
Development of a Parameter Calculator in Cardiovascular Perfusion
BioMEP as a Tool for the Register of Physiological Parameters
Inês Dias
1
, Pedro Fonseca
2
,
Duarte Furtado
2
, Inês Figueira
2
, Paulo Franco
2
, Vanda Cláudio
2
,
Helena Antunes
2
, José Fragata
2
, Cláudia Quaresma
1,3
and Carla Quintão
1,3
1
Departamento de Física, Faculdade de Ciências e Tecnologia da Universidade Nova de Lisboa, Caparica, Portugal
2
Serviço de Cirurgia Cardiotorácica - Hospital de Santa Marta, Centro Hospitalar de Lisboa Central, Lisboa, Portugal
3
LIBPhys - UNL, Faculdade de Ciências e Tecnologia da Universidade Nova de Lisboa, Caparica, Portugal
Keywords: Physiological Parameters, Calculator, Cardiovascular Perfusion, Cardiothoracic Surgeries, Software.
Abstract: Technology has played an increasingly important role in the health sector, with new devices allowing for
better real-time monitoring of patients’ biosignals. Among those, the ones developed with perfusion in mind
are extremely useful, during cardiothoracic surgery, since they provide detailed information about the vital
signs of the patient. However, doctors and technicians have often to calculate several physiological
parameters, which help them make clinical decision during such surgical interventions. In this context, the
authors present a software tool – BioMEP: Perfusion Calculator Application, built in a partnership between
the Department of Cardiothoracic Surgery of Santa Marta Hospital and the Department of Physics of the
Faculty of Sciences and Technology of the NOVA University of Lisbon, and which fulfils the needs of the
surgical team. BioMEP - Perfusion Calculator Application is a safe, intuitive and user-friendly tool that
incorporates and integrates department-specific perfusion parameters and calculations, in a single platform,
and allows for higher intervention efficiency, while minimizing the errors of the required calculation, with
the concomitant improvement in patient safety.
1 INTRODUCTION
Medicine is often an early adopter of new scientific
and technological breakthroughs. Never like today,
technology as had a higher impact in the healthcare
sector. One of the most impressive of such
advancements is the possibility to collect and store
vast amounts data, as well as make them available to
support real time decision making (Brettlecker et al.,
2008). Critical to such progress are computer and
mobile applications, which are becoming ubiquitous
in all healthcare environments. Many reports state
that those tools are helpful in the way they allow for
better clinical decisions as well as improve patients’
outcomes (Ventola, 2014).
Cardiovascular perfusion, as an important area in
medical surgical care, is no exception to the stated
above. That type of extracorporeal circulation
procedure consists in replacing, temporarily, the
pulmonary and heart functions, through specific
circuits, techniques and medical equipment. In that
process, patient’s blood enters a mechanical system
that filters, promotes its oxygenation and regulates its
temperature (Gravlee et al., 2008). When arterialized,
patient’s blood returns to the systemic circulation,
with the help of a pump that substitutes the heart. The
extracorporeal circulation replaces the
cardiopulmonary functions, while preserving the
cellular integrity, as well as the structure, function
and metabolism of the organs and systems of the
patient, during complex cardiothoracic surgeries
(Gravlee et al., 2008). There are, in current use,
several free to use applications that assist
perfusionists in their surgically demanding and
complex tasks, (cf, i-Perfuse, 2014; i-Pump, 2013).
They calculate certain physiological parameters; give
cannula recommendations; allow users to take
quizzes and present news with the latest information
on the subject. Despite all these functionalities, both
applications lack in the calculation of a great variety
of physiological parameters, which are essential to
perfusionists during surgeries. Those include:
• priming calculations
• heparin and protamine levels, at the different
temperatures that the body is cooled
• post dilutional haematocrit levels
254
Dias, I., Fonseca, P., Furtado, D., Figueira, I., Franco, P., Cláudio, V., Antunes, H., Fragata, J., Quaresma, C. and Quintão, C.
Development of a Parameter Calculator in Cardiovascular Perfusion - BioMEP as a Tool for the Register of Physiological Parameters.
DOI: 10.5220/0006723502540257
In Proceedings of the 11th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2018) - Volume 1: BIODEVICES, pages 254-257
ISBN: 978-989-758-277-6
Copyright © 2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

These values are extremely important for the
preservation of the integrity of the patients’ body, in
various cardiothoracic procedures, as they give
invaluable insights and information to clinicians.
Furthermore, no single calculator integrated all the
information of relevance for such procedure.
Practitioners were then left to employ a variety of
non-communicating tools, which increased the
possibility of information misuse.
For the aforementioned reasons, we developed a
new application that calculates, automatically, all
parameters deemed essential during surgery. Such
clinical tool, presented in this manuscript, is called
BioMEP- Perfusion Calculator Application.
2 APPLICATION
REQUIREMENTS
BioMEP was developed in a close collaboration
between physicians and perfusionists, from the
Cardiothoracic Surgery Department of Hospital de
Santa Marta partnership, and biomedical engineers,
from the Physics Department of Faculdade de
Ciências e Tecnologia of Universidade Nova de
Lisboa.
The main goal of the proposed application is to
calculate and integrate, automatically, biometric and
physiological parameters of the patient, during
cardiothoracic surgery. Together with clinicians and
surgeons, and after evaluating the most commonly
used perfusion applications, the following list of
requirements were drawn for BioMEP:
• be user-friendly
• be in digital format
• divided in blocks – each one dedicated to a
specific topic
• allow the user to insert new data
• calculate, automatically, various biometrics and
physiological parameters
• provide relevant data reports
BioMEP was developed using the programming
language MATLAB’s R2012b (MathWorks ©). The
content was designed keeping in mind the definition
of what parameters were worth calculating and what
formulas they required. All calculations of the various
physiological parameters, such as heparin and
protamine levels were assessed through literature
(Gravlee et al., 2008). The entire set of algorithms
was simplified, so that the application would run
faster, and present an easy-to-use interface, while
allowing the access to programming code, if one
needed to construct other specific functions, for any
given parameter. There is no need for the user to see
all the moving information in the application. Yet
there is great value in the complete interaction
between the various elements of the application.
Hence all functions interacted internally with each
other, to register the values inserted by the clinicians,
and to calculate and show the needed parameters.
3 IMPLEMENTATION
The built application is divided in six fundamental
blocks, which interact internally between each other,
each of them dedicated to a specific topic, calculating
automatically several parameters using the empirical
expressions found in the literature (Gravlee et al.,
2008). The six blocks are:
• Biometric Data
• Priming
• Blood flow
• Heparin and protamine doses
• Modified ultrafiltration
• Post-dilution haematocrit
In the biometrics block (figure 1), the clinician can
insert the biometric data, such as: the identification
number, the age, the gender, the weight and the height
of the patient as the correspondent fields for these
parameters are available for the user to insert and
modify if needed. The body surface area is
automatically calculated:
In the priming block (figure 2) the user should decide
the priming type (hematic/non-hematic) and should
type the values of the priming polyelectrolyte solution
in ml and the priming Heparin dose in UI. If the
priming type was chosen, Packed Red Blood Cells
(PRBC), the Fresh Frozen Plasma (FFP) and the
Calcium Gluconate values in ml should be also
inserted manually. The outputs that are automatically
computed are:
Mannitol (20%) = 2.5 ×
NaHCO
3
= 1×, if the ratio (ml/kg) = 1 was
chosen
NaHCO
3
= 0.5×, if the ratio (ml/kg) = 0.5
was chosen
Mannitol dose for rewarming = 1.5×
Development of a Parameter Calculator in Cardiovascular Perfusion - BioMEP as a Tool for the Register of Physiological Parameters
255
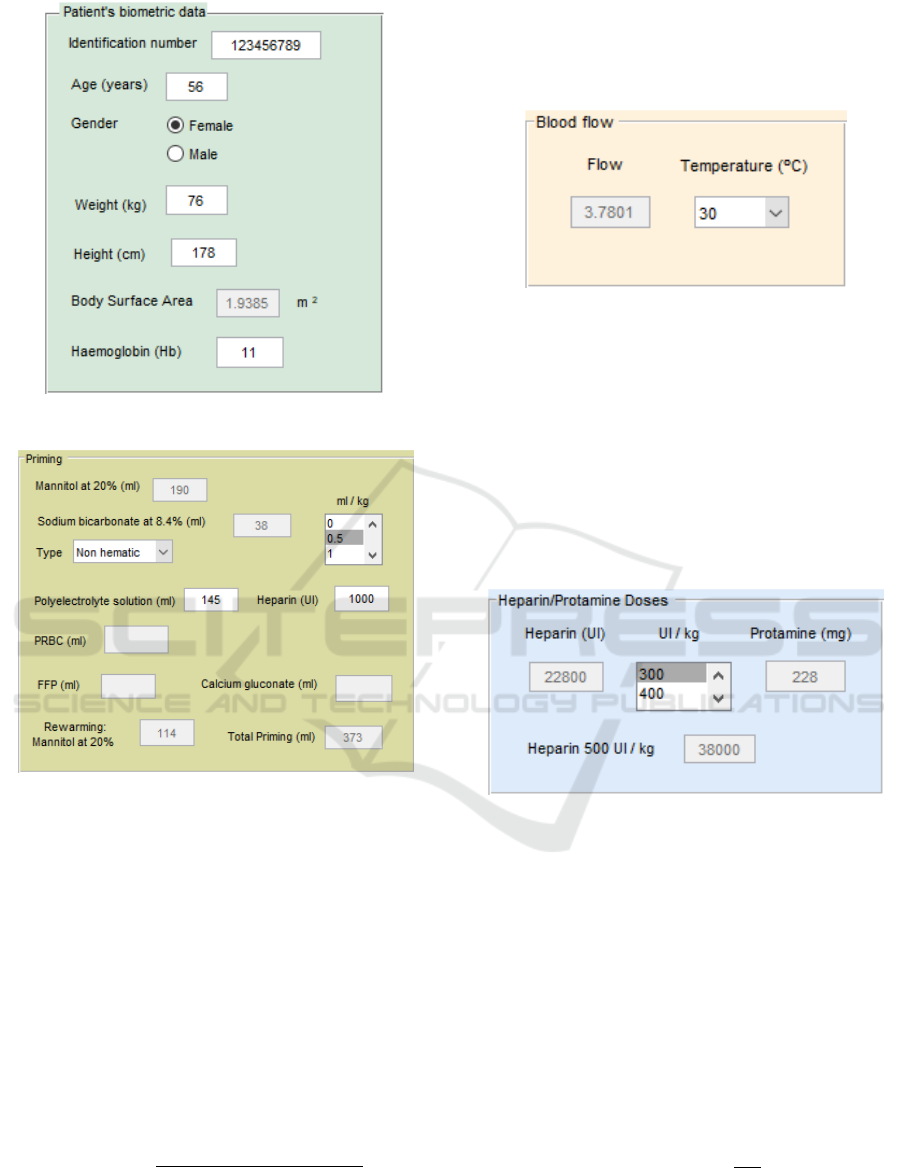
Figure 1: Interface block with the biometric data.
Figure 2: Interface block concerning priming data.
Total Priming Volume, which is the sum of all
other parameters of priming block, but the mannitol
at 20% and the heparin.
In the blood flow block (figure 3), when a specific
temperature is selected, the blood flow value at the
corresponding temperature is displayed.
The empirical expressions used in the application
are:
This information is particularly important, since some
parameters as the blood flow of the patient depend
crucially on the temperature at which the body was
cooled (Gravlee et al., 2008).
Figure 3: Interface block related to blood flow.
In heparin/protamine doses blocks, (figure 4)
heparin and protamine doses and the maximum value
of heparin that can be administrated (Heparine 500
UI/kg) are calculated automatically with the input of
patient’s weight:
Heparin dose (300 UI/kg)
Heparin dose (400 UI/kg)
Protamine dose (3 mg/kg)
Protamine dose (4 mg/kg)
Figure 4: The heparin/protamine doses block.
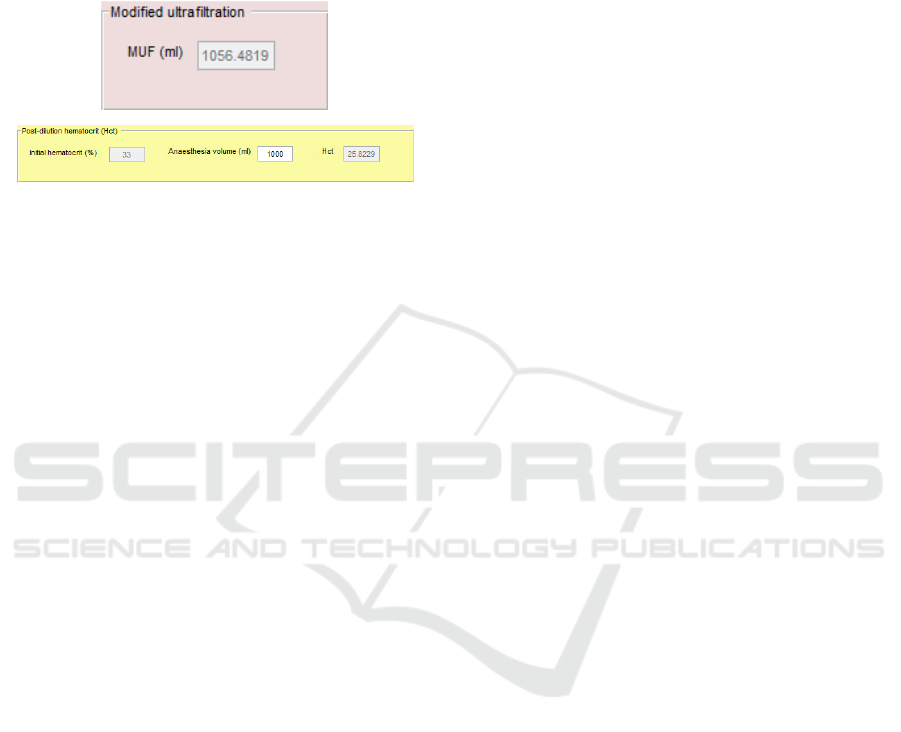
There are further two blocks in which the
modified ultrafiltration volume (ml), the initial
haematocrit (%) and post-dilution haematocrit (%)
were calculated, given the anaesthesia fluids volume
(ml) (figure 5):
The percentage of the post-dilution haematocrit is
then calculated by:
,
where: Hct pt is the initial haematocrit of the patient;
BV
pt
is his blood volume; and TPV is the total priming
volume.
BIODEVICES 2018 - 11th International Conference on Biomedical Electronics and Devices
256
In summary, the heparin and protamine doses,
priming parameters, dilutional haematocrit and
modified ultrafiltration volume are automatically
calculated and displayed in the corresponding fields,
remaining unavailable for the user to modify, since
they are generated by the software.
Figure 5: The interface blocks concerning modified
ultrafiltration and post-dilution haematocrit.
BioMEP – Perfusion Calculator Application is
also prepared for input errors of the user, rejecting
data inserted that is not expected by the application
(letters, characters, and so on). In this case, no
calculations involved the wrong parameter are
performed by the software, leaving the values to zero.
The clinician can correct in real time those parameters
inserted and the calculations are then correctly
performed.
If the health care professional wishes to add the
application data to the perfusion report at the end of
the procedure, a print option is also available. When
closing the application, all generated data is deleted
to make sure that all the values of the current patient
do not get mixed with the parameters of the next
subject.
4 DISCUSSION
In the current manuscript we have proposed a new
application, BioMEP, which can be applied in the
field of cardiovascular perfusion and cardiothoracic
surgery (both adult and pediatric procedures). Before
the advent of technology, such as the one presented
here, professionals had to calculate all relevant
biometric and physiological values by hand. In a
Hospital specialised in cardiothoracic interventions,
such as Hospital de Santa Marta, four cardiothoracic
surgeries are performed, in average, each day, which
totals over 1000 such surgeries every year. Any help
reducing the workload of the highly specialised
personnel present in a surgical scenario has a very
high potential impact.
In addition, BioMEP allows for higher efficiency
in handling data, and a concomitant reduction in
potential sources of mistake, since data transport
between calculations is done automatically.
After some trials, the BioMEP has been deemed a
useful, safe, user-friendly and intuitive tool. It is
currently in test use at the Department of
Cardiothoracic Surgery, with very positive feedback
from surgeons’ teams.
Although fully functioning, the natural
evolutional step for the proposed application
interface, presented in this manuscript, is to export the
current computer-based tool to a more useful
smartphone platform., Because of the modularity of
the application, we may envision other improvements
in the future, such as to include the calculation of new
physiological parameters that may add further
information to surgery procedures.
The BioMEP is an innovative application, very
well received by the cardiothoracic surgery
community, which is showing very promising
practical applicability levels. It shows to be reliable,
easy to use, and capable of combining multiple
anatomical and physiological calculations. New
developments may include the calculation of further
parameters, provide cannula recommendations, as
well as perfusion guidelines.
ACKNOWLEDGEMENTS
The authors would like to thank all the healthcare
professionals of the perfusion team at Hospital de
Santa Marta and to Ricardo Vigário for the revision
on some parts of the manuscript and for his valuable
comments and suggestions.
REFERENCES
Brettlecker, G., Cáceres, C., Fernández, A., Fröhlich, N.,
Kinnunen, A., Ossowski, S., Schuldt, H., Vasirani, M.,
2008. Technology in Healthcare. In CASCOM:
Intelligent Service Coordination in the Semantic Web.
Birkhäuser Basel.
Gravlee, G., Davis, R., Stammers, A., Alfred, H,
Ungerleider, R., 2008. Cardiopulmonary Bypass:
Principles and Practice. Lippincott Williams &
Wilkins. Philadelphia, 3
rd
edition.
i-Perfuse Mobile Application for Perfusionists, 2014,
Courtland Menke
i-Pump, 2013, Perfusion.com, Inc.
MathWorks, 2017, MATLAB Documentation.
Ventola, C., 2014, Mobile devices and apps for health care
professionals: uses and benefits. In P & T: a peer-
reviewed journal for formulary management,
MediMedia USA, Inc.
Development of a Parameter Calculator in Cardiovascular Perfusion - BioMEP as a Tool for the Register of Physiological Parameters
257
