
Trust Factors in Healthcare Technology: A Healthcare Professional
Perspective
Raja Manzar Abbas
1
, Noel Carroll
2
, Ita Richardson
1,3
and Sarah Beecham
1
1
Lero - the Irish Software Research Centre, University of Limerick, Limerick, Ireland
2
Lero - the Irish Software Research Centre, National University of Ireland Galway, Galway, Ireland
3
HRI- Health Research Institute, University of Limerick, Limerick, Ireland
Keywords: Trust, Healthcare Technology, Technology Adoption, Healthcare Professionals, Mapping Study.
Abstract: Being able to trust technology is of vital importance to its potential users. This is particularly true within the
healthcare sector where lives increasingly depend on the correct application of technology to support
clinical decision-making. Despite the risk posed by improper use of technology in the healthcare domain,
there is a lack of research that examines why healthcare professionals trust healthcare technology.
Therefore, there is little evidence regarding the key trust facilitators and barriers. In this paper, we
investigate the concept of trust within a healthcare technology context. We conducted a systematic mapping
study to identify relevant trust facilitators and barriers in published work in well-known bibliographic
databases. Our results present a synthesis of 47 studies that describe trust factors that healthcare
professionals associate with healthcare technology. Facilitators include compatibility and perceived systems
usefulness, while barriers include privacy concerns and lack of knowledge. We conclude that HCT trust is
complex, multi-dimensional, and influenced by a variety of factors at individual and organizational levels.
1 INTRODUCTION
Healthcare technology (HCT) is defined by the
World Health Organization as the “application of
organized knowledge and skills in the form of
devices, medicines, vaccines, procedures and
systems developed to solve a health problem and
improve quality of lives” (WHO, 2017). This
includes the pharmaceuticals, devices, procedures
and organizational systems used in healthcare. HCT
has the potential to address many of the challenges
that healthcare is currently confronting. For
example, HCT improves information management,
access to health services, quality and safety of care,
continuity of services, and costs containment (Miles
and Asbridge, 2014).
Due to the growth in population and shift in
demographics, there is considerable pressure on
global healthcare systems to provide an effective and
efficient service. Shojania et al. (2016) attribute
deaths of 251,454 people in US hospitals per year to
medical errors, the third-leading cause of death in
the USA. The Institute of Medicine study estimated
the cost of nonfatal medical errors is between $17
billion and $19 billion each year, and that between
2.9% and 3.7% of all patients admitted suffer some
type of injury as a result of medical mismanagement.
As a result, there is a growing focus on HCT support
for healthcare services which has given rise to a
comprehensive sociotechnical model for managing
healthcare through technology (Carroll, 2016).
Technological advances have encouraged the
development of new technologies that drive
connectivity across the healthcare sector, for example,
systems that manage care using just-in-time
information (Leroy et al., 2014).
Research suggests that patients also want
clinicians to use HCT (Car and Sheikh, 2004). With
increasing global computerisation, HCT is expected
to become part of healthcare professional practice.
Nevertheless, it appears that several HCT applications
remain underused by healthcare professionals (Berner
et al., 2005, Brooks and Menachemi, 2006).
Healthcare organizations, particularly physician
practices, are often used as examples for lagging
behind in trusting and adopting these technologies
(Yarbrough and Smith, 2007). Human and
organizational factors have frequently been identified
as the main causes of HCT implementation and usage
failure (Pagliari, 2005, Carroll et al., 2016).
454
Abbas, R., Carroll, N., Richardson, I. and Beecham, S.
Trust Factors in Healthcare Technology: A Healthcare Professional Perspective.
DOI: 10.5220/0006594204540462
In Proceedings of the 11th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2018) - Volume 5: HEALTHINF, pages 454-462
ISBN: 978-989-758-281-3
Copyright © 2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

1.1 Problem Statement
Although barriers and facilitators of trust in HCT
settings are described to a certain extent in the
literature, only a few studies have systematically
reviewed factors influencing trust in different types
of HCT (Yarbrough and Smith, 2007, Anderson,
2007, Kukafka et al., 2003, Yusof et al., 2007,
Gagnon et al., 2012). Furthermore, there is no
consensus on the categorisation of barriers and
facilitators related to trust in HCT since most of
these reviews have not been from a healthcare
professional prospective.
The study in this paper systematically maps the
key trust factors that are positively (facilitators) or
negatively (barriers) associated with HCT used in
clinical settings by healthcare professionals.
Furthermore, this mapping allows us to highlight the
differences and similarities of trust factors between
different HCT types. This study serves as an initial
basis for developing a fine-grained understanding of
what comprises ‘trust’ in HCT from a healthcare
professional’s view-point. Such information can be
crucial to design and implementation strategies that
take end-users’ concerns about trust into account and
thus, have a higher chance of being accepted or
implemented.
The remainder of the paper is organized as
follows: Section 2 provides a brief overview of trust
and different trust definitions in the healthcare and
computer science literature. Section 3 describes our
methodology adopted for this study. Section 4
describes our findings and results from the literature.
Section 5 presents the discussion from the findings
and results. Finally, Section 6 presents the
conclusion, limitations and future research
opportunities.
2 OVERVIEW OF TRUST
The ultimate goal of technology is to support end-
users in accomplishing their tasks in a convenient
and efficient manner. However, the literature
suggests a loss of productivity while using HCT and
this leads to a lack of trust in the HCT (Van Velsen
et al., 2016).
Trust is generally seen as an important
antecedent of the acceptance, use of, and loyalty
towards technology (Wu and Chen, 2005, Bélanger
and Carter, 2008, van Velsen et al., 2015). This is
also the case for HCT, where trust has been found to
be an important antecedent of patient acceptance
(Park et al., 2011), patients’ and healthy persons’
thoughts on the usefulness of a personal health
record (Cocosila and Archer, 2014), and physicians’
intention to use HCT for rehabilitation care (Wu et
al., 2008).
Trust is investigated in many research fields,
such as computer science, economics, politics,
sociology and philosophy (Grandison and Sloman,
2000, Jøsang et al., 2007, Misztal, 2013). However,
there is no agreement regarding the definition and
properties of trust (Gollmann, 2006, Massa, 2007,
Raya et al., 2008). According to the literature, trust
is difficult to define, convey, measure or specify.
Michael et al. (2002) explain that ‘trust is a term
with many meanings,’ and this is supported by a
large number of definitions proposed in the
literature. Almenárez et al. (2004) define trust as the
belief that an entity has about another entity, from
past experiences, knowledge about the entity's nature
and/or recommendations from trusted entities.
Similarly, Robinson (1996) indicates that trust is
one's expectations, assumptions or beliefs about the
likelihood that another's future actions will be
beneficial, favourable or at least not detrimental to
one's interests. A more ‘common sense’ form of trust
is derived from Alford (2004) who explains that to
trust someone is to be confident that in a situation
where you are vulnerable, one will be disposed to
act benignly towards you.
Trust is also defined in different ways in the
same research field, such as in computer science
(Jøsang et al., 2007, Raya et al., 2008). For instance,
Massa (2007) defines trust as the judgment
expressed by one user about another user, often
directly and explicitly, sometimes indirectly through
an evaluation of artefacts produced by that user or
their activity on the system. Reliability trust is
defined as the subjective probability by which an
individual expects that another individual perform a
given action on which its welfare depends (Jøsang et
al., 2007).
Trust is a key factor in the delivery of healthcare,
high levels of provider/patient trust is conducive to
more effective healthcare (Hall et al., 2002). Trust in
healthcare can be seen as a three-part relationship
between patient (truster), provider or organization
(trustee), and the specific context of delivering
healthcare (technology).
There are various definitions of trust in computer
science and healthcare that may lead to a confusion
about trust in the context of technology (Gollmann,
2006). Since, our focus is on HCT, we follow the
trust definition in McKnight et al. (2002) where trust
in the technology is defined as an individual’s belief
that using a specific technology is safe and secure.
Trust Factors in Healthcare Technology: A Healthcare Professional Perspective
455
In the same way, Krishna and Maarof (2002) explain
that trust is the firm belief in the competence of an
entity to act dependably, securely and reliably within
a specified context.
3 METHOD
In the research literature, we examined the concept
of trust in HCT, how the technology is accepted, and
what is the criteria for its use. We have employed
mapping study guidelines presented by Petersen et
al. (2015). Our motivation to undertake a mapping
study is to synthesize evidence, and bring about
some structure to this research area - HCT trust
factors demonstrated by healthcare professionals.
Considering the broad nature of technological use in
healthcare, we argue that stakeholders need to have a
set of criteria by which they can assess the level of
trustworthiness of a given technology. We present
evidence related to trust facilitators and barriers
based on the frequency of them occurring in the
literature. In this study, we acknowledge that trust is
often considered an elusive term. Therefore, in
order to ensure that we captured various nuances
related to trust in HCT, we have included terms
related to the adoption, usage and acceptance of
HCT. This builds on our knowledge that the
literature uses these terms interchangeably when
alluding to the concept of trust.
3.1 Eligibility Criteria
To account for the different types of studies on trust
factors for HCT by healthcare professionals, a mixed
study review was conducted. This can be
conceptualized as a mixed methods research study
where data consists of the text of papers reporting
primary qualitative and quantitative studies in
addition to mixed methods studies (Pluye et al.,
2009).
3.2 Search Strategy
We searched seven well-established digital
databases (CINAHL, Embase, IEEE Xplore, Science
Direct, Scopus, Springer Link and Web of Science)
for relevant publications. For expediency, we ran
one search using the following search string (or
variants of the search string to fit the various
databases):
("Health care" OR Healthcare) AND (Trust* OR
Accept* OR Adopt* OR Usage) AND (Software OR
“Information Technology” OR “Information
System”).
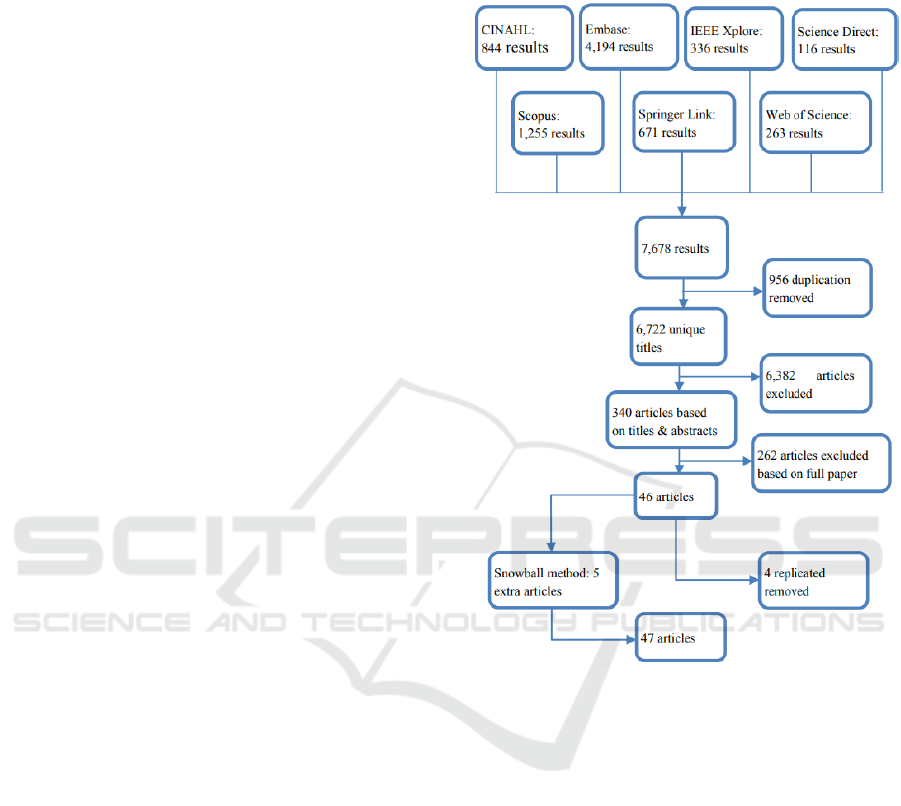
The search process and result is in Figure 1.
Figure 1: Study selection flow diagram.
3.3 Article Selection
Titles and abstracts were screened by one of the
authors [R1]. Out of the total 7,678 studies, 956
studies were removed by EndNote software as they
were duplicated. From 6,722 studies, 340 full
articles were selected by R1 through applying the
inclusion exclusion criteria shown in Table 1. For
validation purpose, a random 44 studies out of 6722
were selected and sent to two authors [R2] [R3].
Where there were conflicts with inclusion, this
discrepancy was resolved by arbitration and mutual
consent. In next step, inclusion exclusion criteria
were applied by R1 on the remaining 340 articles.
This resulted in 294 articles being excluded. For
validation of the excluded articles, a randomly
chosen 40 studies from these 294 articles were
reviewed by R2, and agreement was observed. Out
HEALTHINF 2018 - 11th International Conference on Health Informatics
456
of 46 included articles, four were found to be
replicated and were removed.
In addition, using the snowball method, references
from included articles were checked to ensure
inclusion of relevant studies which may have been
overlooked. Five articles were added resulting in a
total of 47 articles presented in this study.
Table 1: Inclusion (I) and Exclusion (E) criteria.
I: Original and peer-reviewed research written in English;
I: Qualitative, quantitative or mixed methods research;
I: Study on healthcare technology;
I: Study containing healthcare professional prospective;
I: Suggests/ recommends or contains/defines at least one trust
attribute for healthcare technology;
I: Describes factors that influence trust or the intention to use
technology in healthcare practice.
E: White or grey literature
E: Presents research noted in a prior/subsequent paper
3.4 Synthesis
A narrative synthesis, the process of synthesising
primary studies to explore heterogeneity
descriptively rather than statistically (Mays et al.,
2005), was performed to summarize the evidence.
We abstracted the trust factors into three categories:
HCT factors or characteristics of the HCT,
Individual factors or healthcare professional
characteristics and Organizational factors.
4 MAPPING RESULTS
This systematic mixed mapping study presents an
integrative and comprehensive structure of trust
factors and barriers associated with HCT for
healthcare professionals. Additionally, we present
their relative importance for specific types of HCT
used in healthcare. In this mapping study, 47 papers
presented 57 trust facilitators and 48 trust barriers in
HCT demonstrated by healthcare professionals.
Table 2 shows different types of HCT throughout
the literature and categorizes them into 8 specific
types of HCT based on their characteristics. Most
discussed HCT were Information Systems
(including; online databases, electronic guidelines,
information technology, electronic appointment
system and computer systems), Telemedicine
(including; smartphones, m-health, mobile health
systems, tele-health and e-health), Electronic
Records (including; medical/ health/ patient record,
health information exchange, electronically
mediated services and electronic logistics
information system), Wearable Devices, Evidence-
based Medicine, Adverse Event Reporting
System, Multi-agent System and Computerised
Medical Diagnosis Systems. Tables 3 and 4 present
trust facilitators and trust barriers most frequently
discussed in the literature. Studies are referenced in
our associated technical report (Abbas et al., 2017).
There are differences and similarities between trust
factors associated with each type of HCT. Perceived
system usefulness is a consistent factor across all
types of HCT, but its importance varied according to
the technology. Security issues and privacy concerns
are the most prominent trust barriers.
Table 2: Healthcare Technology within studies.
Type of Healthcare
Study reference number
Information System (IS)
S2,S3, S8, S11, S20, S25,
S33, S34, S35, S36, S37,
S39, S46, S47
Telemedicine (TM)
S7, S10, S12, S17, S19,
S26, S30, S31, S40, S43,
S45
Electronic Record (ER)
S2, S4, S6, S9, S13, S14,
S15, S18, S21, S22, S23,
S32, S41, S44
Wearable Devices (WD)
S24, S28
Evidence‐Based Medicine
(EBM)
S1, S16, S29
Adverse Event Reporting
System (AERS)
S5
Multi-Agent Systems
(MAS)
S38
Computerised Medical
Diagnosing System
(CMDS)
S29
5 DISCUSSION
Various types of factors (technological, human, and
organizational) influence the level of HCT trust by
healthcare professionals. Factors facilitating HCT
trust tend to be mostly related to the perception of
the characteristics of the specific HCT and to
organizational aspects. Barriers are also related to
HCT characteristics, and are found in each of the
individual, professional, and organizational levels.
Some of the trust factors identified are ‘multilevel’
since they could affect more than one level (e.g. ease
Trust Factors in Healthcare Technology: A Healthcare Professional Perspective
457

Table 3: Trust facilitators.
Types of Trust
Factors
Trust Facilitators
IS
TM
ER
WD
EBM
AERS
MAS
CMDS
HCT factors or
characteristics
of the HCT
Compatibility
3
×
1
1
×
×
1
×
Security
1
2
2
×
1
×
×
×
Reliability
2
2
2
×
1
×
×
×
Functionality
3
3
2
×
1
×
1
×
Usability
1
3
1
×
×
×
×
×
Individual factors or
healthcare
professional
characteristics
Knowledge
2
2
4
×
2
×
×
1
Positive attitude towards usage
3
×
3
×
×
×
×
1
Perceived system usefulness
17
4
14
3
1
3
×
1
Organizational factors
Training and technical support
3
×
4
×
1
3
×
×
Table 4: Trust barriers.
Types of Trust
Factors
Trust Barriers
IS
TM
ER
WD
EBM
AERS
MAS
CMDS
HCT factors or
characteristics
of the HCT
Privacy concerns
4
5
3
2
×
×
×
×
Security issues
2
5
5
1
1
×
×
×
Lack of efficiency
2
2
1
×
1
×
×
×
Cost issues
3
1
7
×
×
×
×
×
Poor quality
1
2
2
1
×
×
×
×
Design & technical concerns
2
1
3
1
1
×
×
×
Individual factors
or healthcare
professional
characteristics
Lack of knowledge
3
1
4
×
4
×
×
×
Negative attitude towards usage
1
1
1
×
1
2
×
×
Perceived risks of usage
3
2
3
1
1
×
1
×
Task complexity
1
3
2
×
×
×
×
×
Organizational
factors
Poor training and technical
support
2
2
2
×
1
×
×
×
Governance/regulatory
compliance and policies
1
2
3
×
1
×
×
×
of use can be seen as a characteristic of the HCT but
is also related to familiarity with HCT at the
individual level). Interestingly, they are described as
a facilitator in one level, but a barrier in another
level indicating the importance of context.
5.2 HCT Factors
Compatibility is a trust facilitator within the
characteristics of HCT category which is discussed
six times in the literature. S37: Hung et al. (2014)
defined compatibility as the degree to which the
system is consistent with [nurses'] work practices or
preferences. Determining whether HCT is consistent
is an important trust factor because its function has
been specifically updated and modified to meet the
current needs. When the user sees that a particular
HCT is compatible with their work practice or style,
then they start to trust the technology or see the
relative advantage of using it.
Reliability is also discussed as a crucial trust
facilitator. S45: Van Velsen et al. (2016) discussed
trust in a rehabilitation portal technology, which was
mainly determined by its reliability. They defined
reliability for the rehabilitation portal technology as:
“That it works properly; is not constantly offline. But
also scientifically reliable.”
S14: Ross et al. (2010) expressed functionality as
a trust facilitator for HCT as Electronic Medical
Record (EMR) functionality including storage,
retrieval of test results, dictated notes, electronic
prescribing, shared medication and allergy lists
increases motivation to use and trust the system.
HEALTHINF 2018 - 11th International Conference on Health Informatics
458

Usability is explained by S45: Van Velsen et al.
(2016) as a set of attributes that bear on the effort
needed for use, and on the individual assessment of
such use, by a stated or implied set of users.
Usability has previously been identified as a pivotal
part of trust in e-services for the healthcare
professional. It is also identified as an important
antecedent for creating trust by a physician in HCT.
One of the most discussed trust barriers is the
privacy concern that has been discussed 14 times in
the literature. S13: Hsieh (2015) describes this as the
potential loss of confidential patient data in EMR
exchange systems leading towards low trust by the
healthcare professional in the system.
Another highly cited trust barrier is cost and
issues related with cost. S14: Ross et al. (2010)
describe some practices which identified capital
costs, such as installing and supporting new
computers and upgraded networking in the practice,
as a significant barrier to healthcare exchange use.
Lack of efficiency and poor quality has been
discussed regularly in the literature. Poor technology
quality is one of the factors defined by S9: Egea and
González (2011) for clinician’s resistance to use and
trust technology. They explain, “a physician who
uses telemedicine is concerned by the quality of
patient’s care which causes distrust about the
telemedicine”.
‘Multilevel’ influencing factors include security
S13: Hsieh (2015) explain that physicians’
intentions to use the system are based on the
importance of implementing security measures.
Security requirements, such as authentication, data
integrity, and encryption increases trust beliefs
among physicians. Where the integrity of healthcare
data – especially patient identifiable information is
not assured, it creates distrust by physicians.
5.2 Individual Factors
In the context of trust factors for healthcare
professionals, perception of the benefits of the
technology is the most frequent trust facilitator
factor encountered in the study, discussed 43 times.
Perceived usefulness, perceived ease of use/
complexity, intention to use and perceived
behavioural control/facilitating conditions all fall
under the umbrella of usefulness of the system.
Behavioural intention to use is defined as the
individual's interest in using the system for future
work. Perceived usefulness is defined as the degree
to which a person believes that using a particular
system would enhance his or her job performance,
while perceived ease of use is defined as the degree
to which a person believes that using a particular
system would be free of effort S5: (Wu et al., 2008).
Successful cases of HCT trust are usually
characterised by a clear understanding of the
benefits of the innovation by healthcare
professionals. Perceived ease of use is a strong and
significant determinant of [nurses’] intention to use
and trust electronic health records and also
influences the perceived usefulness of the system
S37: (Hung et al., 2014).
Perceived risks of usage and task complexity are
also trust barriers. Perceived risk is explained as the
uncertainty of a user [physician] or risks associated
with the usage of information system S14: (Hsieh,
2015). They have explained that the [physicians’]
perceived risk has a negative effect on their trust and
intention to use an electronic medical record
exchange system as perceived risk increases the
anticipation of negative outcomes, leading to an
unfavourable attitude that typically results in a
negative effect on a user's trust. S15: Saleem et al.
(2009) explain nine instances where complexity of a
task was not supported by the routine workflow or
computerized patient record system functionality,
resulting in the distrust of the system.
‘Multilevel’ influencing factors include
knowledge (experience, awareness) and attitude.
S45: Van Velsen et al. (2016) explain that they
found an indication of prior experience with
telemedicine playing a role in the formation of trust
beliefs among healthcare professionals, where lack
of knowledge and bad experiences led to low
trust. S14: Hsieh (2015) describe how positive or
negative correlation exists between [physicians’]
attitudes toward using the EMR exchange.
5.3 Organizational Factors
The main ‘multilevel’ factors, that may act as a
facilitator or barrier to HCT trust on organizational
level, is training and technical support. It is reported
a little more often as contributing positively as the
facilitator of trust and when it is a negative factor,
training could be non-existent, but also inadequate.
S17: Kayyali et al. (2017) describe that, when
healthcare professionals used telehealth, it also
raised the need for telehealth training packages for
clinicians. It is therefore not surprising that in a
context where healthcare professionals have very
limited time to learn to use a new HCT, training and
technical support plays an important role in forming
trust in the technology. Other influencing trust
barriers include governance/regulatory compliance
and policies.
Trust Factors in Healthcare Technology: A Healthcare Professional Perspective
459

6 CONCLUSION
HCT trust is complex, multi-dimensional, and
influenced by a variety of factors at individual and
organizational levels. Based on the trust factors
identified in this study, the main ingredients for a
successful HCT strategy for any healthcare
professional should include: perceived usefulness,
usability and training and technical support. The
strategy should recognise main trust barriers
including lack of privacy, cost issues, perceived risks
and security issues.
The mapping presented in this paper can guide
decision makers through HCT implementation,
providing them with issues to avoid to ensure
implementation success. HCT trust is complex,
multi-dimensional, and influenced by a variety of
factors at individual and organisational levels
(Kukafka et al., 2003), underscoring the importance
of developing interventions aimed at different levels
simultaneously.
One limitation of this study is that we did not
assess the extent to which proposed interventions
addressed trust barriers or the extent to which they
built on trust facilitators. This would constitute an
interesting avenue for further research in trust in
HCT. Other limitations are the unanswered
questions that are related to the impact of
interventions taking the barriers and the facilitators
identified into account. The relative importance of
each trust factor in specific HCT contexts remains to
be explored by studies using prospective designs. It
is also important to consider how these factors
change over time with the use of a specific
technology and with overall computer literacy.
In this study, we focused on trust in HCT by
healthcare professionals, but we have to
acknowledge that trust in HCT in healthcare
organizations is a multifaceted process since various
stakeholders are involved (Menachemi et al., 2004).
Also, trust is just the first step to consider for the
adoption of the healthcare technology. As noted by
Menachemi et al. (2009), it is important to consider
the viewpoints of all key adopter groups, because
resistance in any of these groups could slow the
overall trust and would not provide essential
information for decision-makers.
For future work, we plan to undertake a
systematic literature review to synthesize evidence,
considering the strength of evidence in assessing the
extent to which interventions addressed the trust
facilitators and barriers in HCT.
ACKNOWLEDGEMENT
This work was supported with the financial support
of the Science Foundation Ireland grant 13/RC/2094
and co-funded under the European Regional
Development Fund through the Southern & Eastern
Regional Operational Programme to Lero - the Irish
Software Research Centre (www.lero.ie).
REFERENCES
Abbas, R. M., Carroll, N., Richardson, I. & Beecham, S.
2017. Protocol for Mapping Study of Trust Factors in
Healthcare Technology: A Healthcare Preofessio-nal
Perspective [Online]. LERO Technical Report.
Available: http://www.lero.ie/sites/default/files/-
TR_2017_04.pdf [Accessed 29/10/2017].
Alford, J. Building Trust in Partnerships Between
Community Orgnization and Government. Changing
the Way Government Works Seminar, Melbourne,
2004.
Almenárez, F., Marín, A., Campo, C. & Garcia, C. PTM:
A pervasive trust management model for dynamic
open environments. First Workshop on Pervasive
Security, Privacy and Trust PSPT, 2004. 1-8.
Anderson, J. G. 2007. Social, ethical and legal barriers to
E-health. International Journal of Medical
Informatics, 76, 480-483.
Bélanger, F. & Carter, L. 2008. Trust and risk in e-
government adoption. The Journal of Strategic
Information Systems, 17, 165-176.
Berner, E. S., Detmer, D. E. & Simborg, D. 2005. Will the
Wave Finally Break? A Brief View of the Adoption of
Electronic Medical Records in the United States.
Journal of the American Medical Informatics
Association, 12, 3-7.
Brooks, R. G. & Menachemi, N. 2006. Physicians’ Use of
Email with Patients: Factors Influencing Electro-nic
Communication and Adherence to Best Practi-ces.
Journal of Medical Internet Research, 8, e2.
Car, J. & Sheikh, A. 2004. Email Consultations In Health
Care: 2-Acceptability And Safe Application. BMJ:
British Medical Journal, 329, 439-442.
Carroll, N. 2016. Key success factors for smart and
connected health software solutions. Computer, 49,
22-28.
Carroll, N., Kennedy, C. & Richardson, I. 2016.
Challenges towards a connected community healthcare
ecosystem (CCHE) for managing long-term
conditions.
Cocosila, M. & Archer, N. 2014. Perceptions of
chronically ill and healthy consumers about electronic
personal health records: a comparative empirical
investigation. BMJ Open, 4.
Egea, J. M. O. & González, M. V. R. 2011. Explaining
physicians’ acceptance of EHCR systems: an
extension of TAM with trust and risk factors.
HEALTHINF 2018 - 11th International Conference on Health Informatics
460

Computers in Human Behavior, 27, 319-332.
Gagnon, M.-P., Desmartis, M., Labrecque, M., Car, J.,
Pagliari, C., Pluye, P., Frémont, P., Gagnon, J.,
Tremblay, N. & Légaré, F. 2012. Systematic review of
factors influencing the adoption of information and
communication technologies by healthcare profession-
als. Journal of medical systems, 36, 241-277.
Gollmann, D. 2006. Why Trust is Bad for Security.
Electronic Notes in Theoretical Computer Science,
157, 3-9.
Grandison, T. & Sloman, M. 2000. A survey of trust in
internet applications. IEEE Communications Surveys
& Tutorials, 3, 2-16.
Hall, M. A., Zheng, B., Dugan, E., Camacho, F., Kidd, K.
E., Mishra, A. & Balkrishnan, R. 2002. Measuring
patients’ trust in their primary care providers. Medical
care research and review, 59, 293-318.
Hsieh, P.-J. 2015. Physicians’ acceptance of electronic
medical records exchange: An extension of the
decomposed TPB model with institutional trust and
perceived risk. International Journal of Medical
Informatics, 84, 1-14.
Hung, S.-Y., Tsai, J. C.-A. & Chuang, C.-C. 2014.
Investigating primary health care nurses' intention to
use information technology: An empirical study in
Taiwan. Decision Support Systems, 57, 331-342.
Jøsang, A., Ismail, R. & Boyd, C. 2007. A survey of trust
and reputation systems for online service provision.
Decision Support Systems, 43, 618-644.
Kayyali, R., Hesso, I., Mahdi, A., Hamzat, O., Adu, A. &
Nabhani Gebara, S. 2017. Telehealth: misconceptions
and experiences of healthcare professionals in
England. International Journal of Pharmacy Practice,
25, 203-209.
Krishna, K. & Maarof, M. A. 2002. An Hybrid Trust
Management Model for MAS Based Trading Society,
Universiti Teknologi Malaysia.
Kukafka, R., Johnson, S. B., Linfante, A. & Allegrante, J.
P. 2003. Grounding a new information technology
implementation framework in behavioral science: a
systematic analysis of the literature on IT use. Journal
of Biomedical Informatics, 36, 218-227.
Leroy, G., Chen, H. & Rindflesch, T. C. 2014. Smart and
connected health. IEEE Intelligent Systems, 29, 2-5.
Massa, P. 2007. Trust in E-services: Technologies
Practices and Challenges. A Survey of Trust Use and
Modeling in Real Online Systems, 51-83.
Mays, N., Pope, C. & Popay, J. 2005. Systematically
reviewing qualitative and quantitative evidence to
inform management and policy-making in the health
field. Journal of health services research & policy, 10,
6-20.
Mcknight, D. H., Choudhury, V. & Kacmar, C. 2002.
Developing and validating trust measures for e-
commerce: An integrative typology. Information
systems research, 13, 334-359.
Menachemi, N., Burke, D. E. & Ayers, D. J. 2004. Factors
affecting the adoption of telemedicine—a multiple
adopter perspective. Journal of medical systems,
28, 617-632.
Menachemi, N., Matthews, M., Ford, E. W., Hikmet, N. &
Brooks, R. G. 2009. The relationship between local
hospital IT capabilities and physician EMR adoption.
Journal of medical systems, 33, 329.
Michael, J. B., Hestad, D. R., Pedersen, C. M. & Gaines,
L. T. 2002. Incorporating the Human Element of Trust
into Information Systems. IAnewsletter, 5, 4-8.
Miles, A. & Asbridge, J. E. 2014. The European Society
for Person Centered Healthcare (ESPCH)–raising the
bar of health care quality in the Century of the Patient.
Journal of Evaluation in Clinical Practice, 20, 729-
733.
Misztal, B. 2013. Trust in modern societies: The search for
the bases of social order, John Wiley & Sons.
Pagliari, C. 2005. Implementing the National Programme
for IT: what can we learn from the Scottish
experience? Informatics in Primary Care, 13, 105-111.
Park, H., Chon, Y., Lee, J., Choi, I.-J. & Yoon, K.-H.
2011. Service design attributes affecting diabetic
patient preferences of telemedicine in South Korea.
Telemedicine and e-Health, 17, 442-451.
Petersen, K., Vakkalanka, S. & Kuzniarz, L. 2015.
Guidelines for conducting systematic mapping studies
in software engineering: An update. Information and
Software Technology, 64, 1-18.
Pluye, P., Gagnon, M.-P., Griffiths, F. & Johnson-Lafleur,
J. 2009. A scoring system for appraising mixed
methods research, and concomitantly appraising
qualitative, quantitative and mixed methods primary
studies in Mixed Studies Reviews. International
Journal of Nursing Studies, 46, 529-546.
Raya, M., Papadimitratos, P., Gligor, V. D. & Hubaux, J.-
P. On data-centric trust establishment in ephemeral ad
hoc networks. INFOCOM 2008. The 27th Conference
on Computer Communications. IEEE, 2008. IEEE,
1238-1246.
Robinson, S. L. 1996. Trust and breach of the
psychological contract. Administrative science
quarterly, 574-599.
Ross, S. E., Schilling, L. M., Fernald, D. H., Davidson, A.
J. & West, D. R. 2010. Health information exchange
in small-to-medium sized family medicine practices:
Motivators, barriers, and potential facilitators of
adoption. International Journal of Medical
Informatics, 79, 123-129.
Saleem, J. J., Russ, A. L., Justice, C. F., Hagg, H., Ebright,
P. R., Woodbridge, P. A. & Doebbeling, B. N. 2009.
Exploring the persistence of paper with the electronic
health record. International Journal of Medical
Informatics, 78, 618-628.
Van Velsen, L., Van Der Geest, T., Van De Wijngaert, L.,
Van Den Berg, S. & Steehouder, M. 2015.
Personalization has a Price, Controllability is the
Currency: Predictors for the Intention to use
Personalized eGovernment Websites. Journal of
Organizational Computing and Electronic Commerce,
25, 76-97.
Van Velsen, L., Wildevuur, S., Flierman, I., Van
Schooten, B., Tabak, M. & Hermens, H. 2016. Trust in
telemedicine portals for rehabilitation care: an
Trust Factors in Healthcare Technology: A Healthcare Professional Perspective
461

exploratory focus group study with patients and
healthcare professionals. BMC Medical Informatics
and Decision Making, 16, 11.
Who. 2017. Available: http://www.who.int/topics/-
technology_medical/en/ [Accessed 5th July 2017].
Wu, I.-L. & Chen, J.-L. 2005. An extension of Trust and
TAM model with TPB in the initial adoption of on-
line tax: An empirical study. International Journal of
Human-Computer Studies, 62, 784-808.
Wu, J.-H., Shen, W.-S., Lin, L.-M., Greenes, R. A. &
Bates, D. W. 2008. Testing the technology acceptance
model for evaluating healthcare professionals'
intention to use an adverse event reporting system.
International Journal for Quality in Health Care, 20,
123-129.
Yarbrough, A. K. & Smith, T. B. 2007. Technology
Acceptance among Physicians. Medical Care
Research and Review, 64, 650-672.
Yusof, M. M., Stergioulas, L. & Zugic, J. 2007. Health
information systems adoption: findings from a
systematic review. Studies in health technology and
informatics, 129, 262.
HEALTHINF 2018 - 11th International Conference on Health Informatics
462
