
Towards an Agent-based Model to Monitor Epidemics and Chronic
Diseases in DR Congo
Jean-Claude Tshilenge Mfumu
1
, Annabelle Mercier
2
, Christine Verdier
1
and Michel Occello
2
1
Grenoble Alps University, CNRS, LIG, F-38000 Grenoble, France
2
Grenoble Alps University, LCIS, 50 Rue Barthélémy de Laffemas, 26000 Valence, France
Keywords: Epidemic, District Health, Agent-based Model, Simulation.
Abstract: Many contagious diseases occurred around sub-Saharan countries in the last decade due to the inefficiency
of health structures to anticipate disease outbreaks. In a huge poorly-infrastructured country such as The
Democratic Republic of Congo (DRC) with insufficient health staff and laboratory facilities, to provide
quick response to an urgent case of epidemic is challenging especially facing the development of its rural
areas. As DRC’s Health System has three levels (peripheral, regional and national levels), from producing
health data at peripheral to national level that takes the decision, it can take time resulting in the spread of
disease. The lack of communication between health centers and laboratory facilities in the same health zone
does not contribute to regional riposte. This paper proposes to face this problem using an agent-centered
approach to study through simulation how to improve the process. An experiment is described by
agentifying two health zones on the same regional level to show how it can reduce the decision time.. It
consists of 2 peripheral coordination offices, 2 labs and 2 health zones the former with 12 health centers and
the latter with 20 health zones. The interaction between these agents will provide a first model to be
compared with the current system in other to reduce decision time.
1 INTRODUCTION
Access to health care is a major concern in
developing countries. The Democratic Republic of
Congo ranks among the poorest countries according
to its HDI
1
(UNDP, 2016). Despite its millions of
hectares of arable land, this vast country of Central
Africa is experiencing serious difficulties in
improving the living conditions of its population,
particularly in the field of basic health care. Life
expectancy at birth is 50 and 53 respectively for men
and women (WHO, 2014).
The country is currently divided into the city-
province of Kinshasa and 25 other provinces. The
provinces are subdivided into territories which are
divided into sectors. To facilitate the supervision of
health structures, the DRC health system is divided
into three levels (Ministère de la Santé Publique de
la République Démocratique du Congo, 2006):
central, intermediate and peripheral. The nearest
level to the population is the peripheral area
composed of 518 health zones (HZ) that coordinate
1
Human Development Index
the actions of the health facilities. A HZ is divided
into Health Area (HA). One or more Health Centers
(HC) can be found at an HA. A General Referral
Hospital (GRH) ensures the complementary
packages of health activities of the HZ. The Central
(national) level defines the policies, strategies and
resources of the sector. It enforces strategies and
policies at the peripheral level through the
intermediate level called the Provincial Health
Division (PHD), which coordinates primary health
care and technical support activities for health zones
in a province.
Each HZ has a Health Information Bureau (HIB)
which retrieves the aggregated data from all its
supervised HA to national level for decision
measures. The HIB organizes weekly meetings with
the Health Zone Executive Team (HZET) to decide
on suspicious cases to report to the hierarchy. HZET
manages health facilities (HF), that includes HC and
GRH, and Community-based organizations (CO).
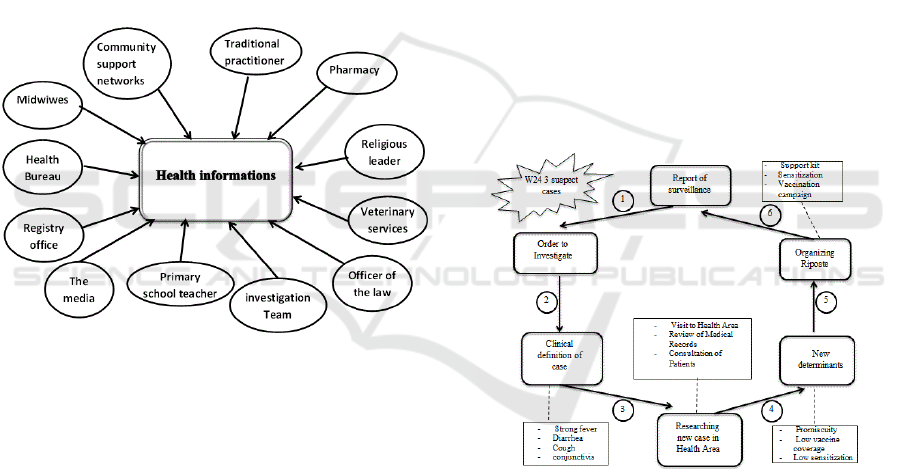
Figure 1 represents three levels of DRC Health
System in with each HZET supervises many HC and
one GRH at peripheral level. PHD at intermediate
level provides technical assistance to HZET while
Mfumu, J-C., Mercier, A., Verdier, C. and Occello, M.
Towards an Agent-based Model to Monitor Epidemics and Chronic Diseases in DR Congo.
DOI: 10.5220/0006557900830093
In Proceedings of the 11th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2018) - Volume 5: HEALTHINF, pages 83-93
ISBN: 978-989-758-281-3
Copyright © 2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
83

Direction of Disease Control (DDC) under National
Health Minister (NHM) gives national policies to 26
PHD at central level. Provincial Health Minister
plays the role of political authority.
Figure 1: Three levels of DRC health system.
As a WHO member country, DRC benefits from
the technical and financial support of the partners to
respond to epidemics under the conditions stipulated
in the International Health Regulations (IHR)
(WHO, 2005). All cases of these four diseases must
be automatically notified to WHO: smallpox,
poliomyelitis due to wild-type poliovirus, severe
acute respiratory syndrome (SARS) and cases of
human influenza caused by a new subtype. On the
ever-changing list of diseases provided by IHR, each
country is free to add other diseases with epidemic
potential or not, which constitute a public health
problem.
Access to basic care is difficult for a large part of
the population. People visit the health facilities in
case of extreme urgency. This is more evident in
rural areas where the diminishing resources of
farmers do not allow them to consult medical
services often. Often health care is provided during
free medical workers’ campaigns.
To collect data about suspicious cases to the
hierarchy for decision-making, the most widely used
ways are described as follows (Ministère de la santé,
2012):
-Health facilities;
-Information from community members
who are experienced in unusual symptoms
and signs;
-Pharmacies that report increasingly
purchases of the same drugs or detect
recurrent treatment;
-School reporting an unusual rate of pupil
absences due to bizarre signs and
symptoms;
- New suspect cases discovered during
medical consultations;
-Medical records providing information on
new diseases detected in the population;
-Media (radio, television or newspapers)
reporting unusual events;
-Civil registries indicating an increasing
rate of maternal deaths;
Despite great efforts to improve disease
surveillance and response, DRC faces big challenges
in identifying, diagnosing and reporting infectious
diseases properly due to the remoteness of
communities, the inadequate transport and
communication infrastructures and the lack of
qualified health staff and laboratory facilities to
ensure accurate diagnosis.
The challenge, in this paper, is to find new
technical solutions based on real population life and
situation to improve health services organization and
data sharing in order to detect infectious disease
very quickly, organize the response and prevent the
spread of the disease.
2 ISSUES
In this paper, we present a part of this challenge. We
propose a multi-agent system to simulate the
interactions between actors working together to
organize an optimal response to epidemic detection.
When a new case of infectious disease is suspected
in HC, actors will collaborate to report it to PHD
through HZET. The approach will be based on the
current DRC heath system processes to extract
relevant actors’ tasks. The identification of these
actors and their tasks will provide the opportunity to
simulate a new system that distributes the entire
competences of the old heath system to those actors
in order to improve their collaboration and
eventually shorten the making-decision time
response. Work-sharing protocols will be proposed
to simplify the complexity of the data sources.
A MultiAgent System (MAS) is a set of agents
situated in a common environment, which interact
and try to reach a set of goals. Through these
interactions, a global behavior, more intelligent than
the sum of the local intelligence of multiagent
system components, can emerge. By ‘agent’ we
mean a software entity evolving in an environment
that it can perceive and within which it reacts. It is
provided with autonomous behaviors and some
objectives. Autonomy is the main concept in the
agent issue: it is the ability of agents to control their
actions and their internal states. The agents’
autonomy implies no centralized control
(Wooldridge, 1999). One of the advantages of MAS
HEALTHINF 2018 - 11th International Conference on Health Informatics
84

is to model systems where a global description is not
possible at any given moment. Multiagent
conception is well suitable to model actors described
in Figure 1.
This paper focuses precisely on improving the
process of reporting health data from the peripheral
level to the hierarchy for rapid decision-making and
anticipate as much as possible the medical response..
Hierarchical dependency between levels forbids
periphery to directly transmit health data to National
level for quick decision. As information must pass
through intermediate level (PHD) combined with
often defective means of communications, it
drastically hampers the fight against a propagation
of a disease.
The next section shows the related work in
healthcare and multiagent domains. Section 3
describes the healthcare system and problematic in
DRC. The methodological approach and agent’s
models are explained in section 4. The model is
validated by a simulation presented in section 5.
Future research directions and conclusion are
developed in section 6.
3 RELATED WORK
Information and Communication Technology is a
powerful solution for health care in developing
countries (Greenberg, 2005). It made possible the
improvement of remote patient follow-up (Wouters
and all, 2009), controlling the progression of malaria
(Zurovac and all, 2012), improving the uptake of
information from health systems (Mutale and All,
2013).
Mobile phone coverage in Africa grew from 10
percent in 1999, 65 percent in 2008 to more than 70
percent in 2012(Aker and Mbiti, 2010). This
technology is used to cover numeric fraction. To
improve drug adherence and suppression of plasma
HIV-1 RNA load in Kenyan, mobile phone
communication between health-care workers and
patients starting antiretroviral therapy was set up
(Lester and all, 2010).Text-message reminders sent
to health workers' mobile phones improved and
maintained their adherence to treatment guidelines
for outpatient pediatric malaria (Zurovac and all,
2011).
Phone traces are powerful tools to estimate
population migration while investigating an
outbreak. These techniques were used to demonstrate
the feasibility of rapid estimates and to identify areas
at potentially increased risk of outbreaks in Haiti
(Bengtsson, 2011). They produced reports on SIM
card movements from a cholera outbreak area at its
immediate onset and within 12 hours of receiving
data. Results suggest that estimates of population
movements during disasters and outbreaks can be
delivered rapidly and with potentially high validity
in areas with high mobile phone.
A trial of mobile phone text messaging for
diabetes management in an eight-month period to
transmit data such as blood glucose levels and body
weight to a server that automatically answered with
a monthly calculated glycosylated hemoglobin
result. The trial results suggest that sms may provide
a simple, fast and efficient adjunct to the
management of diabetes ( Ferrer-Roca, 2004).
In developed countries SMS messages have been
widely used to remind patients of scheduled
appointments (Hasvold, 2011; Car and all, 2008).
Similarly, more complex mobile phone applications
have shown significant improvement in the follow-
up of malaria patients in Thailand (Meankaew,
2010). The same approaches have been tested in
Africa as part of the SMS reminder package to
improve patients’ adherence to antimalarial
treatment schedules in .six sub Saharan countries
(Zurovac, 2012).
Even if text messaging is the simplest and the
most widely used technology function for which all
of the reviewed studies have shown ease of use in
reporting periodic data from the health system
periphery to control managers, it however remains to
be proved for interventions targeting individual
patients, for whom a high facility workload or
illiteracy may present a barrier (Zurovac, 2012).
Simulation has a broad application potential in
healthcare. The more general classification is
clinical, operational, managerial and educational
simulation (Barjis, 2011). Managerial and
operational of simulation are closely interrelated.
These two together are the core components for
healthcare process management. Some challenges
and trends of simulation models in healthcare in the
past two decades have been developed (Almagooshi,
2015). The design of a web-based clinical decision
support system that guides patients with Low Back
Pain in making suitable choices on self-referral has
been experienced in Netherlands (Nijeweme-
d’Hollosy and all, 2016).
MAS is used to describe an approach to the
analysis and development of telemedicine systems
(Mea, 2001), to manage communications in wireless
sensor networks (Jamont and Occello, 2007), the
epidemiological decision support system (Weber and
all, 2006), the care of seniors at home (Mercier and
all, 2013), decision-making for the monitoring and
Towards an Agent-based Model to Monitor Epidemics and Chronic Diseases in DR Congo
85

prevention of epidemics (Younsi, 2016), evaluation
of the disaster response system (Bae, 2017), medical
sensor modules in conjunction with
wireless communication technology supporting a
wide range of services including mobile
telemedicine, patient monitoring, emergency
management and information sharing between
patients and doctors or among the healthcare
workers (Byung-Mo and All, 2006) .
MAS can be considered a suitable technology for
the realization of applications for providing
healthcare and social services where the use of
loosely coupled and heterogeneous components, the
dynamic and distributed management of data and the
remote collaboration among users are often the most
requirements (Bergenti, Poggi, Tomaiuolo, 2013).
Cooperation in the Agent Technology can provide
better healthcare than the traditional medical system
(Jemal and All, 2015). Real programs built on the
multiagent paradigm are still evolving towards a
complete maturity, and the variety and complexity
of the e-health scenario make it one of most
interesting application fields, able of verifying the
advantages of their use of the conditioning their
evolution (Bergenti, Poggi, Tomaiuolo, 2016).
MAS was used to monitor a generic medical
contact center for chronic disease environment,
detect important cases, and inform the healthcare
and administrative personnel via alert messages,
recommendations, and reports, prompting them to
action (Koutkias, Chouvarda and Maglaveras,
2005). Developed MAS applications in healthcare
can provide a reasonable way to mitigate the cost
due to increased demand for services (Shakshuki and
all, 2015).
An Agent-Based Model (ABM) with Geospatial
and Medical Details was used to evaluate the
efficiency of disaster responders to rescue victims in
a mass casualty incident situation in South Korea
(Bae, 2017).
ABM can cooperate to share tasks between
sensors to observe a phenomena (Jamont, 2009), to
manage diabetes treatment between Caregivers and
Patients. The usability evaluation of a collaborative
information system for dementia assessment built
using a user-centred design approach was
experienced in Norway (Berglind and all, 2016). But
from several research papers we have reviewed we
didn’t find a paper addressing ABM in the sharing of
tasks of the actors involved in the processes of the
feedback of the multi-source health information and
the organization of the response to a disease with
high epidemic potential.
4 HEALTH DISTRICT IN DRC
4.1 Administrative Structures
The management of the patient and the reporting of
suspected cases are managed by the peripheral level
through health centers and the general reference
hospitals. The health data collected by the HF are
transmitted to the HZET for consolidation and
transmission of aggregated data from the HZ to the
PHD. This intermediate level structure convenes
weekly meetings to analyze data from each HZ,
decides on actions to be taken and produces
consolidated data from across the province.
The PHD must transmit the health data from its
province to the central level for a second analysis
and national consolidation. If suspected cases
reported by HZ require deeper investigation,
laboratory tests or kits, the PHD will seek technical
and financial support from the central level in the
event of its inability to provide the necessary means.
The Disease Control Direction (DCD) is the
central respondent. It also organizes weekly
meetings to analyze health data from all provinces. It
often provides advice and recommendations to PHD
for monitoring suspect cases in accordance with the
national policy of the sector. It can solicit
government authorities, special programs, partners
and even the international community. Figure 1
shows the data from the periphery to the national
level. Since decision-making is pushed back to the
central level, it can intervene belatedly at the risk of
witnessing an alarming spread of an epidemic with
high epidemic potential.
4.2 Structure Dependencies
The first difficulty in managing epidemics begins
with the processing of data from multiple sources at
the HZ level. National policy has expanded the list
of groups of individuals who can retrieve
information from suspect cases (Figure 2). This
information, which often comes in the form of phone
calls or narrative, is not exhaustive. Hence the
interest in diversifying the mode of communication
by adding text and voice sms, tweets and phone calls
on green lines.
A second difficulty in the accurate identification
of suspect cases is the insufficient number of
qualified health personnel (Ministère du Plan et de
Suivi de la Révolution de la République
Démocratique du Congo, 2014). In spite of the
training courses organized by the HZET for the
benefit of community relays and staff of health
HEALTHINF 2018 - 11th International Conference on Health Informatics
86
facilities, there are gaps in the implementation of the
information brought to their attention. For example,
the PHD conducts a thorough investigation by
qualified personnel as soon as the number of
suspected cases reaches the threshold for each
pathology. Lack of information on the list of the
nearest laboratories delays response time to confirm
cases and ensure accuracy of diagnosis.
Hierarchical dependence does not favor
communication between structures of the same level.
This is the case for the health areas of a HZ,
contiguous health areas but belonging to different
PHD. This lack of dialogue can lead to the non-
detection of an epidemic for the simple reason that
the number of cases is not reached in a HZ.
However, by combining this number with that of the
contiguous health areas, we could detect the
pathology at the intersection of the provinces, which
constitutes a business lock.
Figure 2: Many structures are designated to produce
Health data at each Health Zone.
4.3 Collection and Response for
Epidemic Surveillance
The designated structures report information relating
to suspect cases to the FOSA or HZET. Apart from
the pathologies of the International Sanitary
Regulations (smallpox, poliomyelitis due to wild
polio virus, human influenza and Severe Acute
Respiratory Syndrome (SARS)), the authorities have
added to the list of diseases with epidemic
Eradication measures or Elimination and other
chronic diseases. Reporting of cases is immediate,
weekly, monthly or quarterly according to the
contagiousness of the pathologies.
4.4 Data Collection and Epidemics
Response
As soon as they appear, suspect-cases information
must be transmitted to HZET by all data providers
indicated on 3.2. . When the number of suspect cases
in HZ equals to the threshold according to the
pathology observed, a rapid riposte team (RRT) has
to investigate some HC and the population of the
concerned HZ to make sure the allegation was
correct. The investigation of RRT team could result
to laboratory tests of some samples. In case of
riposte many hierarchical structures such as PHD
and national level would intervene to provide
technical and financial support.
The process used to organize riposte (Ministère
de la Santé Publique de la RDC, 2012) is shortly
described in Figure 3. HZET analyze the report of
surveillance to determine if the number of suspect
case has reached the threshold to order an
investigation. RRT will research new cases at HA
according to the clinical definition of case. It will
find out new determinants of the outbreak to report
to PHD in other to realize the response.
Figure 3: Cycle of outbreak response.
A final evaluation of outbreak response
presented as a report of the process can be shared
with other HZ and Health Facilities.
This type of system is well suited to MAS using
an AEIO representation. The real system is analyzed
with four elements the Agent, the Environment, the
Organizations and the Interactions between the
agents. This model will be detailed in the next part.
Towards an Agent-based Model to Monitor Epidemics and Chronic Diseases in DR Congo
87

5 INDIVIDU-CENTERED
MODELS
“The process of designing a model of a real system
and conducting experiments with this model for the
purpose either of understanding the behavior of the
system or of evaluating various strategies (within the
limits imposed by a criterion or a set of criteria) for
the operation of the system” is a definition given by
(Shannon, 1977) for simulation activity.
At this stage of this research, the simulation's
objective is to understand the DRC healthcare
system for Epidemic diseases. Multiagent-based-
simulation (MABS) allows explicitly modeling the
behavior of each individual and viewing the
emergent system from the interactions between the
individuals.
In further work, on the one hand, we will
determine some metrics to analyze process
simulations and on the other hand, we plan to
develop modules in embedded systems (like phones
or tablets) to assist the end-user in the data
collection, coupled with the multiagent system.
(Morvan, 2013) proposes a survey on MABS and
presents several multiagents platforms. In these
existing platforms, we have not found solutions
which can act as both a simulation system and a tool
to end-users on embedded systems.
However, the DIAMOND method and the
MASH simulator developed in LCIS Laboratory will
be used to model and simulate the system (Jamont
and Occello, 2007, 2009).
The hierarchical organization for collecting data
in DRC (healthcare system) administration is a good
candidate for a multiagent model because there are
several kinds of agent with their own goals which
share the same global achievement. In the process
described previously (figure 3), the agents use some
knowledge and tasks to perform a main goal
together: collecting data in order to respond with
efficiency to epidemic. The process is modeled by
agents able to be simulated in the MASH simulation
platform. The advantage of doing this is to have an
individual-centered vision of the process. After that,
we will be able to contribute to the improvement of
the process with an exterior view provided by the
simulation and propose changes and ideas to
improve the response time, for example.
This section shows the steps to break down
multiagent system’s elements.
5.1 Agents’ Tasks and Knowledge:
The Internal Behavior
For starting the analyses, each individual agent’s
behavior is studied. It is a way of seeing things at a
micro level, the phenomenon (at macro level) does
not change and the process remains the same but the
observer’s level changes.
The goal is to be able to adjust the behavior of
each individual agent and possibly add skills to
certain nodes or node types.
The first step is to model into agent the elements
of the process. For the problem, it is the health
centers, the main hospital of the health areas,
province districts and national health entity related
to the administrative structures and HZET and RRT
for human team working group. The figure 4 shows
the internal behavior of the RRT.
For each agent, we have to list all their skills,
what information will be required to store and to
handle and how the agent acquires this information.
This information should be acquired directly by
perception (e.g. the user grasps something) or on
demand by asking other nodes (higher hierarchy or
same level nodes).
With this step, we obtain for each agent, a vision
of the relevant knowledge to perform its individual
tasks. This is all the necessary information for the
agent who works in the system. The result is a set of
tasks that the agent can perform. These tasks
correspond to the skills of each node. Some skills
are made locally without need to contact other
agents. But to achieve a goal, an agent should have
partial information and needs to ask other agents to
complete their goal. However, we will have
cooperative behavior in opposition to completely
individual behavior entirely internal to the agent.
This kind of social behavior reflecting an interaction
among several agents: either to gain information or
to share tasks.
HEALTHINF 2018 - 11th International Conference on Health Informatics
88
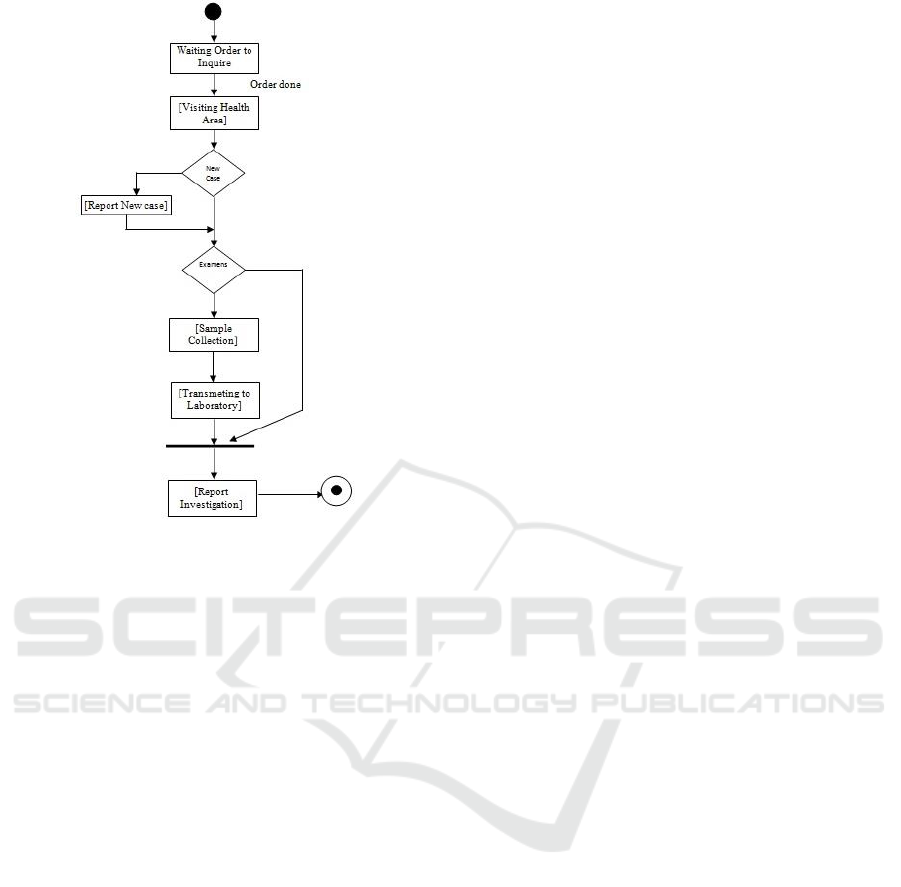
Figure 4: Investigating an outbreak.
5.2 Agent’s Sharing Data and
Interactions
5.2.1 Social Behavior
In this step, we will have to create interactions
between nodes for example to back up information
(HCR to HZET) or to receive orders (HZET from
PHD). These interactions should be between
different partner groups such as health areas. In the
implementation, we define very simple interaction
protocols for data exchange such as receiving
information, answers/queries or order to perform a
task. For some tasks, such as health alert
surrounding areas, it is no longer just a request for
information but cooperative behavior; that is to say
behavior that brings into play several kinds of
agents. In need thereof soliciting other agents, the
agent is led to use interaction protocols. We will
therefore define how this behavior will be realized
by defining a more sophisticated interaction protocol
than query/response. Diverse protocols are available
for negotiating, giving orders, waiting for answers.
The interaction patterns that will govern this
cooperative behavior will be organized between the
agents.
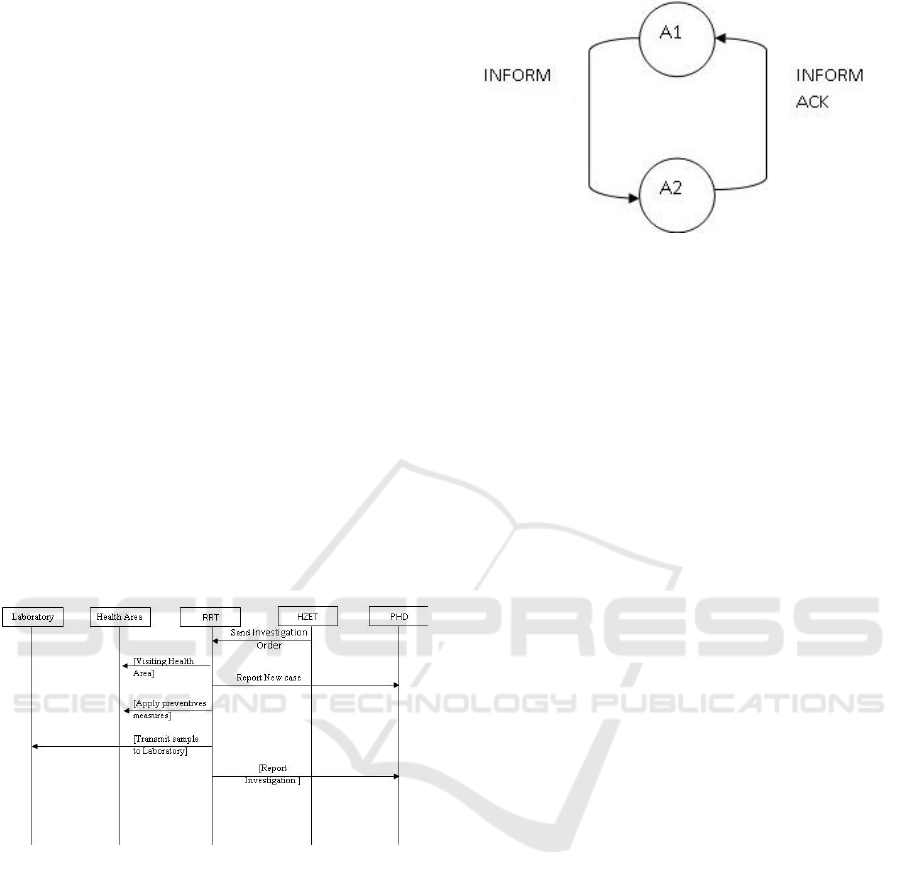
5.2.2 Interaction Protocols
The protocol is a part of the agents’ knowledge.
Agents have a list of protocols that they should
initiate or that they are able to use to answer others.
For the moment, we use a simple protocol with two
states as represented in figure 6. For example, Agent
A1 launches an instance of protocol P1, it is in the
state S1. The agent A2 receives a solicitation of A1
with the performative “information” in the state S1.
A2 knows the protocol and searches the next
transition; it passes in state S2 and sends an
acknowledgment to agent A1. A1 treats the message
and the conversation finishes. The ACL FIPA
compliant Performatives are used:
• RDCMessage.ACL_QUERY_REF for
queries/answers,
• RDCMessage.ACL_REQUEST for an order
to perform a task and,
• RDCMessage.ACL_INFORM for
inform/acknowledgment.
5.2.3 Position in the Organization
The last step is to take into account the position in
the organization when an agent will initiate
interactions with each other. An organization should
be a hierarchy or a simple group. As an example, to
alert neighboring HZ, health center agents will know
the surrounding areas of health, which is a group,
that is to say an organization in the multiagent
system and make a decision based on its position in
this group. The agent’s position in the organization
is integrated in the decision making loop.
5.2.4 Agent’s Internal Decision Making
Loop
The previous steps give the agent’s skills, the
agent’s complex behavior (internal and social), the
knowledge of interaction protocols. We will now
build the agent decision loop. On the one hand
purely individual behavior runs only with an agent’s
context information and does not need other agents
to complete the agent goal. On the other hand, social
behavior involves relationships with other agents.
Using an individual-centered approach defines the
agent at micro level so the interactions with other
agents have to be merged with the internal behavior
in the agent’s decision loop. The individual and
cooperative behaviors are both integrated into the
decision making loop. In the individual behavior,
there is a set of tasks that are launched in the internal
Towards an Agent-based Model to Monitor Epidemics and Chronic Diseases in DR Congo
89
decision loop. In its decision loop, the agent should
have to respond to the message from others’ which
are part of interaction protocols initiated by other
agents or parts of own launch of the agent
interaction patterns. These tasks have to be
synchronized with the messages received from the
others agents.
As an external view, basically, huge decision
loops, which are decentralized in the several kinds of
agents, seem to be synchronized at the system level,
but in fact, each agent decides what state it passes
according to its knowledge and the state of its
interactions.
5.3 Collaborative Tasks of Agents
Agents would collaborate to achieve some
objectives. To investigate on HA, RRT must wait for
an order from HZET. The later receives health data
every week from HC and checks if the threshold of
the followed pathology has been reached. The same
collaboration is needed between RRT and HA, RRT
and Laboratory. The sequence diagram (Figure 5)
gives a snapshot of the kind of collaboration found
in agents concerned with an outbreak investigation.
Figure 5: Sequence diagrams of investigating an outbreak.
5.3.1 Message Format for Interaction
The messages exchanged between agents contains
sender and receiver agents, protocol information and
data to manage like [sender; receiver; conversation;
perform; protocol; inst_prot; state_prot; data]. The
data follow a format according to the performative.
To interact through a message sent by another
agent, a simple protocol is established. For instance
when RRT asks a laboratory to perform exams, he
has to first check its state to be convinced that it can
answer his request. A simple protocol with
acknowledgment is used.
Figure 6: Protocol for information with acknowledgment.
The agent changing state when he asks for
information and when he receives the answer to his
request is represented in Figure 6. In a future
simulation, a negotiation protocol with a call for
proposal to several laboratories will be tested.
However, the agent launching the conversation
should negotiate among laboratories which one is
available, near or powerful.
6 SIMULATION RESULTS
In order to test and evaluate our approach, we
adapted MASH simulator developed for a wireless
sensor multiagent system (Jamont and Occello,
2009). We focus our simulation to the former
Equateur Province that was split in 2015 into the
new, smaller Equateur province, as well as
the Tshuapa, Mongala, Nord-Ubangi and Sud-
Ubangi provinces.
Located in the north of the country, the province
bordered the Republic of the Congo to the west,
the Central African Republic to the north, to the east
the Orientale province, and to the south the Kasai-
Oriental, Kasai-Occidental.
The former Equateur registered 18% of cholera
outbreak suspect cases on 2016 with 31% of death
(Ministère de la Santé Publique de la RDC, 2017).
The crossing of many rivers facilitates the spread of
a disease such as cholera if health staffs don’t alert
the population as soon as a suspect case is noticed.
The simulation concerns precisely Tshuapa
Province that doesn’t register cholera outbreak
suspect case on 2016 while its neighbors Equateur
and Mongala provinces have respectively 2751 and
1781 suspect cases with deaths. The main idea is to
see how the future system would react if each actor
of health system could perform his own task with
autonomy. These experiences could result to many
scenarios and the best of them will be proposed to
DRC’s Health System to reduce time decision as
HEALTHINF 2018 - 11th International Conference on Health Informatics
90
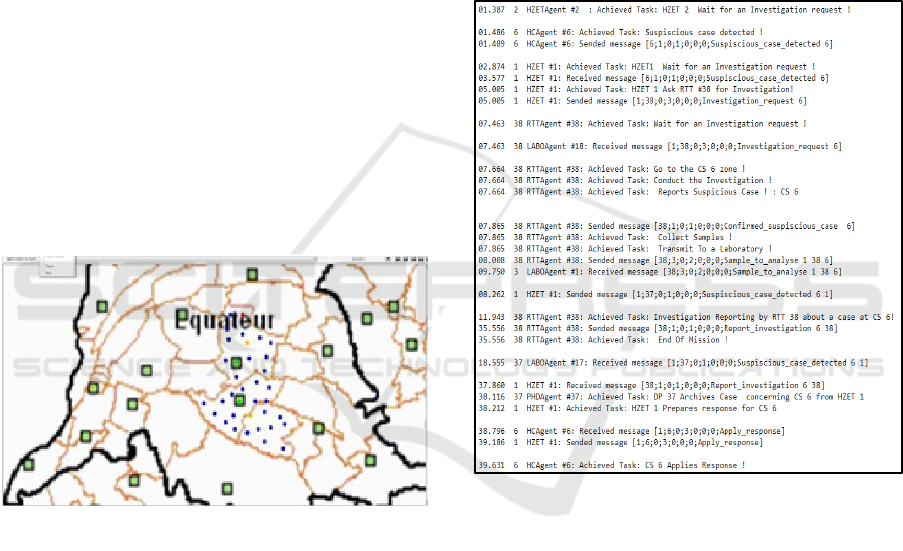
each actor can execute his talks according to the
knowledge of environment and outbreak he will be
provided with.
We chose two HZ of Tshuapa PHD for the
simulation. Befale and Boende are HZ that didn’t
register cholera outbreak in 2016 but they are
bordered with two provinces crossed by rivers that
encountered many deaths due to Cholera at the same
period.
To respond to an outbreak noticed at a HC,
health staff of the concerning HC must refer to
HZET. In their turn HZET must refer to PHD and
PHD to central level. This chain of hierarchical
contacts can enlarge time decision.
In our simulation we worked with this
hypothesis: each actor must contact immediately the
nearest one able to answer to his request or to use his
information to make decision. We considered only
three HA of each HZ and twenty HC in blue with
two HZET (in yellow for each HS) and two medical
test laboratories (Labo in green square).The
suspicious case detected in HC #6 is in red. Figure
illustrates those actors working as Agents in two HZ
named Befale and Boende. The map represents the
former Equateur Province.
Figure 7: Collecting data system simulation in Befale and
Boende.
The simulation trace file (Figure 8) shows the
communication between the agents. As they are
autonomous they perform their own tasks like
“conduct an investigation” and manage messages
like “receive sample to analyze” or “send suspicious
case detected”. The HZET Agents (#1 and #2) are
waiting for a suspect case message from any HC.
Whenever HZET Agent receives such a message he
builds a RRT Agent able to investigate in HAs
around suspect case. RRT Agent could send samples
to LaboAgent while searching for new cases in HAs.
The organization of outbreak riposte depends on the
results from LaboAgent and investigation report
from RRT Agent. .
The agents operate independently: RRTAgent
completes a full investigation, LaboAgent conducts
quality medical testing and PHD manages all
informations from HZET under it supervision.
Message synchronization between kinds of agent is
done in the agent's decision loop. A protocol with
two states is used and implements KQML-like
performatives. The four numbers in the message are
“1” for inform (give information), “2” for query
information (ask for an information) and “3” for
request (ask for a task to be done). The agents
communicate and achieve their goal by reacting to
messages from others or executing their inner task as
response to a query.
Figure 8: Simulation trace.
7 CONCLUSIONS
In this paper, we presented how ABM can be used to
monitor an epidemic outbreak in two Health zones
(Befale and Boende). The process of collecting
health data in health Zones and the response given
by provincial and national levels were analyzed. A
multiagent model for healthcare system in DRC has
been built to represent the use case. This first
experience of our research and the results described
in the section 5 convince us that it is possible to
make a social simulation of the real system. It’s
feasible to simulate the hierarchical organization of
the administrative structures, to collect and manage
health data from health system actors.
Towards an Agent-based Model to Monitor Epidemics and Chronic Diseases in DR Congo
91

Our self-centric analysis and simulation give a
promising result we would like to implement to a
real system by making comparison with the manual
process used to respond to an epidemic disease in
DRC. With certainty, we have some perspectives to
use the simulations. From the study of the current
process and the analyses of its simulation, the
process will be improved by extracting best practices
for a subset of tasks and actors. This paper
represents a first step and a positive sign that shows
that the multiagent solution represents a good
approach to help in decreasing the delay for
riposting.
The multiagent model must be improved. At
first, we are going to integrate analyses criteria on
the agents like the response time or the agent’s load
that is the number of requests resulting from other
agents to analyze the process and propose
improvements. We should simplify or improve
communication and information management.
Applying enriched agents’ behaviors will give us the
opportunity to simulate an operational system with a
new distribution of powers between agents so as to
improve collaboration and shorten the response time
between the actors.
A second axis of improvement is situated at the
level of the interaction protocols. For the moment,
the protocols described in section 4 have two states.
The social behavior of the agents should be
complicated by implementing for example a call for
proposal in the appropriate situations (medical
analyses in agent laboratory).
At the model level, additional work will be done
on the organization: the information will not only be
managed in a hierarchical way but with groups
dynamically built with explicit criteria such as
geographical location.
The last perspective is to couple the simulation
system with embedded devices to collect data. A
part of the agent perception should be the result of
the automation of a portion of the process embedded
in a phone or a tablet.
REFERENCES
Aker, J. C., and Mbiti, I. M., 2010. Mobile phones and
economic development in Africa. The Journal of
Economic Perspectives, 24(3), 207-232.
Almagooshi, S., 2015. Simulation modelling in healthcare:
Challenges and trends. Procedia Manufacturing,
3(supplement C):301–307. 6th International
Conference on Applied Human Factors and
Ergonomics and the Affiliated Conferences.
Bae, Jang Won, Shin, Kyohong, LEE, Hyun-Rok, 2017.
Evaluation of Disaster Response System using Agent-
Based Model with Geospatial and Medical Details.
IEEE Transactions on Systems, Man, and Cybernetics:
Systems.
Barjis, Joseph, 2011. Healthcare simulation and its
potential areas and future trends. SCS M&S Magazine,
vol. 2, no 5, p. 1-6.
Berglind Smaradottir, Santiago Martinez, Elisabeth Holen-
Rabbersvik, TorunnVatnøy and Rune Fensli, 2016.
Usability Evaluation of a Collaborative Health
Information System. Lessons from a User-centered
Design Process. Healthinf 2016.
Bengtsson, L., Lu, X., Thorson, A., Garfield, R., and von
Schreeb, J., 2011. Improved response to disasters and
outbreaks by tracking population movements with
mobile phone network data: A post-earthquake
geospatial study in Haiti. PLoS Med8, 8.
Bergenti, F., Poggi, A., & Tomaiuolo, M., 2016. Multi-
Agent Systems for E-Health and Telemedicine. In M.
Cruz-Cunha, I. Miranda, R. Martinho, & R. Rijo
(Eds.), Encyclopedia of E-Health and Telemedicine
(pp. 688-699). Hershey, PA: IGI Global.
Bergenti, F., Poggi, A., & Tomaiuolo, M. , 2013. Using
Multi-Agent Systems to Support e-Health Services. In
M. Cruz-Cunha, I. Miranda, & P. Gonçalves (Eds.),
Handbook of Research on ICTs for Human-Centered
Healthcare and Social Care Services (pp. 549-567).
Hershey, PA: IGI Global.
Byung-Mo Han, Seung-Jae Song, Kyu Min Lee, Kyung-
Soo Jang, Dong-Ryeol Shin, 2006. Multi Agent
System based Efficient Healthcare Service, 2006. In
the 8th International Conference on Advanced
Communication Technology, 2006. ICACT.
Car J, Gurol-Urganci I, De Jongh T, Vodopivecjamsek V,
Atun R., 2008. Mobile Phone Messaging Reminders
For Attendance At Scheduled Healthcare
Appointments. Cochrane Database of Systematic
Reviews.
Ferrer-Roca, O., Cardenas, A., Diaz-Cardama, A., and
Pulido, P., 2004. Mobile phone text messaging in the
management of diabetes. Journal of Telemedicine and
Telecare, 10(5):282–285.
Greenberg, A. , 2005. ICTs for poverty alleviation: basic
tool and enabling sector. Technical report, Sida 2005
ICT for Development Secretariat, Department for
Infrastructure and Economic Cooperation.
Hasvold, P. E. and Wootton, R., 2011. Use of telephone
and sms reminders to improve attendance at hospital
appointments: a systematic review. Journal of
Telemedicine and Telecare, 17(7):358-364.
Jamont, J.-P. and Occello, M. , 2007. Designing embedded
collective systems: The diamond multiagent method.
In International Conference on Tools with Artificial
Intelligence, pages 91–94, Patras Greece.
Jamont, J.-P. and Occello, M., 2009. A multiagent tool to
simulate hybrid real/virtual embedded agent societies.
In IEEE International Conference on Intelligent Agent
Technology.
HEALTHINF 2018 - 11th International Conference on Health Informatics
92

Jamont, J.-P., Occello, M., and Lagreze, A. , 2010. A
multiagent approach to manage communication in
wireless instrumentation systems. Measurement,
43(4):489–503.
Jemal, H., Kechaou, Z., Ayed, M. B., and Alimi, A. M. ,
2015. A multi agent system for hospital organization.
International Journal of Machine Learning and
Computing, 5(1):51–56.
Koutkias, V. G., Chouvarda, I., and Maglaveras, N., 2005.
A multiagent system enhancing home-care health
services for chronic disease management. IEEE
Transactions on information technology in
biomedicine, 9(4).
Lester, R. T., Ritvo, P., Mills, E. J., Kariri, A., Karanja, S.,
Chung, M. H., Jack, W., Habyarimana, J., Sadatsafavi,
M., Najafzadeh, M., Marra, C. A., Estambale, B.,
Ngugi, E., Ball, T. B., Thabane, L., Gelmon, L. J.,
Kimani, J., Ackers, M., and Plummer, F. A. , 2010.
Effects of a mobile phone short message service on
antiretroviral treatment adherence in Kenya (weltel
kenya1): a randomised trial. The Lancet,
376(9755):1838 – 1845.
Mea, D., 2001. Agents acting and moving in healthcare
scenario - a paradigm for tele medical collaboration.
IEEE Transactions on information technology in
biomedecine, 5(1).
Meankaew, P., Kaewkungwal, J., Khamsiriwatchara, A.,
Khunthong, P., Singhasivanon, P., and Satimai, W. ,
2010. Application of mobile-technology for disease
and treatment monitoring of malaria in the “better
border healthcare programme”. Malaria Journal,
9(1):237.
Mercier, A., Raievsky, C., Occello, M., and Genthial, D.,
2013. Solutions multi-agents pour la prise en charge
domicile des seniors. Ingénierie des systèmes
d’information, 18(6):83–112.
Morvan, G., 2013. Multi-level agent-based modeling: a
literature survey. The Computing Research Repository,
abs/1205.0561.
Mutale, W., Chintu, N., Amoroso, C., Awoonor-Williams,
K., Phillips, J., Baynes, C., Michel, C., Taylor, A., and
Sherr, K., 2013. Improving health information systems
for decision making across five sub-saharan African
countries: Implementation strategies from the African
health initiative. BMC Health Services Research,
13(2):S9.
Ministère de la Santé Publique de la RDC, 2006.Recueil
des normes de la Zone de Santé. Kinshasa.
Ministère de la Santé Publique de la RDC, 2012. Guide
Technique pour la Surveillance intégrée de la Maladie
et riposte. Kinshasa.
Ministère de la Santé Publique de la RDC, 2014. Plan de
Développement de l'Informatique de la Santé –
PNDIS. Kinshasa.
Ministère de la Santé Publique de la RDC, 2017. Rapports
annuels de surveillance des maladies épidémiques à
potentiel épidémique en République Démocratique du
Congo 2014-2016. Kinshasa.
Ministère du Plan et Ministère de la Santé Publique, 2014.
Deuxième enquête démographique et de santé
(eds-rdc II 2013-2014). Kinshasa.
Mutale, Chintu, Amoroso, Awoonor-Williams, Phillips,
Baynes, Michel, Taylor, Sherr, 2013. Improving health
information systems for decision making across five
sub-Saharan African countries: implementation
strategies from the African Health Initiative. BMC
health services research.
Nijeweme-d’Hollosy, W. O., van Velsen, L., Soer, R., and
Hermens, H., 2016. Design of a web-based clinical
decision support system for guiding patients with low
back pain to the best next step in primary healthcare.
In HEALTHINF 2016.
Shakshuki, E. and Reid, M. , 2015. Multi-agent system
applications in healthcare: Current technology and
future roadmap. Procedia Computer Science,
52(Supplement C):252 – 261. The 6th International
Conference on Ambient Systems, Networks and
Technologies (ANT-2015), the 5th International
Conference on Sustainable Energy Information
Technology (SEIT-2015).
Shannon, R. E., 1977. Simulation modeling and
methodology SIGSIM Simul. Dig., 8(3):33–38.
UNDP, 2016. Human development report 2016. Technical
report.
Weber, A., Rahmani, A., and Dupont, D., 2006.
Multiagent system for flow management in complex
systems: Development of a decision support system in
epidemiology. In European Simulation
Multiconference (ESM).
WHO, 2005. International Health Regulations.
WHO, 2014.World Health Statistics.
Wooldridge, M., 1999. Intelligent agents. In Weiss, G.,
editor, Multiagent Systems: A Modern Approach to
Distributed Artificial Intelligence. MIT Press.
Wooldridge, M., Jennings, N. R., and Kinny, D., 1999. A
methodology for agent-oriented analysis and design.
In Proceedings of the Third Annual Conference on
Autonomous Agents, AGENTS ’99, pages 69–76, New
York, ACM.
Wouters, B.; Barjis, J.; Maponya, G.; Martiz, J. and
Mashiri, M., 2009. Supporting home based healthcare
in South Africa rural communities using USSD
technology. In AMCIS.
Younsi, F., 2016 Mise en place d’un Système
d’Information Décisionnel pour le Suivi et la
Prévention des Epidémies. PhD thesis, Université
d’Oran.
Zurovac, D., Sudoi, R. K., Akhwale, W. S., Ndiritu, M.,
Hamer, D. H., Rowe, A. K., and Snow, R. W., 2011.
The effect of mobile phone text-message reminders on
kenyan health workers’ adherence to malaria treatment
guidelines: a cluster randomised trial. The Lancet,
378(9793):795 – 803.
Zurovac, D., Talisuna, A. O., and Snow, R. W., 2012.
Mobile phone text messaging: Tool for malaria control
in Africa. PLOS Medicine, 9(2):1–6.
Towards an Agent-based Model to Monitor Epidemics and Chronic Diseases in DR Congo
93
