the new
emerging healthcare models as well. The key idea is to develop the system by integrating relevant e-health
tools through a shared ontology and to exploit the flexibility of cloud computing in its implementation. In
developing the ontology we have used semantic web technologies such as OWL and RDF.
1 INTRODUCTION
The introduction of new emerging healthcare
models, such as patient-centered care,
pharmaceutical care, and chronic care model, are
changing how people think about health and of
patients themselves.
Patient-centered care (Bauman et al., 2003;
Gillespie et al., 2004; Little et al., 2001) emphasizes
the coordination and integration of care, and the use
of appropriate information, communication, and
education technologies in connecting patients,
caregivers, physicians, nurses, and others into a
healthcare team where health system supports and
encourages cooperation among team members. It is
based on the assumption that physicians, patients
and their families have the ability to obtain and
understand health information and services, and
make appropriate health decisions (Michie et al.,
2003). This in turn requires that health information
should be presented according to individuals
understanding and abilities (Stewart, 2004).
Pharmaceutical care emphasizes the movement
of pharmacy practice away from its original role on
drug supply towards a more inclusive focus on
patient care (Wiedenmayer et al., 2006; Mil et al.,
2004; Hepler and Strand, 1990). It emphasizes the
responsible provision of drug therapy for the
purpose of achieving definite outcomes that improve
patient’s quality of life (WHO, 1997; Hepler, 2004).
Chronic care model (Fiandt, 2011; Boult et al,
2008) emphasizes patients’ long-term healthcare
needs as a counterweight to the attention typically
paid to acute short-term, and emergency care. In this
sense, the traditional care models are not appropriate
as the patients with chronic illness do not receive
enough information about their condition, and they
are not supported in caring themselves after they
leave the doctor’s office or hospital.
Patient remote monitoring and home telehealth
technologies provide a variety of tools for patients to
37
Puustjärvi J. and Puustjärvi L..
MOVING FROM REMOTE PATIENT MONITORS TO CLOUD-BASED PERSONAL HEALTH INFORMATION SYSTEMS - A Way to Practicing
Patient-centered Chronic Care Model.
DOI: 10.5220/0003736500370045
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2012), pages 37-45
ISBN: 978-989-8425-88-1
Copyright
c
2012 SCITEPRESS (Science and Technology Publications, Lda.)

take an active role in the management of their
chronic diseases. Especially, the ability to monitor
and interact with patient from a distance by
exploiting electronic devices to record and send the
measurements of patients’ vital signs to a caregiver
has been a key technology in fostering patients’
ability to receive care at home. Earlier the only
reliable means of controlling such measurements has
been for a medical professional to take them
directly, or for a patient to be constantly monitored
in hospital, which would normally only happen once
the patient has become seriously ill.
The new technologies and principle of practicing
medicine holds significant promise of improving on
major health care delivery problems. However, there
are many functions in the patient-centered care,
pharmaceutical care and chronic care models that the
home telehealth devices and the e-heath tools such
as personal health records do not support.
For example, patients that are out of hospital or
who are left hospital often have concerns about their
medicines, and so there is strong demand for
extending the functionalities of home telehealth
devices by the functions of pharmaceutical care.
Neither the current e-heath tools support the
coordination of the care, nor the social connections
among the members of patient’s healthcare team.
They also fail in providing comprehensive access to
patient’s health data and in promoting patient’s
medical education.
Inspired by the (semantic) web technologies and
the flexibility of cloud computing, we have studied
their suitability for supporting the emerging
healthcare models. Our studies have indicated that
Personal Health Information Systems (PHIS) should
support the functionalities of many traditional e-
health tools such as remote patient monitors,
personal health records, health-oriented blogs, and
health-oriented information servers. It is also turned
out that by gathering these functionalities into one
system we can achieve synergy, i.e., achieve
functionalities that would not be obtainable by any
of the e-health tools independently.
In gathering the functionalities we have adapted
the ideas of knowledge centric organizations to
PHIS, i.e., we have revolved the e-health tools
around a health oriented knowledge base. So, all the
e-heath tools share patient’s health data. Further by
exploiting the characteristics provided by cloud
computing we can easily ensure the interoperation of
patient’s healthcare team: accessing the PHIS
requires only internet connection. Instead of the
prevailing systems provided by healthcare
organizations do not provide appropriate technology
for co-operation as their use is devoted to
organization’s healthcare personnel only.
The rest of the paper is organized as follows.
First, in Section 2, we motivate our work by
considering the recent advances in patient remote
monitoring. Then, in Section 3, we present the
requirements of PHIS that we have derived from
emerging healthcare models, and then, in Section 4,
we analyze the suitability of cloud computing for
satisfying these requirements. In Section 5, we
present the architecture of the knowledge oriented
PHIS and the PHIS-ontology that is shared by the e-
health tools. In Section 6 we describe how the PHIS-
ontology can be exploited in promoting patient’s
medical education and in delivering relevant
information within patient’s healthcare team. In
Section 7, we illustrate how XSLT-transformations
is used in transforming XML-coded medical data in
the format that is compliant with the PHIS-ontology.
Finally Section 8 concludes the paper by discussing
the challenges of our solutions as well as our future
research.
2 REMOTE PATIENT
MONITORING
Telemedicine is the use of medical information
exchanged from one site to another via
communications to improve a patient's health
(Angaran, 1999; Kontaxakis et al., 1990).
Telemedicine is viewed as a cost-effective
alternative to the more traditional face-to-face way
of providing medical care (Kontaxakis, 2006).
Telemedicine can be broken into three main
categories: store-and-forward, interactive services
and remote patient monitoring.
• Store-and-forward telemedicine involves
acquiring medical data and then transmitting
this data to the system that is accessible to
patient’s physician. So it does not require the
presence of patient and physician at the same
time.
• Interactive services provide real-time
interactions between patient and physician. It
includes phone conversations, online
communication and home visits.
• Remote monitoring enables medical
professionals to monitor a patient remotely
using various technological devices. Remote
monitoring is above all used for managing
chronic diseases such as heart disease, diabetes
and asthma.
HEALTHINF 2012 - International Conference on Health Informatics
38
Nowadays remote patient monitoring
technologies are becoming a more sophisticated,
integrated, and systematic approach to healthcare
that can be personalized to each patient’s medical
needs. In particular, Personal Health Systems
(PHSs) go beyond the simple remote patient
monitoring systems in that they enable the
communication between patients and healthcare
professionals and provide clinicians with access to
current patient data. They also provide interactive
tools for personalized care management including
vital sign collection, patient reminders and
communication tools such as video conferencing
capabilities, allowing remotely located health care
professionals to interview, observe and educate the
patient, as well as assist in the use of the peripherals
or other medical devices. Some devices also have
the ability to show video, which can be used for
educating the patient.
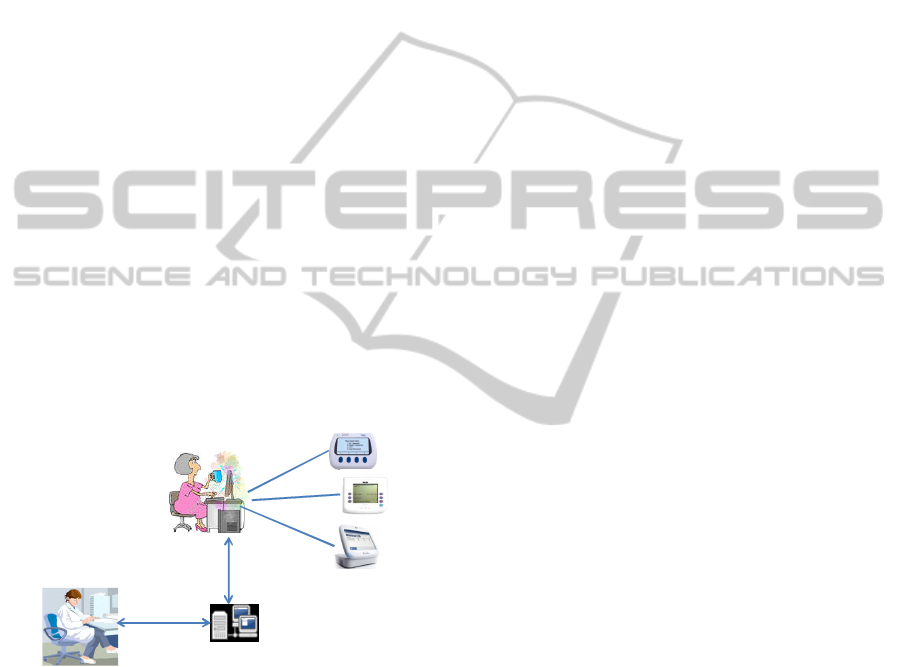
From technology point of view personal health
systems consist of a hub and wireless peripheral
devices that collects physiologic data. Typical
peripheral devices include blood pressure cuffs,
pulse oximeters, weight scales blood glucose meter.
The data gathered from peripheral devices are
transmitted by the hub to a clinical database for later
analysis (Figure 1).
Ahubdeviceat
patient’shome
Healthcareprovider
(physician,nurse,pharmacist).
Clinical
information
database
Peripheraldevices
Figure 1: Remote monitoring through a clinical
information database.
3 INFORMATION
FLOWS IN PHIS
The technology that supports both patient centered
healthcare and pharmaceutical care of the patients
with chronic conditions have to coordinate the flows
of information that are coming from a variety of
sources. These information flows include:
• Vital sign information from peripheral devices
(that collect physiologic data) to PHIS.
• Health regimen information between healthcare
providers (physicians, nurses and pharmacists).
• Information between patient and healthcare
providers.
• Healthcare information between healthcare
providers and patient’s family members.
• Relevant educational health information from
healthcare providers to patient.
Supporting these information flows is much
more challenging as the simple vital sign
information flow that characterized an earlier
generation of remote patient monitoring. In
particular the traditional remote monitoring model
(illustrated in Figure 1) supports only partially these
requirements as the usage of the clinical information
system is isolated from third parties such as from
patient’s family members.
Apart from the co-operation support, the
member’s of patient’s healthcare team should have a
seamless access to patient’s health data, which is
usually stored in electronic health record (EHR)
(EHR, 2011) or personal health records (PHR)
(Raisinghani and Young, 2008). The former is
managed by medical authorities while the latter
managed by the patient and all that are authorized by
the patient are allowed to access it (Puustjärvi and
Puustjärvi, 2011). Hence patient’s PHR, which in
our architecture is a component of the PHIS, has a
central role to support emerging healthcare models.
4 CLOUD-BASED PHIS
Cloud computing is a technology that uses the
Internet and central remote servers to maintain data
and applications (Chappel, 2011). It is an evaluation
of the widespread adoption of virtualization, service
oriented architecture and utility computing
(Wikipedia, 2011). The name cloud computing was
originally inspired by the cloud symbol that's often
used to represent the internet in diagrams.
Cloud computing allows consumers and
businesses to use applications without installation,
and they can access their personal files at any
computer with internet access. This technology
allows for more efficient computing by centralizing
storage, memory, processing and bandwidth.
Further, unlike traditional hosting it provides the
following useful characteristics:
• The resources of the cloud can be used on
demand, typically by the minutes.
MOVING FROM REMOTE PATIENT MONITORS TO CLOUD-BASED PERSONAL HEALTH INFORMATION
SYSTEMS - A Way to Practicing Patient-centered Chronic Care Model
39

• The used resources are easily scalable in the
sense that users can have as much or as little of
a service as they want at any given time.
• The resources are fully managed by the
provider. The consumer does not need any
complex resource, only a personal computer
with internet access.
Software as a service (SaaS), is a type of cloud
computing. In this service model, a service provider
licenses an application to customers either as a
service on demand, through a subscription, in a
"pay-as-you-go" model, or at no charge (Khajeh-
Hosseini, 2011). The SaaS model to application
delivery is part of the utility computing model where
all of the technology is in the "cloud" accessed over
the internet as a service.
There are various architectural ways for
implementing the SaaS model including the
followings (Chappel, 2011):
• Each customer has a customized version of the
hosted application that runs as its own instance
on the host's servers.
• Many customers use separate instances of the
same application code.
• A single program instance serves all customers.
In the case of PHISs the required computation is
rather small compared to traditional business
applications and thus the last mentioned architecture
is appropriate for the implementation of the PHIS,
i.e., a single PHIS serves all patients. However,
patient specific data can only be accessed by the
patient and those that are authorized by the patient.
The SaaS-based PHIS and its users are presented in
Figure 2.
PHIS‐server
PatientathomePatientawayfromhome
Healthcareprovider
(p
h
y
sician
,
nurse
,
p
harmacist
)
.
Patient’sfamilymembers
Thecloud
Aserverin
thecloud
Aserverin
thecloud
Aserverin
thecloud
Peripheraldevices
Figure 2: The users of the cloud-based PHIS.
We next itemize some clarifying aspects of the
figure:
• The cloud takes the advantages of SOA
(Service Oriented Architecture) in the
interoperation of the services, e.g., in importing
patient’s health data the PHIS-server
interoperates with the servers of other
healthcare organizations including hospitals,
physicians’ offices and health centers.
• As the figure illustrates the peripheral devices
that the patient has at home are connected to
patient’s PC, and so the vital signs collected by
the devices are transmitted via the PC to the
cloud, i.e., to the PHIS.
• The patient accesses his or her health data
stored in PHIS through the browser. As the
patient needs nothing but an internet access, the
patient can easily connect to the PHIS at home,
as well as being away from home.
• Healthcare providers and patient’s family
members that are authorized by the patient can
access patient’s health data as well as
communicate through their browsers.
Next, we consider the internal structure of the PHIS-
server.
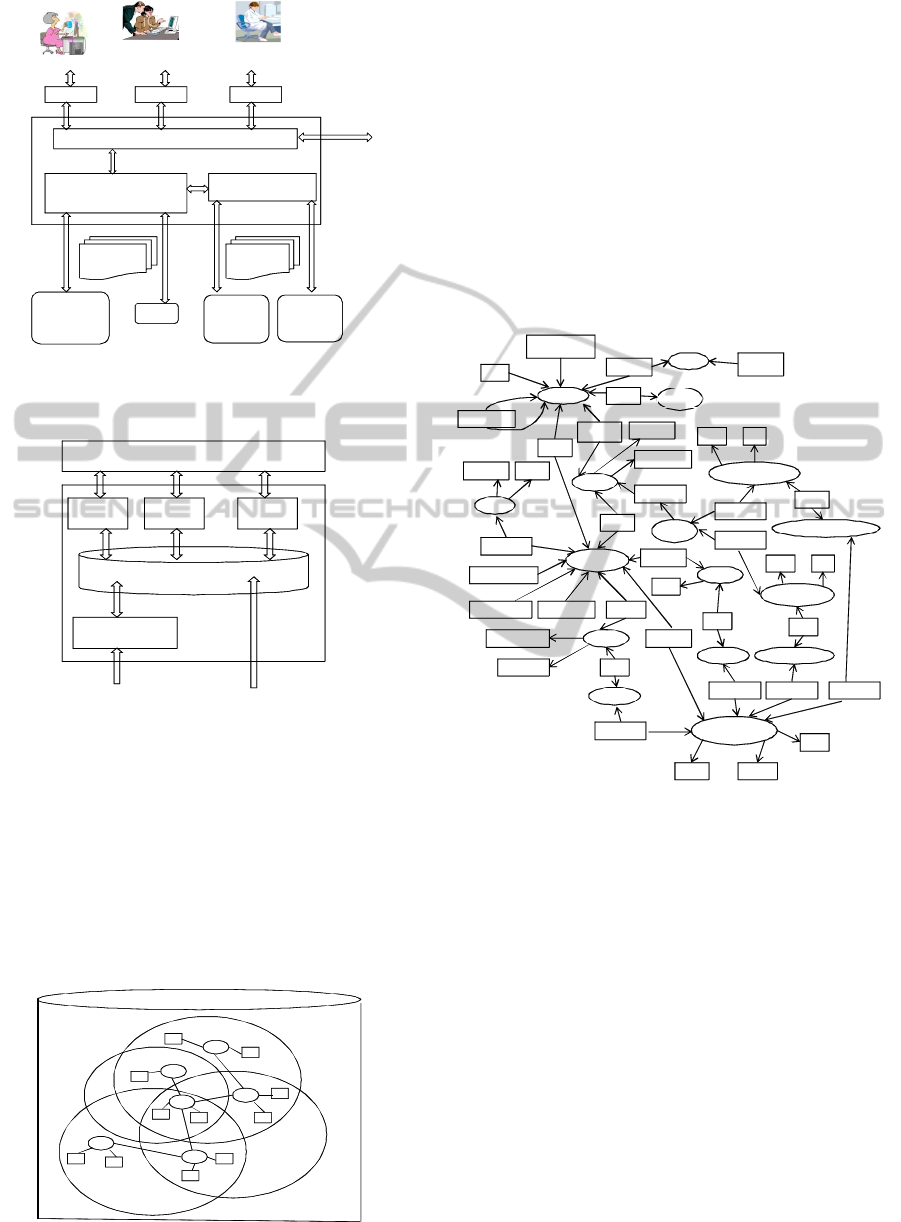
5 PHIS-ONTOLOGY
The architecture of the PHIS and its connections in
the cloud are presented in Figure 3. As the figure
illustrates patient and the members of his or her
healthcare team access the PHIS-server through the
personalized health portal. It is a site on WWW that
provides personalized capabilities for its users and
links to other relevant servers.
In designing the PHIS we have followed the
idea of knowledge oriented organizations (Daconta
et al., 2003), where the key idea is to revolve all
applications around a shared ontology (stored in a
knowledge base), which we call PHIS-ontology. It is
developed by integrating the ontologies of the e-
health tools supported by the PHIS. For now we
have integrated the ontologies of the Blog manager,
Information therapy (Ix) manager, Remote manager,
and PHR manager. Such an internal architecture of
the PHIS is presented in Figure 4.
HEALTHINF 2012 - International Conference on Health Informatics
40
XSLT-
transformationPHIS
Gym
Health data
from patient’s
peripheral
devices
Non-healthcare organizations
Hospital
Information
system
Physician
office
system
Healthcare organizations
CDA-
documents
RDF-coded
documents
Patient
Patient’s
authorized users
Healthcare
providers
Browser
BrowserBrowser
…
Personalized health portal
PHIS- server
Links to
other
servers
Figure 3: The component of the PHIS-server and its
external connections.
PHIS‐ontology
Blog
manager
Ix
manager
PHR
manager
.. .
PersonalHealthPortal
PHIS
RDF‐ codeddata
Remotepatient
controller
RDF‐ codeddocuments
Figure 4: The e-heath tools accessing the PHIS-ontology.
Figure 5 illustrates the idea of the knowledge
base and the case where PHIS-ontology is developed
by integrating the Blog-ontology, Ix-ontology, PHR-
ontology and RM-ontology (Remote Monitoring
ontology). In the figure ellipses represent OWL´s
classes, rectangles represent OWL’s data properties
and the lines between ellipses represent OWL’s
object properties. Accordingly class A is shared by
all the four ontologies.
d2
C
D
B
E
A
a2
c1
c2
e2
e1d1
b2
b1
a1
Knowledgebase
E
e1
PHR‐ ontology
Blog‐ ontology
RM‐ ontology
Ix‐ ontology
Figure 5: PHIS-ontology.
In order to illustrate shared classes, A could be
class Disease, B class Patient, and C class
Informal_entity. Further assume that object property
A-B is suffer_from, object property A-E is deals,
data property b1 is patient_name, and data property
e1 is a url. In such as setting we could specify by
RDF (Resource Description Framework) that John
Smith suffers from diabetes and the educational
material dealing diabetes is stored in a specific url.
A portion of the PHIS-ontology is graphically
presented in Figure 6. In this graphical
representation ellipses represent classes and
subclasses, and rectangles represent data and object
properties.
Patient
Medication
LabTest
BloodPressureTest
ProductProductName
BrandName
StrenghtUnit
Source
ActorIDActorRole
ColesterolTest
Value Unit
Value Unit
Patie ntId
PatientName
SubclassOf
SubclassOf
Uses
Performed
ContainsStrenghtValue
Originates
MedicationId
InformationEntity
SubclassOfSubclassOf SubclassOf
Disease
Name
RelatesTo
DiseaseIE
Deals
SubclassOf
ProductIE
Deals
ColesterolTestIE
Deals
BloodPressureTestIE
Deals
Date Source
URL
Author
Predecessor
Deals Subject
Blog BlogName
Includes
BlogItem
Relates
InsertionDate
Associates
URL
Figure 6: A portion of the PHIS-ontology.
A portion of the graphical ontology of Figure 6 is
presented in OWL in Figure 7.
In order to understand the relationship of XML,
OWL and RDF note that XML (Extensible Mark-up
Language) (Harold and Scott, 2002) is just a meta
language for defining markup languages. By a meta
language we refer to a language used to make
statements about statements in another language,
which is called the object language. Accordingly
RDF (RDF, 2011) and OWL (OWL, 2011) are
object languages. Instead, XML says nothing about
the semantics of the used tags. It just provides a
means for structuring documents. Due to the lack of
semantics we do not use XML for representing
PHIS-ontology but instead we use ontology
languages RDF and OWL.
MOVING FROM REMOTE PATIENT MONITORS TO CLOUD-BASED PERSONAL HEALTH INFORMATION
SYSTEMS - A Way to Practicing Patient-centered Chronic Care Model
41
<rdf:RDF
xmlns:rdf=http://www.w3.org/1999/02/22-rdf-syntax-nsl#
xmln s:rdfs=http://www.w3.org/2000/01/rdf-schema#
xmln s:owl=http://www.w3.org/2002/07/owl#>
<owl:Ontology rd f:about=“”PHA/>
<owl:Class rdf:ID=“Blog/”>
<owl:Class rdf:ID=“BlogItem/”>
<owl:Class rdf:ID=“Patient/”>
<owl:Class rdf:ID=“Medication/”>
<owl:Class rdf:ID=“Source/”>
<owl:Class rdf:ID=“Product/”>
<owl:Class rdf:ID=“LabTest/”>
<owl:Class rdf:ID=“BloodPressureTest”>
<rdfs:subClassOf rdf:resource=“#LabTest”/>
</o wl:Class>
<owl:Class rdf:ID=“ColesterolTest”>
<rdfs:subClassOf rdf:resource=“#LabTest”/>
</o wl:Class>
<owl:ObjectProperty rdf:ID=“Relates”>
<rd fs:d omain rd f:resource=“#BlogItem”/>
<rdfs:range rdf:resource=“#Medication”/>
</owl:ObjectProperty>
<owl:ObjectProperty rdf:ID=“Uses”>
<rdfs:domain rdf:resource=“#Patient”/>
<rdfs:range rdf:resource=“#Medication”/>
</owl:ObjectProperty>
.
.
.
<
/
rdf:RDF
>
Figure 7: A portion of the PHIS-ontology in OWL.
6 PROVIDING INFORMATION
FLOWS AND MEDICAL
EDUCATION
As we have already stated the technology that
supports emerging healthcare models should
coordinate the flows of information within patient’s
healthcare team as well as provide educational
relevant material. In our developed solutions these
functionalities are carried out by the information
stored in the PHIS –ontology. In particular these
functionalities exploit the instances of the classes
BlogItem and InformationEntity.
Each instance of the class BlogItem represents an
entry in patient blog. By its object property
Predecessor the entries are presented in
chronological order with the latest entry listed first,
and by using the object property Deals blog’s entries
can be classified into different subjects. Patient and
patient’s healthcare team are allowed to access and
create new entries for the blog through the
functionalities provided by the Blog manager.
Each instance of the class InformationEntity
represents an educational material. Its data property
url specifies the location of the actual content of the
material, i.e., the instance. As illustrated in Figure 6,
the PHIS-ontology also specifies the relationships of
the class InformationEntity to other relevant classes
such as Medication and Disease. Thus, based on
these relationships relevant educational material can
be automatically delivered to the patient. For
example, we can query the information entities that
deal the diseases that patient John Smith suffers
from. Further, by activating such queries (by the Ix-
manager) when new disease is inserted for a patient,
we can automate information therapy, i.e., prescribe
the right information to right patient at right time.
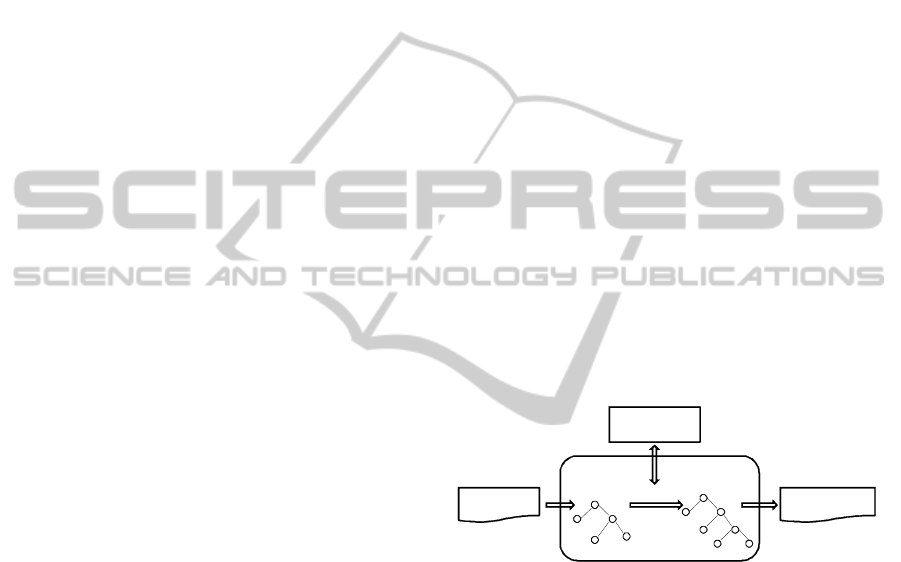
7 TRANSFORMING XML-CODED
DOCUMENTS
As we have already illustrated in Figure 3, the PHIS-
server does not only import data from patients home
telehealth devices but it also imports data from other
information sources such as a hospital laboratory,
gym and physician office.
If the format of the imported data does not
coincide with the PHIS-ontology, then the stylesheet
engine (Daconta, et al., 2003) is required for
transforming the imported data before its insertion
into the PHIS-ontology. Such a transformation is
illustrated in Figure 8.
XML tree
Transformed
XML/RDF tree
Stylesheet Engine
Transformation
Semantic document
in RDF/XML
Stylesheet
(XSLT document)
CDA –document
In XML
Figure 8: Transforming CDA-documents into semantic
documents.
CDA-documents are typical XML-based
documents, and so they are not compliant with the
PHIS-ontology. By the CDA-documents we refer to
documents that are based on the Clinical Document
Architecture (CDA), which is an ANSI approved
HL7 standard (Dolin et al., 2001). It is proven to be
a valuable and powerful standard for a structured
exchange of persistent clinical documents between
different software systems (Puustjärvi and
Puustjärvi, 2009).
However, in the case of non persistent
documents with CDA we encounter many problems.
The main reason for this is that the semantics of the
CDA-documents is bound to the shared HL7
Reference Information Model (RIM) (Dolin et al.,
2001). Thereby introducing new document types
HEALTHINF 2012 - International Conference on Health Informatics
42

would require to extending the RIM, which is a long
lasting standardization process. So this approach
contradicts with our requirement of flexibility in
introducing new document types in importing health
information into the PHIS-ontology. Therefore in
importing data from XML-based data sources (e.g.,
from HL7 CDA compliant systems) requires that the
XML-formatted data is first translated (by an XSLT-
based style sheet engine (Harold and Scott, 2002)
into RDF and then inserted into the PHIS-ontology.
In order to illustrate this transformation consider
the CDA document of Figure 9.
<ContinityOfCareRecord>
<Pat ient>
<ActorID>AB -12345></ActorID>
<ActorName> Susan Taylor</ActorName>
</Patient>
<M edications>
<M edicat ion>
<Source>
<ActorID>Pharmacy of Kaivop uisto</ActorID>
<ActorRole>Pharmacy</ActorRole>
</Source>
<Description>
<Text>One tablet ones a day</Text>
<GenericSubstitutionInfo >
http://www.../medicalinfo/SubstitutionInfo
</ GenericSubst itution Info>
</Descrip tion>
<Product>
<Produ ctName>Valsartan</ProductName>
<ProductInfo>
http://www.../medicalinfo/Valsartan Info
</ProductInfo>
</Product>
<Strenght >
<Value>50</Value>
<Un it>m illigram</ Uni t>
</Stren gh t>
<Quantity>
<Value>30</Value><Unit>Tabs</Unit>
</Quantity>
</Medication>
</Medi cations>
</ContinityOfC areRecord>
Figure 9: A CCR document.
Figure 9 represents a CCR file that has a
medication list (element Medications), which is
comprised of one medication (element Medication)
that is source stamped by the Pharmacy of
Kaivopuisto. The CCR file is based on the CCR
standard (CCR, 2011).
The CCR standard as well as the CCD standard
(HL7, 2011) are originally a patient health summary
standards, and later on these standards are
commonly exploited in structuring the data in
personal health records. From technology point of
view these standards represent two different XML
schemas designed to store patient clinical summaries
(Puustjärvi and Puustjärvi 2009). However, both
schemas are identical in their scope in the sense that
they contain the same data elements.
After the XSLT transformation the CCR
document of Figure 9 is in the RDF/XML format
presented in Figure 10. In this format the document
is compliant with PHIS-ontology and can be inserted
into the PHIS-ontology.
<rdf:RDF
xmlns : rdf=h ttp://www.w3. org/1999/02/22-rdf-s yntax-ns#
xmln s : po=htt p://www.l ut.fi/ontologi es/PHIS-ont ology#>
<rdf:Description rdf:about=”AB-12345”>
<rdf:type rdf:resource=“&po;Patient”/ >
<po : PatientName>Susan Taylor</po:PatientName>
<po:Uses rdf:resource=“&po;Med-07092010”/>
</rdf : Description >
<rdf:Description rdf:about =” Med-07092010”>
<rdf:type rdf:resource=“&po;Medication”/>
<p o:Contains rdf:resource=“&po;Valsartan”/>
<po : Stren gh tValue rdf:datatype=
”&xsd;integer”>30</po : StrenghtValue>
<po : StrenghtUnit>Tabs</po : StrenghtUnit>
</rdf : Description>
<rdf:Description rdf:about=” Valsartan”>
<rdf:type rdf:resource=“&po;Product”/>
<po:Deals rdf:resource=“&info;ValsartanInfo”/>
</rdf : Description>
< rdf:Description rdf:about=” Pharmacy of Kaivopuisto”>
<rdf:type rdf:resource=“&po;Source/>
<p o : ActorRole >P harma cy< /po : Act orR ole>
</rdf : Description>
</rdf:RDF>
Figure 10: Transformed CDA document in RDF/XML
format.
The RDF/XML-formatted document of Figure
10 is comprised of four RDF-descriptions. Further,
the first RDF-description is comprised of three RDF-
statements. The first statement states that the type of
the instance identified by “AB-12345” is Patient in
the PHIS-ontology. The second RDF-statement
states that the name of the instance identified by
“AB-12345” is Susan Taylor.
8 CONCLUSIONS
Monitoring a patient’s vital signs provides an
important source of information to the physician that
treats the patient. Nowadays information and
communication technology provides the possibility
of a new generation of lightweight monitoring
systems which a patient can wear while being at
home or while going about their daily business.
Formerly the only reliable means of such monitoring
has been for a medical professional to take them
directly, or for a patient to be constantly monitored
in hospital.
The new patient remote monitoring technology
MOVING FROM REMOTE PATIENT MONITORS TO CLOUD-BASED PERSONAL HEALTH INFORMATION
SYSTEMS - A Way to Practicing Patient-centered Chronic Care Model
43

holds significant promise of improving on major
health care delivery problems. However, there are
many functions in the emerging healthcare models
(including patient centered care, pharmaceutical care
and chronic care models) that the modern
monitoring devices and systems do not support as
they only provide the communication between
patient and healthcare provider. Instead the
emerging healthcare models require Information and
Communication Technology (ICT) support for the
co-operation of patient’s healthcare team and the
support in delivering relevant educational material
for the patient and the members of the healthcare
team.
Our studies have shown that the ICT-support of
these requirements requires the integration of
patient’s e-health tools as it significantly simplifies
patients’ interaction with the services, enables the
co-operation within the healthcare team and the
development of new services such as automated
information therapy.
From technology point of view we have
integrated e-heath tools through the shared PHIS-
ontology that is stored in the knowledge base, which
exploits semantic web technologies such as OWL
and RDF. The management of the shared ontology
requires that in importing data the documents that
are not compliant with the ontology have to be
transformed by XSLT transformation into the RDF-
format that is compliant with the ontology, i.e., a
stylesheet has to be defined for each non-compliant
document type.
In our future work we will study the effects of
introducing cloud-based health information systems
on the mind-set of patient and healthcare personnel
as the introduction of these technologies also
changes the daily duties of the patient and many
healthcare employees. Therefore we assume the
most challenging aspect will not be the technology
but rather the changing the mind-set of patient’s
healthcare team.
REFERENCES
Angaran, D. M., 1999. Telemedicine and Telepharmacy:
current status and future implications. American
Journal of Health System Pharmacy. Jul 15; Vol. 56:
1405-26
Bauman, A., Fardy, H., Harris, H., 2003. Getting it right;
why bother with patient centred care? Medical Journal
of Australia, 179(5), pp. 253-256.
Blyth, J., 1990. Telecommunications, Concepts,
Development, and Management. Second Edition,
Glencoe/McCgraw-Hill Company, pp.280-282.
Boult, C., Karm, L., Groves, C., 2008. Improving Chronic
Care: The “Guided Care” Model. Available at:
http://www.guidedcare.org/pdf/Guided%20Care%20m
odel_Permanente%20Journal_Winter%202008.pdf
CCR, 2011. Continuity of Care Record (CCR) Standard.
Available at: http://www.ccrstandard.com/
Chappel, 2011. A Short Introduction to Cloud
Computing: An Enterprise-OrientedView. Available
at: http://digitalebookden.com/a-short-introduction-to-
cloud-platforms.html
Daconta, M., Obrst, L., Smith, K., 2003. The semantic
web: A Guide to the Future of XML, Web Services,
and Knowledge Management, John Wiley & Sons.
Dolin, R., Alschuler, L., Beerb, C., Biron, P., Boyer, S.,
Essin, E., Kimber, T. 2001. Lincoln, and J.E.
Mattison. The HL7 Clinical Document Architecture. J.
Am Med Inform Assoc, 2001:8(6), pp. 552-569.
EHR, 2011. Electronic Health Record, Available at:
http://en.wikipedia.org/wiki/Electronic_health_record
Fiandt, K., 2011.. The Chronic Care Model: Description
and Application for Practice. Available at:
http://www.medscape.com/viewarticle/549040
Gillespie, R., Florin, D., Gillam, S., 2004. How is patient-
centred care understood by the clinical, managerial
and lay stakeholders responsible for promoting this
agenda? Health Expectations, vol. 7, No 2, pp. 142-
148.
Harold, E., Scott Means, W., 2002. XML in a Nutshell.
O’Reilly & Associates.
Hepler, C. D., 2004. Clinical pharmacy, pharmaceutical
care, and the quality of drug therapy.
Pharmacotherapy. 24(11):1491–98.
Hepler C. D., Strand L. M., 1990. Opportunities and
responsibilities in pharmaceutical care. Am J Hosp
Pharm; 47:533–43.
HL7, 2007. What is the HL7 Continuity of Care
Document? Available at: http://www.neotool.com/
blog/2007/02/15/what-is-hl7-continuity-of-care-
document/
Little, P., Everitt, H., Williamson, I., 2001. Observational
study of effect of patient centredness and positive
approach on outcomes of general practice
consultations. British Medical Journal, pp. 908-911.
Khajeh-Hosseini, A., Sommerville, I., Sriram, I., 2011.
Research Challenges for Enterprise Cloud Computing.
Available at: http://arxiv.org/ftp/arxiv/papers/1001/
1001.3257.pdf.
Kontaxakis, G., Visvikis, D., Ohl, R., Sachpazidis, I.,
Suarez, J., Selby, B., Peter; et al., 2006. Integrated
telemedicine applications and services for oncological
positron emission tomography - Oncology Reports,
Vol.15: 1091–1100.
Michie, S., Miles, J., Weinman, J., 2003. Patient-
centredness in chronic illness: what is it and does it
matter? Patient Education and Counselling, pp. 197-
206.
Mil. I., Schulz, J., Tromp M., 2004. Pharmaceutical care,
European developments in concepts, implementation,
teaching, and research: a review. Pharm World Sci.
Dec; 26(6):303–11.
HEALTHINF 2012 - International Conference on Health Informatics
44

OWL, 2011. WEB OntologyLanguage. Available at:
http://www.w3.org/TR/owl-features/
Puustjärvi, J., Puustjärvi, L., 2009.. The role of medicinal
ontologies in querying and exchanging pharmaceutical
information. International Journal of Electronic
Healthcare, Vol. 5, No.1 pp. 1 – 13.
Puustjärvi, J., Puustjärvi, L., 2010. Automating the
Importation of Medication Data into Personal Health
Records. In the proc. of the International Conference
on Health Informatics (HEALTHINF 2010). Pages
135-141.
Puustjärvi, J., Puustjärvi, L., 2011. Designing and
Implementing an Active Personal Health Record
System. In the Proc. of the International Conference
on eHealth, Telemedicine, and Social Medicine
(eTELEMED2011).
Raisinghani M. S., Young, E., 2008. Personal health
records: key adoption issues and implications for
management, International Journal of Electronic
Healthcare. Vol. 4, No.1 pp.67-77. 2008.
RDF, 2011. Resource Description Language. Available at:
http://www.w3.org/RDF/
Stewart, M., 2004. Towards a global definition of patient
centred care: The patient should be the judge of patient
centred care. British Medical Journal, 322, pp. 444-
445.
WHO, 1997. The role of the pharmacist in the health care
system. Preparing the future pharmacist: Curricular
development. Report of a third WHO Consultative
Group on the role of the pharmacist, Vancouver,
Canada, 27–29. Geneva: World Health Organization.
WHO/PHARM/97/599. Available at: http://www.
who.int/medicinedocs/
Wiedenmayer, K., Summers, R., Mackie, C., Gous, A.,
Everard, M., Tromp, D., 2006. Developing pharmacy
practice. World Health Organization and International
Pharmaceutical Federation.
Wiki, 2011, Cloud Computing. Available at:
http://en.wikipedia.org/wiki/Cloud_computing
MOVING FROM REMOTE PATIENT MONITORS TO CLOUD-BASED PERSONAL HEALTH INFORMATION
SYSTEMS - A Way to Practicing Patient-centered Chronic Care Model
45
