
Translingual Neurostimulation in Treatment of Children with
Cerebral Palsy in the Late Residual Stage. Case Study
T. S. Ignatova
1
, V. E. Kolbin
1
, A. M. Sarana
1,2
, S. G. Scherbak
1,2
, Yu. P. Danilov
3
,
N. N. Semibratov
4
, A. V. Sokolov
4
, G. E. Trufanov
4
, A. V. Ryzhkov
4
and A. Yu. Efimtsev
4
1
State Health Institution «City Hospital №40», Neurology and Rehabilitation Department, Saint-Petersburg, Russia
2
State University, Faculty of Medicine, Saint-Petersburg, Russia
3
TCNL, Kinesiology Department, Wisconsin, U.S.A.
4
National Medical Research Centre n.a. V.A.Almazov, SIL MRI, Saint-Petersburg, Russia
Keywords: Translingual Neurostimulation, Portable Neurostimulator, Rehabilitation, Cerebral Palsy, fMRI,
Neuroimaging.
Abstract: Management of cerebral palsy is an actual problem of modern medicine. A new direction of
neurorehabilitation, intensively discussed in modern science and practice, includes various types of electrical
stimulation. Constant stimulation of the nervous system is one of the most popular ways to activate neural
networks in order to activate the brain and initiate neuroplasticity processes. Participants in the experiment
were children with cerebral palsy, spastic diplegia form at the age of 6 to 19 (n=6) (mean age - 17,9 ± 5,6
years). All subjects underwent standard treatment, including massage, therapeutic gymnastics simulators,
robotic mechanotherapy, etc., which lasted 20-25 minutes with neurostimulation of the brain (using a PoNS
device). All subjects underwent a functional brain imaging (MRI) before and after neurostimulation course.
Results indicate positive dynamics in all subjects: most of them learned walking without aids, decreased
muscle tonus and improvement in balance, coordination function were noted. Neurostimulation with the PonS
device combined with curative gymnastics (focused exercises), improves the efficiency of motor functions
and development of motor skills. Functional MRI with an active paradigm, with proper and high-quality
performance, is an auxiliary method of objective control of treatment effectiveness.
1 INTRODUCTION
In subjects with cerebral palsy, there are obvious
violations of equilibrium, position of motion,
retention of the pose in space. Each function of the
human body is based on well-organized complex
neural networks, including numerous interconnected
structures (cortex, nuclei, neural clusters) located in
different levels of brain and spinal cord. Collaboration
and synchronization of human performance in
behavioral, cognitive and autonomic functions. This
close integration is especially important in complex
sensory and motor functions, such as vision, hearing,
balance, gait, speech.
Neurorehabilitation of children with cerebral
palsy is multicomponent and includes physiotherapy,
special massage therapy, treatment, special limb
treatment with different stitches, the use of fixing
devices for walking, special, facilitating the motor
activity of the child, and costumes. In modern
medicine, the problems of rehabilitation of children
with cerebral palsy are given particular attention. A
new direction of neurorehabilitation, intensively
discussed in modern science and practice, is the use of
various types of electrostimulation, as well as their
use in or in combination with existing procedures. The
most common among them - electrical stimulation of
muscles and nerves, as well as the spinal cord.
Electrical stimulation was used to treat spastic Erb-
Duchenne paralysis in 1871. Since that time treating
patients with spasticity by electrostimulation of
muscles and nerve structures used in psychotherapy,
the subcutaneous, epidural location of the electrodes,
as well as peroneal implantation (Svozil et al. 2015,
Kublanov et al. 2008). Despite the positive results
achieved by the integrated treatment approach, the
problem of rehabilitation of children with cerebral
palsy in the late residual stage with persistent
stereotypes remains unresolved. The problems of
restoring muscle control and complex sensorimotor
integration (balance, coordination of movement,
retention of the body in space) have so far not been
332
Ignatova, T., Kolbin, V., Scherbak, S., Sarana, A., Sokolov, A., Trufanov, G., Semibratov, N., Ryzhkov, A., Efimtsev, A. and Danilov, Y.
Translingual Neurostimulation in Treatment of Children with Cerebral Palsy in the Late Residual Stage. Case Study.
DOI: 10.5220/0006732403320337
In Proceedings of the 11th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2018) - Volume 4: BIOSIGNALS, pages 332-337
ISBN: 978-989-758-279-0
Copyright © 2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

given great attention. Artificial stimulation of the
nervous system is one of the most popular ways to
activate neural networks in order to activate the brain
and initiate neuroplasticity processes (Petrenko et al.
2017).
2 MATERIALS AND METHODS
2.1 Participants
This study involved 6 children with cerebrally palsy,
form of spastic diplegia. Patients with intact intellect,
no seizures in anamnesis. All children obtained
standard treatment, including massage, medical
gymnastics with simulators, robotic mechanotherapy,
hydrotherapy, and 10 daily sessions of physical
therapy, which lasted for 20-25 minutes and
neurostimulation of the brain (using the PonS device).
Patients underwent functional MRI of the brain before
the start of and at the end of the course of treatment
using neurostimulation. The patients were aged 8 to
14 years. Patients were evaluated by standard scales
GMFSC Scale (gross motor skills), FMS (functional
motor scale), Berg balance scale, the Ashworth scale
(spasticity). 5 patients with a GMFCS level of
development 3 field of the treatment received positive
dynamics in FMS.
2.2 Neurostimulation
Along with the existing modern high-performance
methods of use of peripheral nerve stimulation
(Kublanov et al. 2017), an innovative method was
developed at the University of the state of Wisconsin,
USA, in the laboratory, which was headed by
renowned scientist Paul Bach-y-Rita, one of the
founders of the modern concept of neuroplasticity. An
instrument for electrotactile stimulation of human
skin, in the most densely innervated tactile region -
the tongue, was designed in the laboratory of tactile
communication and neurorehabilitation (TCNL)
(Danilov et al. 2008). Electrotactile stimulation of
language is, at the moment, the most effective and
safe stimulation of the Central nervous system.
Language is the most thin portion relative to the other
surfaces of the skin, full of different types of
mechano-, thermo - and taste buds, with the addition
of free nerve endings. This area has the highest
density of mechanoreceptors per unit area and has a
minimum two-point discrimination threshold: 0.5-1
mm for mechanical stimulation and 0.25-0.5 mm for
electrical stimulation (Danilov et al. 2006, Danilov et
al. 2007). Two major cranial nerves (branch of
trigeminal, 20-22 000 nerve fibers and the facial
nerve, 3-6000 nerve fibres) from the anterior surface
of the tongue provide the transmission of nerve
impulses directly to the structure of the brain stem,
activating the complex nuclei of the trigeminal nerve
(mesencephalic, sensory and spinal cord-the large
core of the trunk) and, at the same time, neighboring
nucleus of solitary tract on the branch of the facial
nerve is stimulated. The cochlear nuclei are being
activated as well, medulla and upper sections of the
cervical spine (C2 and C3). The reticular formation of
the brain stem, a complex of vestibular nuclei and the
ventral part of the cerebellum enters the area of
secondary activation (Barbara et al. 2009). As is
known, the area of the brain stem has a large cluster
of neuronal nuclei (N=86), some of them engaged in
Autonomous regulation (circulation, respiration), and
other sensorimotor integration. One should not
exclude possible secondary activation of several
common systems of neurochemical regulation of
activity of brain nuclei located in the brainstem –
noradrenergic, dopamine-mediated error, and
acetylcholinergic by dopamine and serotonin. From
the same region the trigeminal-spinal path, regulating
the activity of spinal motoneurons, goes down
solitary-three spinal and Vestibulo-spinal directly
involved in the regulation of the activity of the lower
limbs and walk (Michelle et al. 2009). Intense
rhythmic stimulation of active neurons leads to a
corresponding activation of synaptic contacts and
axon, including the whole complex of pre - and
postsynaptic neurochemical mechanisms. Such
phenomena as long potentiate or depression of neural
networks may underlie the effects observed when
using electrotactile stimulation of the tongue.
Potentiate long-term (Long-termpotentiation, LTP)
and long-term depression (Longterminhibition, LTI),
this enhancement/inhibition of synaptic transmission
between two neurons that persist long after exposure
to the synaptic pathway. LTP is involved in the
mechanisms of synaptic plasticity provides the
nervous system of a living organism the ability to
adapt to changing environmental conditions. Most
theorists of neurophysiology believe that long-term
potentiate together with long-term depression
underlie the cellular mechanisms of learning and
memory (Danilov et al. 2008).
At the moment, the device for electrotactile
stimulation is called PoNS (Portable
Neurostimulator), and its use for stimulation of the
brain in children with cerebral palsy is a new direction
in neurorehabilitation. The matrix, in which are the
electrodes of irregular shape; optimized to stimulate
the most sensitive areas of language (Fig.1A). The
Translingual Neurostimulation in Treatment of Children with Cerebral Palsy in the Late Residual Stage. Case Study
333
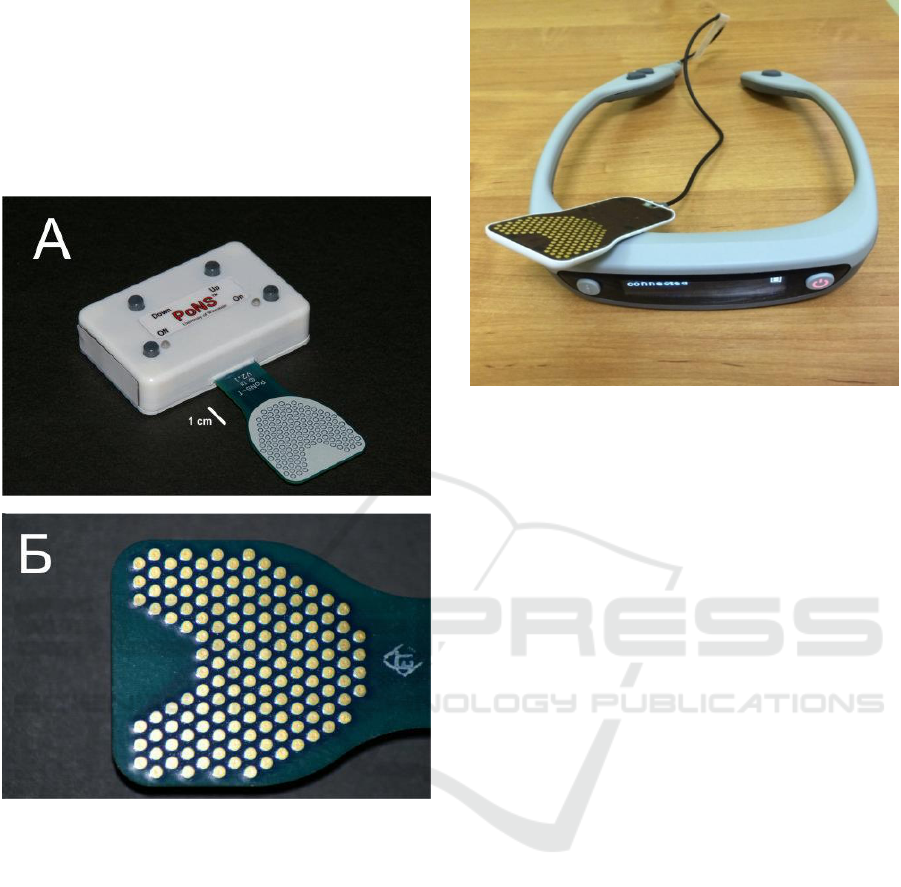
matrix itself includes 143 electrodes divided into nine
16 - electrode sectors (Fig.1B). Within each sector,
only one electrode is active at a given time, the rest
are grounded. Stimulation through one electrode
occur simultaneously in nine sectors. The electrodes
are alternated with a frequency of 50 Hz. The
incentive is a triplet of rectangular pulses of
microsecond duration.
Figure 1: The PoNS device (Portable Neurostimulator).
Appearance (A) and close-up of the matrix (B).
Regular stimulation of the PonS device,
activating an extensive region of the brain, increases
the efficiency of existing neural networks, increases
the likelihood of the formation of new synaptic
contacts (synaptogenesis), enhances the innate ability
of the brain to improve motor functions. The purpose
of a successful rehabilitation when such stimulation
to restore motor function or to teach new motor skills
is done by combining specialized exercises with a
wide activation of the brain with the PoNS device.
The studies were conducted in patients with
peripheral and Central vestibular disorders (Lomo
2003, Badke et al. 2011, Amanda and Raza 2014,
Kublanov 2008), multiple sclerosis (Kublanov et al.
2010), stroke and ischemic damage (Danilov et al.
2015), head injury and spinal cord injury
Figure 2: The PoNS device (Portable Neurostimulator).
New design.
(Wildenberg 2011, Wildenberg et al. 2013). High
effectiveness of peripheral neurostimulation in
combination with a specialized physical therapy to
restore motor control of the body, balance, walking,
speech, eye movements, different aspects of
sensorimotor integration was shown. Additional
studies, using functional MRI, unambiguously
confirmed the presence of a powerful activation of
the brain stem and ventral parts of the cerebellum
upon stimulation of the tongue, and also the long-
term effects of after-effect, the persistence of pockets
of activity in the brain of subjects for hours or even
days after the last stimulation (Bach-y-Rita 2003,
Joseph et al. 2011). Additional data analysis showed
that while the activation of subcortical structures of
the brain are changed and the coefficients of coupling
between areas of the cerebral cortex involved in the
integrative processes of training (Petrenko et al.
2017).
2.3 fMRI Data Acquisition and
Postprocessing
To investigate the organization of functions, to
localize activated cortical areas and to assess the
therapeutic effect we used functional magnetic
resonance imaging. Conventional T1- and T2-
weighted images in three orthogonal planes were
obtained also. fMRI was performed on 3.0 T MR-
scanner with BOLD (Blood Oxygenation Level
Dependent) technique. Functional MR images were
acquired using echo-planar imaging (EPI) with
repetition time (TR) = 3000 ms, echo time (TE) = 50
ms, flip angle = 90º, field of view (FOV) = 230 mm
NENT 2018 - Special Session on Neuro-electrostimulation in Neurorehabilitation Tasks
334
and matrix size 128*128. The research was carried out
using active movement functional paradigms for each
extremity (both feet and hands) and active count
paradigm for patients who could perform these tasks
and depending on clinical status, and passive
movement or sensory paradigms was performed for
those, who could not. Besides, a “virtual walking”
paradigm was performed to some patients: they had to
imagine they walk. Each activation paradigm lasted
5 minutes with five epochs of movement, 30 seconds
each. Taking into consideration patients’
hyperactivity, scanning protocol (number of
performed paradigms) could be reduced in some cases
to focus on most weak extremity (hand and leg). To
obtain high resolution images of whole brain for
Talairach coregistration and reslicing along different
planes, we used 3D MPRAGE (Magnetization
Prepared Rapid Acquisition Gradient Echo) – T1-
sequence with the following parameters: repetition
time (TR) = 2000 ms, echo time (TE) = 4,38 ms, flip
angle = 10º, field of view (FOV) = 250 mm, 160 slices
and matrix size 256*256. Processing of neuroimaging
data with the identification of activation sites in each
patient and evaluation of the results were carried out
using the software package SPM12 (Welcome
Department of Imaging Neuroscience, University
College, London, UK) software package running
under MATLAB R2011b (The Mathworks, Sherborn,
MA, USA) programming. Template space was
defined by standard EPI template data in SPM (MNI
coordinates - Montreal neurologic Institute, McGill
University, Montreal, Canada).
3 RESULTS
The first patient before the treatment was able to walk
using multisupporting canes within the room, and for
longer distances used walkers (500 meters or more),
after a course of treatment learned to walk using one
cane single-bearing alternator within the room and in
school, for longer distances uses a multisupporting
cane. The second patient before treatment used
multisupporting canes to walk across the room and on
the street, could not stand alone without support; the
end of the course of treatment learned to walk
independently on a level surface (within the room),
the patient can stand on his own without support, in
school and on the street uses one single-bearing
alternator cane. The third patient before the start of
treatment used to walk the Walker across the room, at
school, and for longer distances used stroller. Upon
completion of the course of treatment the patient has
mastered multisupporting cane across the room, uses
a Walker in school and can go to the playground, for
longer distances use stroller active type. A fourth
patient before treatment went using two single-
bearing alternator canes within the space and outside,
independently and without reliance might stand for a
few seconds at the end of the course of treatment
learned to walk independently on level surfaces,
standing safely alone on the street uses one single-
bearing alternator cane. Patient N5 before treatment
used multisupporting canes for walking, at the end of
treatment mastered walking within the premise of
relying on one single-bearing alternator cane, for
longer distances uses a multisupporting cane. Patients
N6 with the level of development GMFSC 4, before
the treatment could move around within the premises
using a walker, at school and on the street used active
type stroller, at the end of the treatment the patient
learned to walk with the use of multisupporting canes
within the premises and in school, for longer distances
confidently uses a Walker. Also all patients noted
decreased muscle tone and improve balance,
coordination functions. Improvement of balance,
assessed on a scale of Berg, ranged from two to seven
units (average 4.5) and as a percentage of the original
state improvement was observed from 12 to 70 %
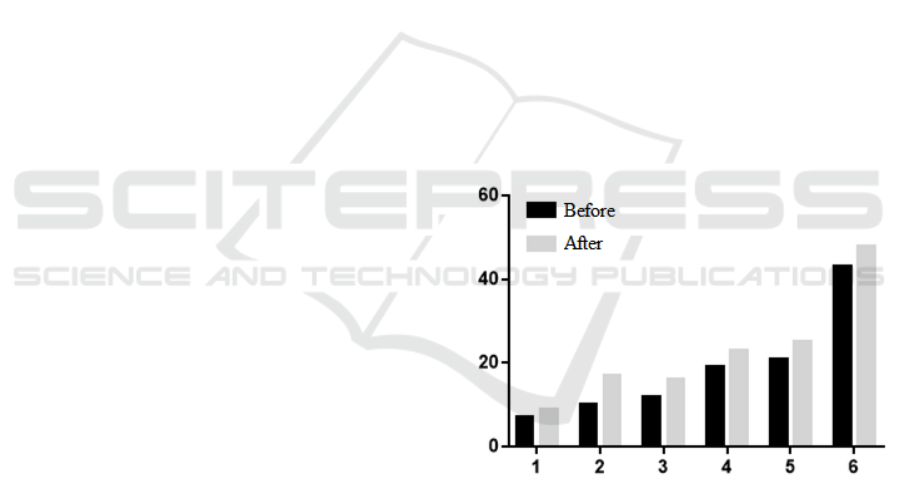
(average 31%). (Fig. 3)
Figure 3: Dynamical differences in patients by Berg balance
scale (black – before, grey - after).
According to obtained fMRI data for each subject
individually, we detected activations of
corresponding areas in response to presentation of
movement stimuli, active and passive, located in the
hemispheres, before and after neurostimulation.
First patient showed increased activation in right
hand motor area, and activation in foot motor area in
response to “virtual walking” paradigm after
neurostiumulation (before it was weaker and appeared
in “wrong place”) (Fig.4). Patients N4 and N6 showed
significant changes in activation patterns for foot and
hand motor areas. All other patients also have had
Translingual Neurostimulation in Treatment of Children with Cerebral Palsy in the Late Residual Stage. Case Study
335
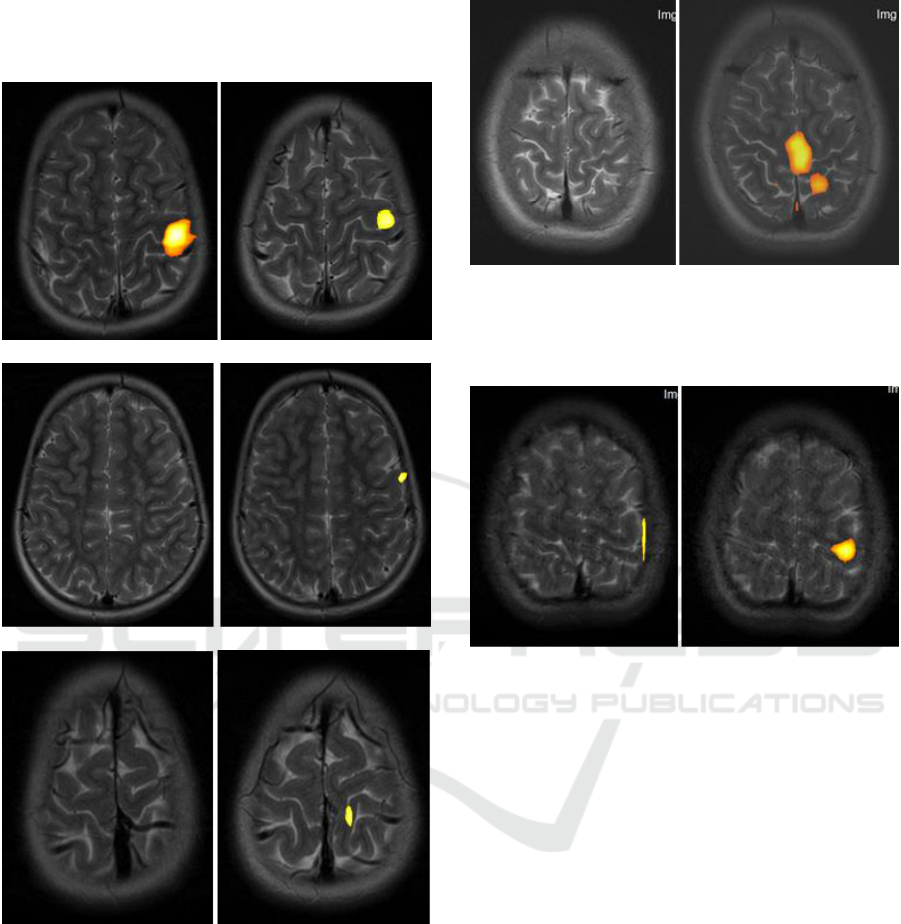
more expressed activations in response to different
stimuli, primarily in foot motor areas and in response
to “virtual walking”.
A B
C D
E F
Figure 4: Activation areas in patient N1. A, B – right hand
fingers movement, С, D – count paradigm active response,
E, F – right leg movement activation, before and after
neurostimulation respectively.
4 CONCLUSIONS
Given the limitations and the minimum intensity of
the workouts, the main objective of the study was
limited by the formation of new motor skills. The
patient had to form a new motor skill in 10 sessions,
A B
Figure 5: Activation areas in patient N6. Illustration of
activation pattern in projection of left leg motor area before
(A) and after (B) neurostimulation.
A B
Figure 6: Activation areas in patient N4. Illustration of
activation pattern in projection of right hand motor area
before (A) and after (B) neurostimulation.
to strengthen it and to confidently use in a daily life.
Based on these considerations, it is understandable
why overall motor control (scale FМS) statistically
significantly improved. Since the task was to develop
the skills of motor control, these neural networks
improved their functional activity as a result of the
neurostimulation. This technique is non-invasive,
innovative in the field of neurostimulation, safe and
easy to use. Daily 20 minute stimulation of the tongue
within two weeks increases the innate ability of the
brain to improve motor function, promotes the
formation of new motor skills. Neurostimulation with
the use of PoNS device, combined with therapeutic
exercises (targeted sessions) allows to improve the
efficiency of recovery of motor function and motor
skills development. Functional MRI active
paradigms, with proper and high-quality
implementation is an auxiliary method of the
objective control of efficiency of treatment.
NENT 2018 - Special Session on Neuro-electrostimulation in Neurorehabilitation Tasks
336

REFERENCES
Aicardi J., Protsenko, S. V., Barashkova, A. A. T Skorosze,
2013. Diseases of the nervous system in children.
BINOM. 568.
Svozil, A. V., Morenko E. S., Vissarionov.In. In Umnov.In.
Manushkina T. R., Gerasimenko, Y. P., Baindurashvili
A. G., 2015. Functional and spinal stimulation in
comprehensive rehabilitation with cerebral palsy.
Vedical. 2: 40-46.
Danilov, Y. P., Tyler, M. E., Kaczmarek K. A., 2008.
Vestibular sensory substitution using tongue
electrotactile display. Human Haptic Perception: Basics
and Applications. Birkhauser Basel Switzerland. 467-
480.
Danilov, Y.P., M.E. Tyler, K.L. Skinner, R.A. Hogle, and
P. Bachy-Rita, 2007. Efficacy of electrotactile
vestibular substitution in patients with peripheral and
central vestibular loss. J Vestib Res, (17), 119–130.
Danilov, Y.P., Tyler M.E., Skinner K.L., Bach-y-Rita P.,
2006. Efficacy of electrotactile vestibular substitution in
patients with bilateral vestibular and central balance
loss. Conf Proc IEEE Eng Med Biol Soc, 6605–6609.
Barbara Susan Robinson, PT, DPT, Jeanne L. Cook, PT,vs,
Cynthia McCormick Richburg, PhP, CCC-A, and
Stephen Pria, PT, MPT, 2009. Use of an Electotactile
Vestibular Substitution System to Facilitate Balance fnd
Gait of an Individual with Gentamicin- Induced
Bilateral Vestibular Hypofunction and Bilateral
Transtibial Amputation. JNPT, (33), 150-159.
Mitchele E. Tyler, Member IEEE, Jacquelin G and Yuri P.
Danilov, 2009. Spatial Vapping of Eltctrotactile
Sensation Threshold and Intersty Range jn the Human
Tongue: Initial Results. Conf Proc IEEE Eng Med Biol
Soc, (4), 559-562.
Danilov Y.P, Tyler M.E., Skinner K.L., Hogle R.A., Bach-
y-Rita P, 2007. Efficacy of electrotactile vestibular
substitution in patients with peripheral and central
vestibular loss. Journal of Vestibular Research, (17),
119-130.
Danilov, Y. P., Tyler, M. E., Kaczmarek K. A. Vestibular
sensory substitution using tongue electrotactile display,
2008. Human Haptic Perception: Basics and
Applications. Birkhauser Basel Switzerland, (4), 467-
480.
Lomo T., 2003. The discovery of long-term potentiation.
Philos Trans R Soc Lond B Biol Sci, (4), 17-20.
Badke MB, Sherman J, Boyne P, Page S, Dunning K., 2011.
Tongue-based biofeedback for balance in stroke:results
of an 8-week pilot study. Arch Phys Med Rehabil, (13),
64-70.
Amanda E Chisholm, Raza Naseem Malik, Jean-Sébastien
Blouin, Jaimie Borisoff, Susan Forwell Tania Lam,
2014. Feasibility of sensory tongue stimulation
combined with task-specific therapy in people with
spinal cord injury. Journal of NeuroEngineering and
Rehabilitation, (1), 96.
Kublanov, V.S., 2008. A hardware-software system for
diagnosis and correction of autonomic dysfunctions.
Biomed. Eng. (6), 206–212.
Kublanov, V.S., Danilova, I.G., Goette, I.F., Brykina, I.A.,
Shalyagin, M.A., 2010. Application of Spatially
Distributed Field of Electric Impulses for Correction of
Angiogenesis in Ischemic Muscular Tissue. Int. J.
Biomed. Sci. IJBS 6, 310.
Kublanov, V.S., Babich, M., Dolganov, A., 2017. Principles
of Organization and Control of the New Implementation
of the" SYMPATHOCOR-01" Neuro-
electrostimulation Device. In: BIOSIGNALS. pp. 276–
282.
Danilov Y., Kaczmarek, K. Skinner K., Tyler M., 2015.
Cranial nerve noninvasive neuromodulation: New
approach to neurorehabilitation: Brain neurotrauma:
Molecular, neuropsychological, and rehabilitation
aspects: CRC Press, (23), 605-628.
Bach-y-Rita P., 2008. Late postacute neurologic
rehabilitation: Neuroscience, engineering, and clinical
programs. Arch Phys Med Rehabil, (8), 1100–1108.
Wildenberg J., Tyler M.E., Danilov Y.P., Kaczmarek K.,
Meyerand M., 2013. Altered Cоnnectivity of the
Balance Proccessing Network After Tongue
Stimulation in Balance-Impaired Individuals. Brain
Connectivity, (10), 87-97.
Wildenberg J., Tyler M.E., Danilov Y.P., Kaczmarek K.,
Meyerand M., 2011. High-resolution fMRI defects
neuromodulation of individual brainstem nuclei by
electrical tongue stimulation in balance-impaired
individuals. Neuroimage, 56 (8), 2129-2137.
Wildenberg J., Tyler M.E., Danilov Y.P., Kaczmarek K.,
Meyerand M., 2011. Electical Tongue Stimulation
Normalires Activity Within the Motion-Sensitive Brain
Networt in Balance-Impaired Subjects as Revealed by
Group Indtpendent Component Analysis. Brain
connectivity, (3), 255-265.
Bach-y-Rita P., 2003. Theoretical basis for brain plasticity
after a TBI. Brain Inj, (8), 643–651.
Joseph C. Wildenberg, Mitchell E.Tyler, Yuri P. Danilov,
Kurt A. Kaczmarek, Mary E., 2011. Meyerand High-
resolution fMRI detects neuromodulation of individual
brainstem nuclei by electrical tongue stimulation in
balance-impaired individuals. Journal Neurolmage, (8),
2129-2137.
Petrenko, T., Kublanov, V., Retyunskiy, K., 2017. The role
of neuroplasticity in the treatment of cognitive
impairments by means multifactor neuro-
electrostimulation of the segmental level of the
autonomic nervous system. Eur. Psychiatry, 770.
Translingual Neurostimulation in Treatment of Children with Cerebral Palsy in the Late Residual Stage. Case Study
337
