
Supporting Multiple Agents in the Execution of Clinical Guidelines
Alessio Bottrighi, Luca Piovesan and Paolo Terenziani
DISIT, Universitá del Piemonte Orientale, Viale Teresa Michel 11, Alessandria, Italy
Keywords: Clinical Guidelines, Physician Interaction and Communication, Human Resources Coordination.
Abstract: Clinical guidelines (GLs) exploit evidence-based medicine to enhance the quality of patient care, and to
optimize it. To achieve such goals, in many GLs different agents have to interact and cooperate in an
effective way. In many cases (e.g. in chronic disorders) the GLs recommend that the treatment is not
performed/completed in the hospital, but is continued in different contexts (e.g. at home, or in the general
practitioner’s ambulatory), under the responsibility of different agents. Delegation of responsibility between
agents is also important, as well as the possibility, for a responsible, to select the executor of an action (e.g.,
a physician main retain the responsibility of an action, but delegate to a nurse its execution). To manage
such phenomena, proper support to agent interaction and communication must be provided, providing them
with facilities for (1) treatment continuity (2) contextualization, (3) responsibility assignment and delegation
(4) check of agent “appropriateness”. In this paper we extend GLARE, a computerized GL management
system, to support such needs. We illustrate our approach by means of a practical case study.
1 INTRODUCTION
Clinical guidelines (GLs) are defined as
“systematically developed statements to assist
practitioner and patient decisions about appropriate
healthcare under specific clinical circumstances”
(Field and Lohr, 1990). They are conceived as a way
of putting Evidence-Based Medicine (EBM) into
practice, as well as a mean to grant both the quality
and the standardization of healthcare services, and
the minimization of costs. Thousands of GLs have
been devised in the last years. For instance, the
Guideline International Network (http://www.g-i-
n.net) groups 103 organisations representing 47
countries from all continents, and provides a library
of more than 6400 CPGs. Since the 90’s, the medical
community has started to recognize that a computer-
based management can further increase GL advanta-
ges, providing relevant benefits (e.g. decision
making support) to care providers and patients.
Many different systems and projects have been
developed to this purpose (see e.g. (Fridsma, 2001;
Gordon and Christensen, 1995; Peleg, 2013)). Such
systems usually provide facilities to acquire,
represent and/or execute GLs, and are mainly
developed to support physicians in patient care.
Different forms of support may be provided. In
particular, a lot of attention has been devoted to
decision support facilities (such as “what if” analysis
(Terenziani et al., 2002) or cost-benefit analysis
(Montani and Terenziani, 2006)). Notably,
computer-based approaches do not aim at
substituting physicians: although physicians may
take into account the suggestions provided by the
systems, the final decision is always left to
physicians themselves. Specifically, physicians
retain the full responsibility of taking decisions, and
of identifying the proper actions for the patients.
However, computer-based GL systems have quite
neglected the problem of properly supporting the
coordination of different healthcare agents in the
execution of GLs (see, however, the discussion in
Section 6). Indeed, while some GLs are specifically
related to an execution context (e.g., they have to be
totally executed in an hospital), others, mainly
dealing with chronic disorders, require that patient
treatment is continued in time, and is carried on in
different contexts (e.g. at home, or in the general
practitioner’s ambulatory), under the responsibility
of different agents (not only physicians). In such
cases, the correct interaction and communication
between the involved agents is critical for the quality
of care, involving the ability of identifying a proper
responsible for the next actions, and the possibility
of delegating the responsibility and\or the execution
of actions to other agents. None of the available
208
Bottrighi, A., Piovesan, L. and Terenziani, P.
Supporting Multiple Agents in the Execution of Clinical Guidelines.
DOI: 10.5220/0006654802080219
In Proceedings of the 11th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2018) - Volume 5: HEALTHINF, pages 208-219
ISBN: 978-989-758-281-3
Copyright © 2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

computerized GL systems fully addresses such
needs.
In this work, we propose an extension of a
computerized GL management tool to deal with
these needs. First, we identify the extensions to the
GL formalism needed to represent the different
pieces of information required to manage the above
phenomena. In particular, our representation
formalism supports the specification, for each
action, of the context in which it can be execute, and
of the qualification and capabilities required to its
responsible, and to its executor.
Then, we describe the facilities we have provided
to support the coordination of multi-agents
executing a GL. The main goal of such facilities is to
support a proper treatment of the patient, in such a
way that the GL actions are executed in the proper
context, under the responsibility of a proper (i.e.,
having the correct qualification and capabilities)
agent, and are executed by a proper agent. To
achieve such a goal, our facilities support:
(1) treatment continuity,
(2) action contextualization,
(3) responsibility assignment and delegation
(4) check of agent and executor
“appropriateness”.
Notably, there are several multi-agent
approaches for healthcare in the literature (see e.g.
the survey in (Isern and Moreno, 2016)), but they
consider agents as autonomous software entities. In
our approach, we consider agents as a representation
of a real entity and use a multi-agents view to
describe and support a distributed GL execution.
A practical implementation of this work is
represented by an extension of META-GLARE.
META-GLARE (Bottrighi and Terenziani, 2016) is
a recent extension of GLARE , a domain-
independent system for GL acquisition and
execution (Terenziani et al., 2008).
Resorting to the META-GLARE formalism, we
will illustrate the application of our approach to the
“management of harmful drinking and alcohol
dependence in primary care” GL developed by the
Scottish Intercollegiate Guidelines Network (SIGN)
(Scottish Intercollegiate Guidelines Network, n.d.),
which we have adapted to the Italian context.
However, although we have implemented our
approach in META-GLARE, it is worth stressing
that the methodology we propose is general and
application-independent.
The paper is structured as follows: in section 2
we describe the main features of GLARE and
META-GLARE. In section 3 we describe our
extensions to META-GLARE representation
formalism. In section 4, which is the core of the
paper, we describe the different facilities we provide
to support the distributed execution of a GL, and the
coordination of the involved agents. In section 5 we
exemplify a practical application of our approach
considering the treatment of alcohol-related
disorders. Finally, in the section 6 we address related
works and concluding remarks.
2 GLARE AND META-GLARE
META-GLARE is an evolution of GLARE, a
domain-independent system for acquisition and
execution of GLs (Terenziani et al., 2008), which we
are developing since 1997, in collaboration with the
physicians of Azienda Ospedaliera San Giovanni
Battista in Torino, Italy.
The core of GLARE (see box on the left of
Figure 1) is based on a modular architecture.
CG_KRM (Clinical Guidelines Knowledge
Representation Manager) is the main module of the
system: it manages the internal representation of GL,
and operates as a domain-independent and task-
independent knowledge server for the other
modules; moreover it permanently stores the
acquired GL in a dedicated Clinical Guidelines
Database (CG-DB). The Clinical Guidelines
Acquisition Manager (CG_AM) provides expert-
physicians with a user-friendly graphical interface to
introduce the GL into the CG_KRM and to describe
them. It may interact with four databases: the
Pharmacological DB, storing a structured list of
drugs and their costs; the Resources DB, listing the
resources that are available in a given hospital; the
ICD DB, containing an international coding system
of diseases; the Clinical DB, providing a “standard”
terminology to be used when building a new GL,
and storing the descriptions and the set of possible
values of clinical findings.
The execution module (CG-EM) executes a GL
for a specific patient, considering the patient’s data
(retrieved from the Patient DB). The schema of the
Patient DB mirrors the schema of the Clinical DB.
Therefore, the interaction with the Clinical DB
during the acquisition phase makes it possible to
automatically retrieve data from the Patient DB at
execution time. CG-EM stores the execution status
in another DB (CG Instances) and interacts with the
user-physician via a graphical interface (CG-IM).
GLARE’s architecture is open: new modules and
functionalities can be easily added if\when
necessary. In the latest years, several new modules
and\or methodologies have been added to cope with
Supporting Multiple Agents in the Execution of Clinical Guidelines
209

automatic resource-based contextualization (ADAPT
module, (Terenziani et al., 2004)), temporal
reasoning (TR, (Anselma et al., 2006)), decision
making support (DECIDE_HELP, (Montani et al.,
2005)), model-based verification (VERIFY,
(Bottrighi et al., 2010)), and comorbidities
(COMORBID, (Piovesan et al., 2014)).
Figure 1: Architecture of GLARE. Rectangles represent
computation modules, and ovals data/knowledge bases.
Representation Formalism. In the GLARE project,
a GL is represented through the set of actions
composing it. GLARE distinguishes between atomic
and composite actions. Atomic actions can be
regarded as elementary steps in a GL, in the sense
that they do not need a further decomposition into
sub-actions to be executed. Composite actions are
composed by other actions (atomic or composite).
Four different types of atomic actions can be
distinguished in GLARE: work actions, query
actions, decisions and conclusions. Work actions are
basic atomic actions which must be executed on the
patient, and can be described in terms of a set of
attributes, such as name, (textual) description, cost,
time, resources, goals. Query actions are requests of
information, which can be obtained from the outside
world (physicians, Databases, knowledge bases).
Decision actions are specific types of actions
embodying the criteria which can be used to select a
alternative paths in a GL. In particular, diagnostic
decisions are represented as an open set of triples
<diagnosis, parameter, score> (where, in turn, a
parameter is a triple <data, attribute, value>), plus a
threshold to be compared with the different
diagnoses’ scores. On the other hand, therapeutic
decisions are based on a pre-defined set of
parameters: effectiveness, cost, side-effects,
compliance, duration. Finally, conclusions represent
the output of a decision process. Composite actions
are defined in terms of their components, via the
“has-part” relation. Control relations establish which
actions might be executed next and in what order.
We distinguish among four different control
relations: sequence, constrained, alternative and
repetition. The description of sequences usually
involves the definition of the minimum and
maximum delay between actions. Complex temporal
constraints between actions (e.g., overlaps, during)
can be specified using constrained control relations.
In particular, action parallelism can also be
supported through this feature.
Acquisition. GLARE’s acquisition module (CG-AM
in Figure 1) provides expert-physicians with a user-
friendly and easy-to-use tool for acquiring a GL. In
order to achieve these goals, GLARE provides: (i) a
graphical interface, which supports primitives for
drawing the control information within the GL, and
ad hoc windows to acquire the internal properties of
the objects; (ii) facilities for browsing the GL; (iii)
an “intelligent” help and consistency checking
including name and range checking, logical design
criteria checks, and semantics checks concerning the
consistency of temporal constraints in the GL.
Execution. A dedicated module has been developed
to support the execution of a GL on a specific
patient, adopting the “agenda technique” (see
(Anselma et al., 2006)). Basically, though the
“agenda technique”, GLARE is able to identify all
the next actions to be executed in the current GL,
and a window of time during which such actions
have to be executed (according to the GL temporal
constraints).
Testing. GLARE has been already tested
considering different domains, including bladder
cancer, reflux esophagitis, heart failure, and
ischemic stroke. The acquisition of a GL using
GLARE is reasonably fast (e.g., the acquisition of
the GL on heart failure required 3 days).
META-GLARE. In the last years, a new GL
system, META-GLARE, has been designed, on top
of GLARE. Indeed, META-GLARE is a “meta”
system, in that it takes in input a GL representation
formalism, and automatically generates a GL system
to acquire and execute GL expressed in the input
formalism. To test it, an extended formalism has
been used (see (Bottrighi and Terenziani, 2016)). In
the following, we refer to such an extended
formalism as “META-GLARE formalism”. In
particular, META-GLARE formalism extends
GLARE’s one with the possibility of specifying not
only 1:1 arcs (i.e., arcs with just one input action and
one output action), but also 1:n, n:1 and n:n arcs.
Such an additional feature is very useful to easily
model the parallelism between actions.
GLARE and META-GLARE have been
developed in Java, to take advantage of its portability.
HEALTHINF 2018 - 11th International Conference on Health Informatics
210

As a consequence, GLARE can run similarly on any
hardware/operating-system platform.
3 GL ANNOTATIONS
In order to support the coordination of different
healthcare agents during the execution of a GL on a
specific patient, the description of the GL actions
must be extended to consider several additional
aspects. For each one of such aspects, we augment
the representation formalism with an additional
attribute, modelling it. In the following we refer to
such attributes as (action) annotations. First of all,
the possible contexts in which an action can be
executed must be specified.
• Context annotation: it specifies where the
action can be executed (e.g. in-patient care,
community medicine). Observe that a context
is not necessarily a physical place, but it is an
operative environment. For instance,
community medicine can refer to the
patient’s home or to the general practitioner’s
ambulatory. A set of contexts for an action
can be specified, meaning that the action can
be executed in any one of the contexts
specified in the list;
In many practical cases, it is important to
distinguish between the responsible of an action (or
of a whole part of a GL; for instance the head
physician of an hospital department), and the
executor of the action (for instance, a physician or a
nurse of that department). Indeed, to be
“appropriate” a responsible (executor) must have a
proper qualification, and, in some cases, some
specific additional competence (other than the ones
typically held by all the agents having the specified
qualification). To cope with such issues, we further
add six annotations:
• responsible_qualification: it specifies who
can be responsible of the action (e.g.
neurologist, gastroenterologist, …). A list of
qualifications can be specified, meaning that
the responsible must have (at least) one of the
qualifications in the list;
• responsible_competence: it specifies that
the must have specific abilities (e.g. expert in
the alcohol-related disorders management).
Such an attribute is optional. A list of
competences can be specified, meaning that
the responsible must have all the
competences in the list;
• delegate_qualification: it specifies who can
be delegated to manage the action (e.g.
physician, nurse); A list of qualifications can
be specified, meaning that the delegate must
have one of the qualifications in the list;
• delegate_competence (optional): it specifies
that the action can be managed only by agents
with some specific abilities (e.g. alcohol-related
disorders management). A list of competences
can be specified, meaning that the delegate must
have all the competences in the list;
• executor_qualification: it specifies who can
execute the action (e.g. physician, nurse); A list
of qualifications can be specified, meaning that
the executor must have one of the qualifications
in the list;
• executor_competence (optional): it specifies
that the action can be executed only by agents
with some specific abilities (e.g. alcohol-related
disorders management). A list of competences
can be specified, meaning that the executor must
have all the competences in the list;
When a GL is being acquired, we impose that
each action in it is annotated with a specification of
a list of possible contexts and of a list of possible
qualifications of responsibles and executors. This is
mandatory, and the acquisition module is extended
to support the acquisition of such annotations (see
Section 4). On the contrary competence annotations
are optional. In case the competence list is empty, no
specific restriction needs to be applied; otherwise,
only the agents having the required competences are
allowed to be responsible for or to execute the action
at hand.
Example. The action “Brief intervention for
hazardous and harmful drinking” (see action 11 in
Figure 3) in the alcohol-related disorders treatment
GL (Scottish Intercollegiate Guidelines Network,
n.d.) is described as follows:
• resposible_qualification: physician;
• resposible_competence: \
• delegate_qualification: physician;
• delegate_competence: \
• executor_ qualification: physician, nurse;
• executor_competence: \
• context: community medicine, SERT medicine
(SERT is the acronym for “SERvizio per le
Tossicodiopendenze”, an Italian service similar
to the Mental Health Service in U.S.A.), in-
patient care, hospital ambulatory care.
Supporting Multiple Agents in the Execution of Clinical Guidelines
211
In addition, as an independent data structure, we
support the annotation of a whole GL with a set of
continuity constraints. Such constraints are used to
model the fact that, in many practical cases, it is
preferable to assign “homogeneous” sets of actions
in a GL to the same responsible (or, in some cases,
executor). For instance, it might be preferable that
the same neurologist is responsible of all the
neurological activities performed on a given patient,
and that the different EMG examinations of a patient
are executed by the same specialist. Notably,
continuity constraints are interpreted as
“preferential” constraints by our system (see Section
4), but admits violations (e.g., after a period, a
physician may, for any reason, not be able to
continue to treat a given patient).
In the next sections, we will present how
annotations are formalized in our approach, and how
they are treated by META-GLARE.
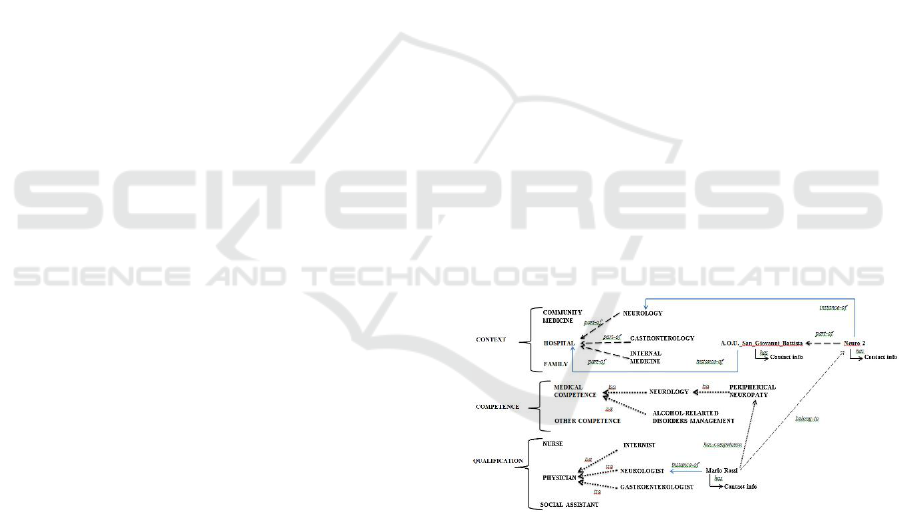
3.1 Basic Ontology
GL annotations can be modeled on the basis of three
taxonomies, and of the relations between them. Part
of the taxonomies and relations are graphically
shown in Figure 2. The ontology of contexts is a
“part-of” taxonomy, in which each context can be
further specified by its components. For instance, in
Figure 2, FAMILY, HOSPITAL and COMMUNITY
MEDICINE are three possible contexts, and
NEUROLOGY, GASTROENTOROLOGY and
INTERNAL MEDICINE are some of the
departments that are part of hospitals. Qualifications
can be modeled through a standard “isa” taxonomy,
in which each qualification can be further refined
(isa relation) by its specializations. For instance, in
Figure 2, Nurse and Physician are two possible
qualifications. In turn, NEUROLOGIST,
GASTROENTEROLOGIST and INTERNIST are
specializations of PHYSICIAN. Analogously, also
competences are modeled by an “isa” taxonomy. For
instance, in Figure 2, (the competence in)
PERIPHERAL NEUROPATHY is a specialization
of (competence in) NEUROLOGY, which is a
specialization of MEDICAL COMPETENCE.
Besides concepts, which denote classes of
entities, the ontology also includes instances,
denoting specific entities. Each instance is connected
to its class through an “instance-of” relation. For
example, in Figure 2, Neuro2 is an instance of
Neurology in Azienda Ospedaliera San Giovanni
Battista (which is an instance of Hospital); Mario
Rossi is an instance of Neurologist (thus, given the
transitivity of the isa relation, Mario Rossi is also an
instance of Physician). It is worth noticing that,
while the entities in the context and qualification
taxonomies have instances, competences do not have
them (they are individual concepts). Besides part-of,
isa and instance-of relations, other relations are
useful to represent our domain. Agents (which are
instances of Qualifications) are related to the
contexts they belong by the belong-to relation.
Additionally, agents may have competences, and
this fact is represented by the has-competence
relation. For instance, in Figure 2, Mario Rossi
belongs to Neuro2, and has specific competence
about Peripheral Neuropathy. Contexts and persons
have contacts (usually phone numbers).
On the other hand, continuity constraints are
simply formalized, for each GL, by an independent
data structure, modeling
(i) the sets of actions which should (preferably)
have the same responsible;
(ii) the sets of actions which should (preferably)
have the same delegate;
(iii) the sets of actions which should (preferably)
have the same executor.
The definition of continuity constraints is a
refinement process. First the user can define the
continuity constraints concerning the responsibles.
Then, within each responsible-level continuity
group, she can further specify continuity groups for
possible delegates. Finally, continuity execution
groups can be defined, within the delegate-level
continuity groups.
Figure 2: Ontology of contexts, qualifications and
competences and their instances.
4 SOFTWARE TOOLS
4.1 Navigation Tool
We have developed a navigation tool to facilitate the
navigation through the above ontology. Such a tool
provides two types of facilities:
(1) schema browsing,
(2) instance browsing.
HEALTHINF 2018 - 11th International Conference on Health Informatics
212

The schema browsing facility allows users to
navigate the ontology (using the part-of and isa
relations) and to find qualifications/contexts/
competences.
The instance browsing facility allows users to
find a specific agent on the basis of the relations
part-of, isa, instance-of, has-competence, belong-to.
For example, it is possible to find an agent on the
basis of a qualification (e.g. Physician), a context
(e.g. Neurology) and, possibly, a competence (e.g.
Peripheral Neuropathy). This facility can give in
output (i) one or more agents (and their contact
information) satisfying the requirements, or (ii) one
or more specific contexts, in which agents having
the required qualification and competences operate.
4.2 Acquisition
We have extended GLARE with an annotation
support, supporting the acquisition of GL
annotations. We have developed a user friendly
Graphical User Interface (GUI). To achieve such a
goal, we enrich the acquisition GUI to provide users
with schema browsing facilities (section 4.1).
Moreover, we have developed an ad-hoc module
to support the definition and the acquisition of
continuity constraints. The user can use this module
to browse the GL and to specify the set of actions in
the GL which belong to a continuity constraints by
selecting such actions in the graphical representation
of the GL.
4.3 Execution Engine
We now extend the execution engine of META-
GLARE to support the distributed execution of GLs.
Specifically, we provide facilities to support the
identification of the responsible(s), of delegate(s)
and of the executor(s) for the next action(s)
according to the GL annotations.
Already in its original version (Terenziani et al.,
2014), META-GLARE execution engine was
adopting an agenda, containing a set of pairs
{(A
1
,T
A1
), …,(A
k
,T
Ak
)} representing the actions to
be executed next (A
1
,…,A
k
), and the window of time
within which the actions have to be executed
(T
A1
, …,T
Ak
). Notably, more than one pair may
appear in the set, to support concurrent execution.
To support the management of responsibilities\
delegations\executions, we add, for each action A in
the agenda, a new data structure Stack
A
, called agent
stack (of A), of the form Stack
A
: <(X
1
, role
1
),
…,(X
k
, role
j
)> where X
i
is a specific agent, and role
h
her role in the management of the action A
(i.e., responsible (R), delegate (D), or executor (E))
1
.
The execution of a GL starts with an
initialization phase. All the initial actions are
inserted into the agenda, together with the window
of time in which they must be executed. Here and in
the following algorithms, we adopt the approach in
[9] to determine the window of time in which each
action has to be executed, on the basis of the
temporal constraints in the GL. For each one of such
actions, and for each actions belonging to the
Responsibility Continuity Group (“RCG” in the
following algorithm) of such actions, the agent stack
is initialized. In such a way the continuity of
resposibles is granted.
Notably the responsibles of the first actions are
predetermined and provided as input to the
execution engine.
The GL execution engines operates as described
by Algorithm 2. For each action A in the agenda, the
GL execution engine starts its execution by sending
the execute message (line 2) to the agent on the top
of the agent stack Stack
A
, asking her to manage the
action A in the time window T
A
according to her
role. In case action A is executed (line 3), A is
removed from the Agenda (line 4). Thus, the
execution engine evaluates the set S of the next
actions in the GL to be executed, using the get_next
function (line 5). Notably, identifying the next
actions which have to be executed during the
execution of a GL is a standard operation (see (Isern
and Moreno, 2008)). For the META-GLARE
approach see (Terenziani et al., 2014).
Each action B belonging to S is pushed onto the
Agenda. Then, in the case that B has not a
responsible (i.e., Stack
B
has not been created yet),
the execution engine asks to the responsible of A
(i.e. the agent stored at the bottom of Stack
A
) to
search a responsible for B and the other actions in its
responsibility continuity group (i.e., RCG(B); line 9)
through the next_responsible? message. Notably,
since we manage continuity groups, the responsible
of an action B in the GL can be already determined
before the time when B is inserted in the agenda
(due to the fact that B belongs to the responsibility
continuity group of another action A already inserted
1
At the time of the execution of an action A, its agent
stack Stack
A
should contain the responsible (bottom of
the stack), a certain number of delegates (zero
delegates in case no delegation has been performed;
more than one delegate are possible, to support
delegation of delegations), and one executor (which
might be also be the last delegate, or the responsible).
Supporting Multiple Agents in the Execution of Clinical Guidelines
213

in the agenda). Finally, the stack of A is deleted
(line 10).
1. Let {(A1,M
A1
), …, (Ak,M
Ak
)} be the set of the
starting actions of GL, and of their
responsibles.
2. put the starting actions (and their time) in
Agenda
3. for each (A, T
A
) in Agenda do
for each B RCG(A) do
initialize(Stack
B
, M
A
, R)
Algorithm 1: Pseudocode of the initialization of the GL
executor engine.
1. for each (A, T
A
) in Agenda do
2. OUTsend (top(Stack
A
),execute(A,T
A
))
3 if (OUT == OK) then
4. Remove A from Agenda
5. S get_next(A)
6. for each B in S do
7. put in Agenda B
8. if B has no responsible then
9. send(next_responsible?
(bottom(Stack
A
), RCG(B))
10. Delete Stack
A
11. else
12. pop(stack of A)
13. goto 2
Algorithm 2: Pseudocode of GL executor engine.
Otherwise, in case A is not executed (i.e. the
agent on the top of StackA rejects its role), a pop on
Stack
A
is performed (line 12). Thus, A remains in
Agenda and the engine executor has to handle it
again sending an execute message to the new top of
the stack of A.
Notably, we support the fact that an agent
accepts the responsibility, the delegation or the
execution of a set of actions (all the actions in a
continuity group) but, later on, stops to operate on
some of the accepted actions. In such a case, the GL
execution engine “goes up” in the agent stack of the
“rejected” actions to find new delegates or
responsibles. Notably, though the current
responsible may decide not to operate any more on
the actions he previously accepted, before “retiring”
she has to find a new responsible for them
4.4 Support to Agents
As described above, we consider three different
categories of agents in GL execution: responsibles,
delegates, and executors. Each of them has different
rights and duties, and for each of them we provide
different supports.
A first set of facilities has the goal of supporting
agents to find proper responsibles, delegates and
executors of one or more GL actions.
The find_responsible function allows an agent to
use the instance browsing facility to find a set of
agents that satisfy the requirements expressed in the
GL annotations. The agent selects one of them as the
responsible for the action A (if A is in a continuity
group, all the actions in the continuity group are
considered). Notably, finding a responsible for a
continuity group of actions does not only involve the
selection of an appropriate (i.e., satisfying the
annotations of the actions) agent in the ontology, but
also to interact with her to know whether this agent
accepts or not (by sending the
accept_responsibility?({(A
1
,T
A1
)…,(A
k
,T
AK
)})
message. In the case the agent gives a positive
response the agent stacks of A
1
, …, A
K
are created,
specifying the new responsible, otherwise the
research for a responsible goes on.
The find_delegate and find_executor functions
operate similarly, supporting the identification of
appropriate delegates (if desired) and executors
(compulsory) to actions (through the use of
accept_delegation? and accept_execution?
messages) and taking into account continuity groups.
In our approach, each agent has the possibility to
receive and send different types of messages,
depending on her current role (responsible, delegate,
executor) in the execution of the GL.
Responsible.
Receipt of an execute(A,T
A
) message. When the
responsible of an action A receives an execute(A,T
A
)
message, it means that it has previously accepted the
responsibility of such an action. However, it may be
the case that, for any reason, at the time when A
must be executed, the responsible wants\needs to
decline (e.g., the responsible of a patient with a
chronic disease may retire, or move away). We
allow her to do so, but with a restriction: the current
responsible is in charge of finding a new responsible
for the action A and the other actions (not executed
yet) in the responsibility continuity group of A
(using the find_responsible function). On the other
hand, if the responsible retains her responsibility,
she still has several options: she can
(i) delegate DCG(A) (i.e., A and all the other
actions in the Delegate Continuity Group of
A), through the find_delegate function
(ii) find an executor for ECG(A) (i.e., A and all
the other actions in the Executor Continuity
Group of A, through the find_executor
function,
(iii) directly execute A herself
HEALTHINF 2018 - 11th International Conference on Health Informatics
214
Receipt of a next_responisble?({(A1,T
A1
),…,
(Ak,T
Ak
)} message.
The current responsible is in charge of
identifying an appropriate responsible for the actions
A
1
… A
k
. To support her in this task, we provide the
find_responsible function, described above.
Receipt of an accept_responsibility?({(A1,T
A1
),…,
(Ak,T
Ak
)} message.
The agent may accept or reject the new
responsibility.
Notably, soon after the acceptance of the
responsibility of a set of actions {(A1,T
A1
),…,
(Ak,T
Ak
)} (a Responsibility Continuity Group of
actions), the new responsible can soon search for
delegates or executors for such actions (considering
their Delegate and Executor Continuity Groups
respectively), using the find_delegate and
find_executor facilities. In such a way, the
mechanism of determining delegates and executors
can proceed in a (partially) asynchronous way with
respect to the actual execution of actions in the GL.
Delegate.
When a delegate receives an execute(A,T
A
)
message, she may decline. Such a situation is
directly managed by the execution engine (see
Algorithm 2), which pops the delegate from Stack
A
and send the execute(A,T
A
) message to the new top
of the stack. On the other hand, if the delegate
retains her role, she can delegate DCG(A), find an
executor for ECG(A) or directly execute A herself.
Additionally, she may accept or reject an
accept_delegation?({(A1,T
A1
),…, (Ak,T
Ak
)} request.
Notably, as in the case of responsibles, soon
after the acceptance of the delegation of a set of
actions {(A1,T
A1
),…, (Ak,T
Ak
)} the new delegate
can soon look for delegates or executors for such
actions.
Executor.
When an executor receives an execute(A,T
A
)
message, she may decline. Such a situation is
directly managed by the execution engine, as
described above (concerning delegates). Otherwise,
she must execute action A within the time interval
T
A
. Additionally, she may accept or reject an
accept_execution?({(A1,T
A1
),…, (Ak,T
Ak
)} request.
5 EXAMPLE
In this section, we present an application of our
approach to a GL for alcohol-related problems
(Scottish Intercollegiate Guidelines Network, n.d.),
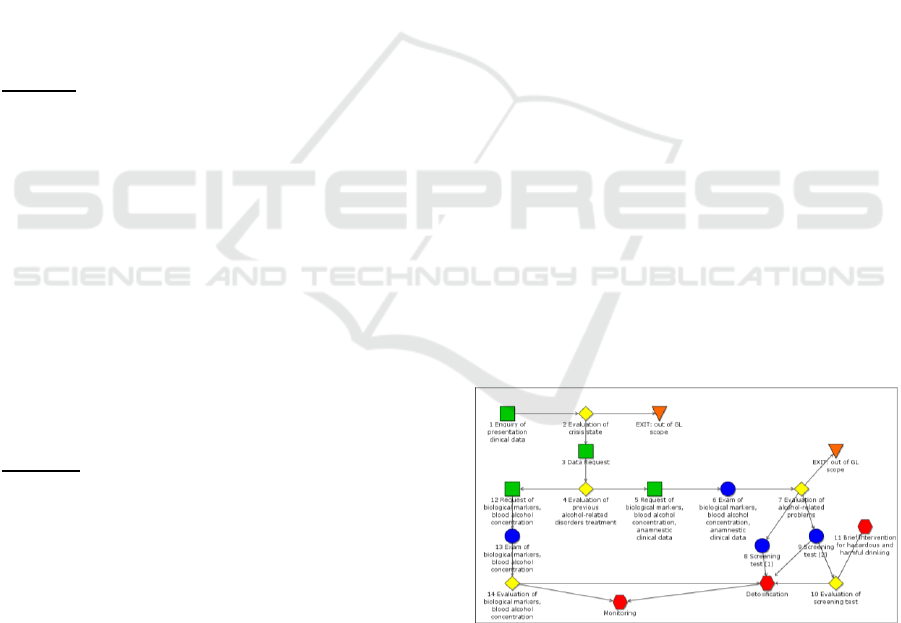
adapted to the Italian context (see Figure 3).
The GL starts with a request of some clinical
data (query action 1), used in the following decision
action (decision action 2), which is meant to
diagnose whether the patient is currently experien-
cing a crisis state. The management of an alcohol-
related crisis is outside the GL scope. If, on the other
hand, the patient is not experiencing a crisis, her
history is collected (query action 3), to distinguish
whether it is the first time that the patient is in
treatment for alcohol-related problems, or not
(decision action 4). New patients require the
collection of biological markers, blood alcohol
concentration and anamnestic data (data request 5
and work action 6), while this data collection is not
needed for patients who were already cared for
alcohol related disorders (data request 12 and work
action 13). For latter patients, an evaluation of
biological markers and blood alcohol concentration
(decision action 14) are required, to decide whether
monitoring them or proceed with a detoxification.
Focusing on new patients, a diagnosis about the
presence of alcohol-related problems is performed
(decision action 7), on the basis of the collected
information. Ifthe patient does not show alcohol-
related problems, the GL execution is ended.
Otherwise, two different treatments can be applied,
depending on the severity of alcohol-related
problems; both start with a screening test (work
actions 8 and 9 respectively). Focusing on patients
who show a mild alcohol-dependence (work action
9), after evaluating the screening test results
(decision action 10), the patient can be selected for a
brief intervention for hazardous and harmful
drinking (composite action 11), which basically
consists in a set of motivational interviews.
Figure 3: META-GLARE graphical representation of part
of the GL on the treatment of alcohol related disorders.
Exploiting the annotation support (see Section 4.2),
we have annotated all the actions defining the
possible qualification(s) of its responsible, delegate
(if any) and executor. Moreover, we have identified
and specified the continuity groups in the GL. In this
specific application, possible values for the attributes
Supporting Multiple Agents in the Execution of Clinical Guidelines
215

Figure 4: The annotations of actions in Figure 3.
in the annotations are the following:
• context: Community medicine (C1), SERT
medicine (C2), in-patient care (C3), hospital
ambulatory care (C4), social services (C5);
• qualification: physician (R1), nurse (R2),
healthcare assistant (R3), social assistant (R4),
laboratory technician (R5).
The treatment continuity criteria demands that all the
actions corresponding to the initial evaluation of the
patient status (actions 1-4) must have a unique
responsible (responsibility continuity group RG1;
see Figure 4), which must be a physician (R1) or a
social assistant (R4). The continuity group RG1 is
further divided into two “subparts”, corresponding to
the two delegation continuity groups DG1 and DG2.
In particular, DG1 corresponds to the identification
of a crisis currently in progress (actions 1 and 2) and
DG2 corresponds to the identification of previous
alcohol-related disorder treatments (actions 3 and 4).
Moreover, due to the execution continuity
constraints, action 1 and action 2 belong to a single
execution continuity group (EG1) and the actions 3
and 4 to a single execution continuity group (EG2).
The executor of the actions in EG1 must be a
physician (R1), or a social assistant (R4), or a nurse
(R4). The actions in EG2 have the same constraints
and the same annotations. After action 4, there are
two alternative treatment paths. One path manages
patients who are treated for alcohol correlated
problems for the first time. Such a path is annotated
with a responsibility continuity group RG2 on the
actions to evaluate the patient’s problem (action 5
and 7) and with a responsibility group RG3 on the
exams needed for such an evaluation (action 6). RG2
and RG3 require a physician (R1) as responsible.
Notably, a continuity group can contain non-
contiguous actions (e.g., RG2 is composed by action
5 and 7 which are not contiguous in the GL).
In the following, we exemplify how META-
GLARE extended execution engine can work on the
above part of the GL. For the sake of simplicity, we
omit the management of temporal constraints.
STEP 0: at the beginning of the execution, the
META-GLARE executor engine identifies action 1
as the first action of the GL, and puts it in the
agenda. We suppose that agent X, who is a social
assistant in the social services SS1, is the responsible
of action 1. Since action 1 belongs to RG1, X is also
the responsible of all the actions belonging to such a
continuity group (i.e., actions 1, 2, 3 and 4). Thus,
the agent stacks of the four actions are created and
initialized with X as responsible. In the initial step,
the stacks for actions 1-4 are therefore initialized as
follows (line 3 of Algorithm 1):
stack
1
: <(X,R)>; stack
2
: <(X,R)>; stack
3
: <(X,R)>;
stack
4
: <(X,R)>.
The agenda of the execution engine contains
only action 1 (and its temporal window, not
considered in the example).
Agenda: <1>.
STEP 1: the executor engine sends an execute
message for each action in the agenda (line 2 on
Algorithm 2). Action 1 is the only action in the
agenda, therefore the executor engine sends a
message to the top element of the stack
1
(i.e., to X)
to perform the execution of action 1. X receives the
execute message and she decides to be the executor
of action 1. Thus, X is put in the stack of action 1 as
executor, and since actions 1 and 2 belong to the
execution continuity group EG1, she is pushed as
executor also onto the stack of action 2. At this
point, the status of agent stacks and the agenda is the
following:
stack
1
: <(X,R),(X,E)>; stack
2
: <(X,R),(X,E)>;
stack
3
: <(X,R)>; stack
4
: <(X,R)>.
Agenda: <1>.
X executes action 1 (returning “OK”, line 2).
Since action 1 has been executed, the executor
engine removes it from the agenda (line 4). Then
(line 5), the next action of the GL is found (i.e.
action 2) and it is put in the agenda (line 7). Action 2
has already a responsible, thus the stack of action 1
is simply deleted.
stack
2
: <(X,R),(X,E)>; stack
3
: <(X,R)>; stack
4
:
<(X,R)>.
Agenda: <2>.
STEP 2: the above procedure is similarly repeated
for action 2 in the Agenda. We suppose that, after
receiving the message, X, who is registered as
executor of action 2, executes it, deciding that
patient is not experiencing a crisis. Thus, action 3 is
HEALTHINF 2018 - 11th International Conference on Health Informatics
216

identified as next action and put in the agenda. Also
in this case, action 3 has its responsible already
defined (i.e. X).
stack
3
: <(X,R)>; stack
4
: <(X,R)>.
Agenda: <3>.
STEP 3: Action 3 is the only action in the Agenda
and is managed sending an execute message to its
responsible X (i.e. X is on the top of stack
3
).
However, in this case we suppose that X decides to
delegate such an action. Exploiting the instance
browsing facility of our navigation tool (see Section
4.1), X searches for an agent satisfying the
requirements (i.e. a social assistant or a physician in
her context). Through the navigation tool, X is
provided with a list of possible agents. She selects a
preferred one from the list and ask for acceptance,
until she receives a positive reply. We suppose that
(possibly after some negative replies of social
assistants) the social assistant Y accepts. Since
actions 3 and 4 belong to the same delegation
continuity group (i.e. DG2), Y is also delegated for
action 4.
stack
3
: <(X,R),(Y,D)>; stack
4
: <(X,R),(Y,D)>.
Agenda: <3>.
Y decides to be the executor of action 3. Since
actions 3 and 4 belong to the same execution
continuity group EG2, Y is nominated also as the
executor of action 4 and she is put in the two stacks
as executor.
stack
3
: <(X,R),(Y,D),(Y,E)>;
stack
4
: <(X,R),(Y,D),(Y,E)>.
Agenda: <3>.
Y executes action 3 and action 4 is put in the
agenda as next action.
stack
4
: <(X,R),(Y,D),(Y,E)>.
Agenda: <3>.
STEP 4: the engine takes action 4 from the agenda,
then it notifies to Y (i.e. Y is on the top of stack4)
that action 4 has to be executed. Exploiting the
instance browsing facility Y identifies the agent W
as executor of action 4. W satisfies the action
annotations (i.e. she is a nurse and operate is SS1).
W accepts the assignments and she is put on stack
4
as executor.
stack
4
: <(X,R),(Y,D),(W,E)>.
Agenda: <4>.
W executes action 4 and identifies that the
patient is in treatment for alcohol-related problems
for the first time (i.e. action 5 is the next action).
Thus, action 5 is put in the agenda. Since action 5
has not yet a responsible (line 8), the system asks to
X, the responsible of action 4 (i.e., the element at the
bottom of the stack
4
) to find a responsible for the
next action. X must find a responsible who is a
physician (R1) and works either in a Community
medicine (C1) or in a SERT medicine (C2) or in-
patient care (C3) or in a hospital ambulatory care
(C4). Exploiting the instance browsing facilities, X
finds a physician Z, who works in the community
medicine CM2, and asks her for the responsibility of
action 5. Z accepts the responsibility and, since
action 7 belongs to the same responsibility
continuity group (RG2), Z is nominated as
responsible of both the actions in RG2.
Stack
5
: <(Z,R)>; Stack
7
: <(Z,R)>.
Agenda: <5>.
Then, the GL execution goes on in a similar way.
6 COMPARISONS AND
CONCLUSIONS
In this paper, we describe the first computerized
approach to GLs supporting many different crucial
issues for the distributed and coordinated execution
of GLs by multiple healthcare agents. Our
approachgrants for the continuity of the treatment of
patients (i.e., the fact that, in any moment during the
GL execution, there is always a responsible for each
one of the next actions to be executed on the patient)
through a support to the identification of the
responsibles, executors and contexts of execution of
the next actions. The extensions to the GL formalism
(Section 3) and to the GL execution engine and the
facilities in Section 4 fully achieve such a
challenging goal. Indeed, they support action
contextualization and (through the definition of
Continuity Groups) treatment continuity. They
provide support in the identification of responsibles,
delegates and executors of actions having the
required qualification, and the overall approach
grants that, whenever an action has to be executed,
there is always a current responsible for it, and
possibly delegates and executors (notably, if an
executor has not been already identified, the current
responsible is urged to do so). Notably, also the
temporal window in which actions must be executed
(given the temporal constraints in the GL) is taken
into account. Last, but not least, delegation is
supported, to enable the current responsible to take
advantage of the help of other healthcare agents.
Notably, we have described our approach on the
basis of METAGLARE, but it is worth stressing that
our methodology is completely general and system\
application-independent (i.e. other GL system can be
extended applying our approach).
Supporting Multiple Agents in the Execution of Clinical Guidelines
217

While in the literature there is no other approach
to computerized GL that has provided a support
considering all the aspects above, several approaches
have faced at least few of them.
Fox’s group proposed an extension of the
PROforma representation formalism (Sutton and
Fox, 2003) to specify who will execute an action.
However their goal is not the one of managing
agents interactions in different contexts: they exploit
agent information for better contextualizing GLs
taking into account local human resources, and for
flexibly adjusting them through delegation.
(Leonardi et al., 2007) propose a workflow-
based solution to manage chronic patients over long
time periods. In particular, the approach is meant to
allow patients to obtain the necessary health care
services by accessing different locations/
organizations, which can properly exchange/
communicate health data when needed. Their goal
(i.e. support cooperative work between different
healthcare organizations) is quite similar to ours;
moreover, the authors model organizational
knowledge (i.e. qualifications, resources etc.) by
means of ontologies – as we do. However, their
approach is not as flexible as ours, because
interactions between agents, and allocations of the
next action to a specific responsible, are strictly
predetermined by a contract and can not be
determined dynamically during the GL execution.
On the other hand, we allow the responsible of the
current action to navigate the ontology, and to
dynamically and freely identify the responsible
and\or the executor of the next action on the basis of
the available knowledge and constraints. Moreover,
they do not support delegation.
(Sánchez et al., 2011) propose an ontology-
driven execution of GLs. Their approach relies on a
multi-agent system, where every entity (i.e. actor or
structure) in a medical centre is represent by one
specific agent and every GL action is characterized
by hasResposible relation with one agent or a set of
agents. Their main contribution regards the
delegation issue in a supervised fashion and the
automation of the coordination internal activities
using a medical-organisational ontology. Since their
approach is meant to be applied within a specific
medical centre, it is focused on supporting
interaction in a distributed environment, where the
coordination between actors can not be managed
automatically.
Grando et al (2010) formalize cooperative work
in GL execution (but not distributed executions
across different contexts). The main issue they deal
with is delegation of tasks to specific members of
the working team, on the basis of their competences,
paying particular attention to responsibilities for
enacting a service, and for handling exceptions.
Specifically, they extend the design pattern
framework introducing the types role (qualification
in our approach) and actor, and a set of relations
between key concepts. Since actors have roles and
competences, they recall our notion of agent.
Therefore, they rely on concepts which are similar to
our annotation information, even if we resort to a
different mean for formalizing them (i.e. an
ontology). However, Grando et al. do not consider
contexts: in this sense, their approach is more
limited than ours, and not straightforwardly
extendable to deal also with distributed (and not just
cooperative) GL executions. Moreover, we provide
a set of software tools to manage the ontology in our
formalization.
(Wilk et al., 2015) propose a framework to
support GL execution, in which interdisciplinary
healthcare teams are involved. They define three
classes of agents (i.e. team manager, practitioner
assistant, patient representative), but they classes do
not correspond to qualification. They have the
concept of capability that is similar to competence.
They annotate actions, but their annotations are only
related to the capability requirements. They have
only the concept of executor of an action and not of
responsible. Moreover, they have the concept of
team, i.e. a set of agents (defined using a hybrid
approach) who managed the execution and are
coordinated by the team manager, i.e. the response-
ble of execution for the whole GL. The identification
of executor of an action is not general as ours: only
the team manager can identify the executors and first
she has to consider the agents in the team. Only in
the case than there is not any suitable and available
agents in the team, she can search an external agent
to execute the action and can add it to the team.
Notably, this is a clear limitation, since many GLs
can not have a single responsible. Considering also
the absence of context, their approach is not adapt to
deal with distributed executions.
(Bottrighi et al., 2013) is the approach most
closely related to the one we present in this paper. In
particular, in such an approach, actions are annotated
(coloured, in the terminology in (Bottrighi et al.,
2013)) with context, and qualification and
competences for the responsible, and different forms
of support are proposed to acquire and query
annotations, and to execute coloured GLs. Notably,
the approach we propose deeply extends the one in
(Bottrighi et al., 2013) to consider three significant
aspects, neglected in (Bottrighi et al., 2013):
HEALTHINF 2018 - 11th International Conference on Health Informatics
218

(1) we support the distinction between the
responsibles of actions, and their executors;
we support the delegation of responsibility
(2) we represent and manage continuity
constraints
(3) we manage the execution of GLs expressed
in META-GLARE formalism (while
(Bottrighi et al., 2013) considered only
GLARE formalism), thus also supporting
n:1, 1:n, and n:m arcs (i.e., concurrency in
the GL execution).
ACKNOWLEDGEMENTS
The authors are very grateful to Prof. Gianpaolo
Molino and Dr. Mauro Torchio of Azienda
Ospedaliera San Giovanni Battista in Turin (one of
the largest hospitals in Italy) for their constant
support, and for their help in the definition of the
case study.
REFERENCES
Anselma, L., Terenziani, P., Montani, S., Bottrighi, A.,
2006. Towards a comprehensive treatment of repeti-
tions, periodicity and temporal constraints in clinical
guidelines. Artif. Intell. Med., Temporal Representa-
tion and Reasoning in Medicine 38, 171–195.
Bottrighi, A., Giordano, L., Molino, G., Montani, S.,
Terenziani, P., Torchio, M., 2010. Adopting model
checking techniques for clinical guidelines
verification. Artif. Intell. Med. 48, 1–19.
Bottrighi, A., Molino, G., Montani, S., Terenziani, P.,
Torchio, M., 2013. Supporting a distributed execution
of clinical guidelines. Comput. Methods Programs
Biomed. 112, 200–210.
Bottrighi, A., Terenziani, P., 2016. META-GLARE: A
meta-system for defining your own computer
interpretable guideline system—Architecture and
acquisition. Artif. Intell. Med. 72, 22–41.
Field, M. J., Lohr, K. N. (Eds.), 1990. Clinical Practice
Guidelines: Directions for a New Program. National
Academies Press (US), Washington (DC).
Fridsma, D. B., 2001. Special Issue on Workflow
Management and Clinical Guidelines. J. Am. Med.
Inform. Assoc. 22, 1–80.
Gordon, C., Christensen, J. P. (Eds.), 1995. Health
Telematics for Clinical Guidelines and Protocols. IOS
Press, Amsterdam.
Grando, A., Peleg, M., Glasspool, D., 2010. Goal-based
design pattern for delegation of work in health care
teams. Stud. Health Technol. Inform. 160, 299–303.
Isern, D., Moreno, A., 2016. A Systematic Literature
Review of Agents Applied in Healthcare. J. Med. Syst.
40.
Isern, D., Moreno, A., 2008. Computer-based execution of
clinical guidelines: A review. Int. J. Med. Inf. 77, 787–
808.
Leonardi, G., Panzarasa, S., Quaglini, S., Stefanelli, M.,
van der Aalst, W.M.P., 2007. Interacting agents
through a web-based health serviceflow management
system. J. Biomed. Inform. 40, 486–499.
Montani, S., Terenziani, P., 2006. Exploiting decision
theory concepts within clinical guideline systems:
Toward a general approach. Int J Intell Syst 21, 585–
599.
Montani, S., Terenziani, P., Bottrighi, A., 2005. Exploiting
decision theory for supporting therapy selection in
computerized clinical guidelines. Lect. Notes Comput.
Sci. Subser. Lect. Notes Artif. Intell. Lect. Notes
Bioinforma. 3581 LNAI, 136–140.
Peleg, M., 2013. Computer-interpretable clinical guide-
lines: A methodological review. J. Biomed. Inform.
46, 744–763.
Piovesan, L., Molino, G., Terenziani, P., 2014. Supporting
Physicians in the Detection of the Interactions between
Treatments of Co-Morbid Patients, in: Healthcare
Informatics and Analytics: Emerging Issues and
Trends. IGI Global, pp. 165–193.
Sánchez, D., Isern, D., Rodríguez-Rozas, Á., Moreno, A.,
2011. Agent-based platform to support the execution
of parallel tasks. Expert Syst. Appl. 38, 6644–6656. y.
Scottish Intercollegiate Guidelines Network, n.d.
Management of harmful drinking and alcohol
dependence in primary care [WWW Document]. URL
http://www.sign.ac.uk/guidelines/fulltext/74/index.htm
l (last accessed 05.10.17).
Sutton, D.R., Fox, J., 2003. The Syntax and Semantics of
the PROforma Guideline Modeling Language. J. Am.
Med. Inform. Assoc. JAMIA 10, 433–443.
Terenziani, P., Bottrighi, A., Rubrichi, S., 2014. META-
GLARE: a meta-system for defining your own CIG
system: Architecture and Acquisition, in: KR4HC. pp.
92–107.
Terenziani, P., Montani, S., Bottrighi, A., Molino, G.,
Torchio, M., 2008. Applying artificial intelligence to
clinical guidelines: the GLARE approach. Stud. Health
Technol. Inform. 139, 273–282.
Terenziani, P., Montani, S., Bottrighi, A., Torchio, M.,
Molino, G., 2002. Supporting physicians in taking
decisions in clinical guidelines: the GLARE“ what if”
facility. Proc. AMIA Symp. 772.
Terenziani, P., Montani, S., Bottrighi, A., Torchio, M.,
Molino, G., Correndo, G., 2004. A context-adaptable
approach to clinical guidelines. Stud. Health Technol.
Inform. 107, 169–173.
Wilk, S., Astaraky, D., Michalowski, W., Amyot, D., Li,
R., Kuziemsky, C., Andreev, P., 2015. MET4:
Supporting Workflow Execution for Interdisciplinary
Healthcare Teams, in: Fournier, F., Mendling, J.
(Eds.), Business Process Management Workshops.
Springer International Publishing, Cham, pp. 40–52.
Supporting Multiple Agents in the Execution of Clinical Guidelines
219
