
The Privacy Management Platform
An Enabler for Device Interoperability and Information Security in mHealth
Applications
Christoph Stach, Frank Steimle and Bernhard Mitschang
Institute for Parallel and Distributed Systems, University of Stuttgart,
Universit
¨
atsstraße 38, D-70569 Stuttgart, Germany
Keywords:
mHealth, Device Interoperability, Information Security, COPD, Privacy Management Platform.
Abstract:
Chronic diseases are on the rise. Afflicted patients require persistent therapy and periodic screenings. This
causes high treatment costs and overburdened physicians. Innovative approaches that enable patients to perform
treatment methods on their own are badly needed. Telemedical approaches with the aid of modern Smartphones
connected to medical devices (the so-called mHealth) can be the answer. However, mHealth apps face two key
challenges, namely device interoperability and information security. In this paper, we describe how the
P
rivacy
M
anagement
P
latform (PMP) and its extendable Resources can contribute to these challenges. Therefore, we
analyze a real-world mHealth app and derive generic functional units, each realizing a certain task recurring
frequently within mHealth apps, e. g., metering, data storage, or data transmission. For each functional unit we
provide a PMP Resource, enabling both, device interoperability and information security. Finally, we revise the
analyzed mHealth app using the Resources in order to evaluate our approach.
1 INTRODUCTION
Due to long stand-by times and multiple built-in sen-
sors, the Smartphone became our ubiquitous compa-
nion. New use cases are constantly emerging. Especi-
ally in the health sector, the use of Smartphones can be
highly beneficial to save treatment costs and help pa-
tients who cannot visit their physicians regularly (Silva
et al., 2015). The usability of Smartphone apps
1
in the
health sector—the so-called mHealth apps—is limit-
less. There is an app for almost any situation (Siewio-
rek, 2012).
While there are some mHealth apps for medical
reference (that is, apps providing information about
diseases) as well as hospital workflow management
apps (i. e., apps supporting physicians in their every-
day duties), mHealth apps are mainly from the health
management domain (Milo
ˇ
sevi
´
c et al., 2011). The
latter includes cardio fitness, medication adherence,
and chronic disease management. To this end, these
apps support two essential features: self-observation
and feedback (Mattila et al., 2010). That is, the patient
performs health measurements instructed by the app,
transmits the measured values to the app and the app
1
In the following, we use the generic term app for any
kind of mobile application.
performs analyses on these values. Based on the re-
sults, the app gives the user medical recommendations.
Since mHealth apps involve the patient actively
into the treatment and monitoring process, s/he gets
more aware of his or her condition. So, mHealth apps
change the physician patient relationship especially for
patients with a chronic disease. These patients have
to visit their physician periodically in order to check
certain health values. However, such a metering can
be performed by the patients autonomously, if they
receive a proper guidance tailored to their know-how.
That is, with the help of an mHealth app they are able
to do the monitoring in a telemedical manner. This
take the load off both, patients as well as physicians.
Patients benefit from the freedom to do the metering
at any arbitrary place and time while physicians are
able to concentrate on emergencies. This is not just a
huge saving potential but also improves the quality of
healthcare at the same time (Schweitzer and Synowiec,
2012).
To capture health data, mHealth apps make use
of various sensors. In addition to the already broad
spectrum of sensors built into modern Smartphones
that can be used for healthcare (e. g., a heart rate sensor,
a camera, or a microphone), even medical devices for
home-use can be connected to a Smartphone. The
Stach, C., Steimle, F. and Mitschang, B.
The Privacy Management Platform - An Enabler for Device Interoperability and Information Security in mHealth Applications.
DOI: 10.5220/0006537300270038
In Proceedings of the 11th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2018) - Volume 5: HEALTHINF, pages 27-38
ISBN: 978-989-758-281-3
Copyright © 2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
27
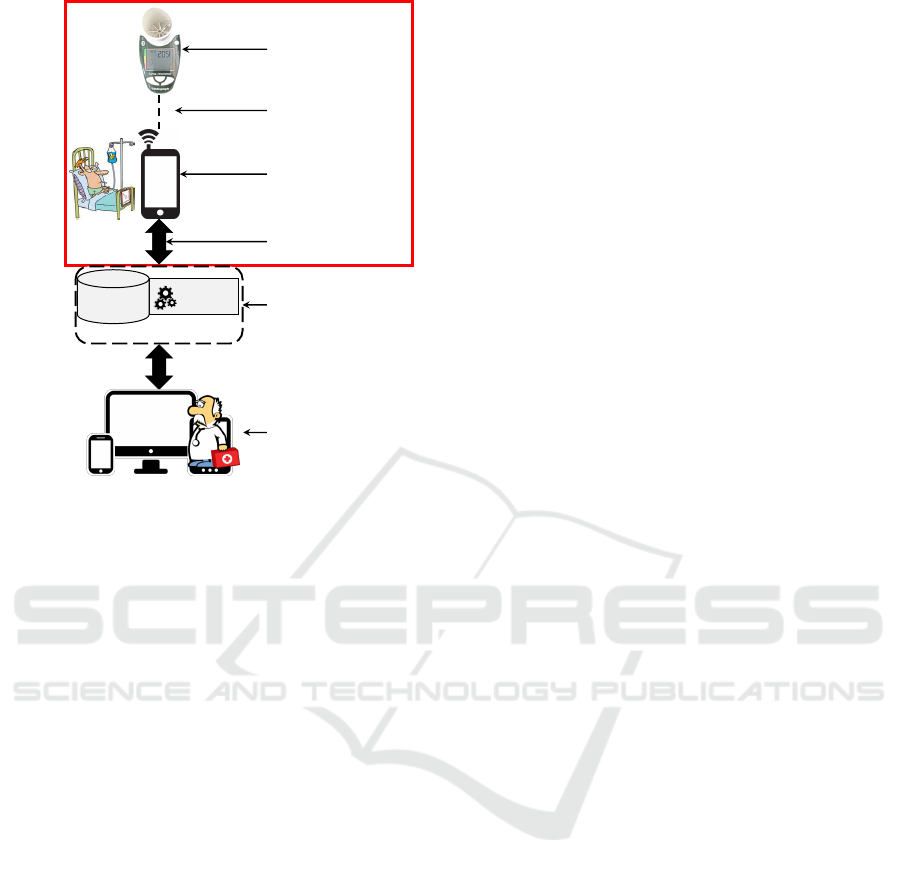
Analytics
Data
Storage
Online mHealth Service
Metering Device (e.g.,
Vitalograph copd-6 bt)
Connection to Smart
Device (e.g., Bluetooth)
mHealth Applications
for Smart Devices
(e.g., ChronicOnline)
Connection to Back-
End (e.g., REST calls)
mHealth Back-End
(e.g., ECHO Platform)
mHealth Application
for Physicians (e.g.,
Diagnosis Tools)
Sensor
Layer
Smartphone
Layer
Back
-End
Layer
Presentation
Layer
Figure 1: Overview of an mHealth System (Red-Rimmed
Components are in the Focus of this Paper).
Vitalograph copd-6 bt is an example for such medical
device.
Yet, the data interchange between medical devices
and Smartphones often fails because of non-uniform
communication protocols. The
device interoperabi-
lity
of Smartphones and medical devices is a key chal-
lenge for the success of mHealth apps (Chan et al.,
2012). Also the assurance of
information security
is vital for mHealth, as patients have to trust their
apps (Bai et al., 2014). Thus, we address these two
challenges in our work. Therefore, we come up with a
concept for an enabler for device interoperability and
information security in mHealth apps. To achieve this
objective, we proceed as follows:
(I)
We analyze a re-
al-world mHealth app regarding the collected data and
used devices.
(II)
We deduce a generic data model for
mHealth apps. Due to this data model, our approach
is applicable for any kind of mHealth app.
(III)
We
identify five recurring tasks within mHealth apps for
which device interoperability and information security
are key requirements, namely login, metering, localiza-
tion, data storage and analytics, and data transmission.
For each of these tasks, we introduce an extension
for the
P
rivacy
M
anagement
P
latform (PMP) (Stach
and Mitschang, 2013), to ensure interoperability and
information security.
(IV )
We use these extensions to
revise the analyzed mHealth app in terms of sensor
support and the patients’ privacy. With this revised
app, we assess the practical effect of our approach.
The remainder of this paper is as follows: Section 2
introduces a real-world application scenario from the
mHealth domain, namely ChronicOnline, an mHealth
app for COPD patients. Then, Section 3 takes a look at
related work concerning connection techniques used
by medical device as well as information security me-
chanisms in mHealth apps. Based on these findings,
we introduce a generic interchange data model for
mHealth apps and induct briefly in the PMP, the foun-
dation platform for our solution approach in Section 4.
Then, Section 5 details on the key components of our
approach and demonstrates their applicability, using
the example of a COPD app. In Section 6 we assess
how our approach contributes to solve information se-
curity and interoperability problems for mHealth apps.
Section 7 concludes this work and gives an outlook on
some future work.
2 APPLICATION SCENARIO
Typically, mHealth systems consist of three layers (Ku-
mar et al., 2013). The Sensor Layer manages the
access to any sensor required by mHealth apps, i. e., it
collects the sensors’ raw data and provides it to subse-
quent layers. In the Smartphone Layer, this data is col-
lected, assessed, and processed. The processing step
transforms the raw data to information. An optional
analysis phase can derive events from the information,
e. g., to detect a seizure automatically. The data can
also be stored on the Smartphone, e. g., to monitor the
progress of the disease. Additionally, the data is for-
warded to on-line servers managed by the Back-End
Layer. While the Smartphone Layer holds health data
of a single patient, in the Back-End Layer the data
of multiple patients is assembled (e. g., to derive new
insights into the course of a disease or to prepare the
data for subsequent in-depth analyses). Via this layer
physicians are able to perform analyses and receive
diagnosis support for each of their patients. For this
purpose, there is sometimes an additional Presentation
Layer. This fourth layer preprocesses the health data
stored in the back-end and presents the relevant data
in a user-friendly manner. So, physicians are able to
interpret the results.
Figure 1 shows the interaction of these four layers.
A metering device can be connected to a Smartphone
via Bluetooth. A patient can install an mHealth app
on his or her Smartphone and use the medical data
recorded by the external metering device. This data
can be enriched by data from the Smartphone’s built-
in sensors (e. g., location data). The app sends the
gathered data to an mHealth back-end for thorough
analyses and to store the data at a central repository.
HEALTHINF 2018 - 11th International Conference on Health Informatics
28

Physicians can access the repository via their diagnosis
tools to find an adequate method of treatment.
Concerning the two key issues addressed in this
paper, namely device interoperability and information
security, several components have to be taken into con-
sideration. Any data interchange between two layers is
a problem, since there are heterogeneous interchange
formats and multiple connection standard. This con-
cerns especially the data interchange between Smartp-
hones and medical devices, since these devices com-
monly define proprietary communication protocols.
Yet, the harmonization of the medical data formats
used by mHealth apps and back-ends has to be con-
sidered as well. While there are several approaches
towards a server-sided unified data model for health
data (e. g., in the HealthVault (Bhandari, 2012)), there
are no such approaches for apps.
Information security has to be considered at any
layer. However, as users cannot influence the security
mechanisms implemented in sensors, data protection
has to be assured mainly on the Smartphone Layer.
While there are approaches to protect sensitive data
on the Back-End Layer (e. g., (Jafari et al., 2011)), an
adequate solution for the Smartphone Layer is missing.
The Presentation Layer does not create any sensitive
data.
So, we focus on the Sensor Layer and the Smartp-
hone Layer in our work regarding both, device in-
teroperability and information security, as there are
adequate solutions for the other layers solving the-
ses issues. However, the usability and security of an
mHealth system is impaired by its weakest component.
That is, the existing usability and security solutions
for the Back-End Layer and the Presentation Layer are
worthless with respect to the whole system, as long
as there are no appropriate approaches for the Sensor
Layer and the Smartphone Layer as well.
In the following, we introduce a real-world mHe-
alth app for COPD patients.
Chronic Obstructive Pulmonary Disease.
COPD is
an obstructive lung disease. Patients suffer from a poor
airflow which worsens over time. According to the
WHO, approximately
6%
of all deaths in
2012
resul-
ted directly from COPD. Even though COPD is not
curable, a fast and persistent therapy can slow the pro-
gression of the disease significantly down. Telemedi-
cine is very appropriate as the required measurements
can be carried out with medical metering devices for
home use (de Toledo et al., 2006).
The ChronicOnline App.
mHealth apps are good for
regularly recording various parameters but they are
insufficient for a comprehensive COPD screening. For
this reason, the University of Stuttgart, the University
of Crete, and OpenIT launched the ECHO project in
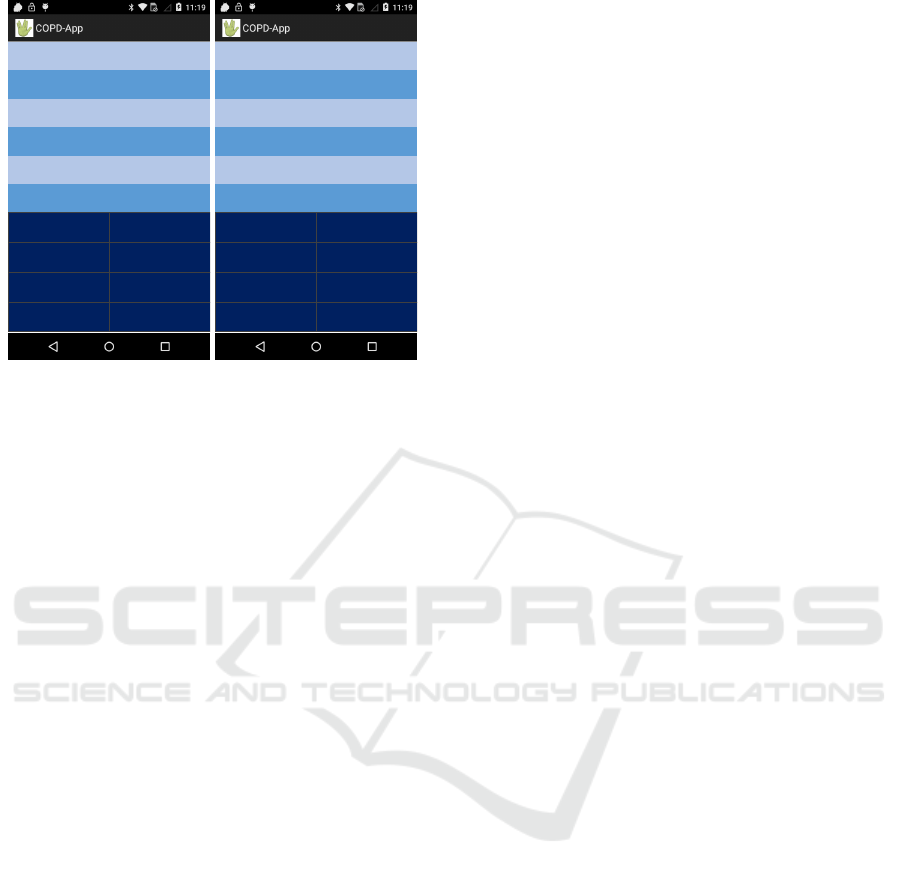
(a) Login Screen (b) Questionnaire
Figure 2: The ChronicOnline App’s Key Functionality.
2013
2
. Within the scope of this project several mHe-
alth apps collect various health data and gather the
data in a Cloud infrastructure. Online services are
available for physicians enabling various data analy-
tic functions and giving them an holistic overview of
their patients’ condition. In addition to it, the patients
and the physicians remain in contact with each other
whereby the physicians can give their patients advices
by sending them messages via their mHealth app. The
ChronicOnline app (Bitsaki et al., 2016) is a mobile
front-end for the ECHO project. Its key functions (user
management and a COPD questionnaire) are shown in
Figure 2.
Initially, the user has to log in his or her account
(see Figure 2a). The app differentiates two user groups,
patients who have only access to their personal account
and physicians who monitor several patients. The login
process is realized by REST calls
3
to the ECHO back-
end.
After authorization is complete, the patient has
access to several tabs. The most significant tab is the
questionnaire tab (see Figure 2b). Here the user has
to answer five questions about his or her condition.
Each question can be answered with ‘yes’ or ‘no’.
Depending on the given answers up to six subquesti-
ons appear to refine the medical finding. Afterwards,
the results are transferred to the back-end as a JSON
object. More details on the data format are given in
Section 4.1.
The back-end performs analyses and preprocesses
the data for physicians. The physicians can contact
their patients via the Amazon Simple Notification Ser-
2
see http://chroniconline.eu
3
see (Fielding, 2000)
The Privacy Management Platform - An Enabler for Device Interoperability and Information Security in mHealth Applications
29

vice (SNS)
4
. These messages are meant for vital issues
(e. g., “Go to the Hospital!”). The discussion of the
medical findings in case of a aggravation still has to
take place in a personal meeting with the physician.
As for both, physicians and patients, the progres-
sion of the health condition is an important informa-
tion, the app can retrieve history data from the back-
end (e. g., to display former questionnaire answers).
For detailed analyses and history charts, especially for
the physicians, the input and output capabilities of a
mobile device are less applicable, which is why cur-
rently such profound reports are stripped off the app
completely.
This app is a representative sample for the innu-
merable COPD apps available in various app stores.
We could use any of them without a loss of argument.
Please note that the back-end is out of this paper’s
scope. More information about the back-end can be
found in (Steimle et al., 2017). However, we give a
brief outlook on a information security mechanism for
the processing of sensitive data in such a back-end in
Section 7.
Applied Metering Devices.
The Vitalograph copd-6
bt
5
is used to screen the pulmonary function. So, pa-
tients with respiratory conditions can perform the me-
tering by themselves. It records various lung function
parameters including the Peak Expiratory Flow (PEF)
and the Forced Expiratory Volume (FEV) among ot-
hers. PEF and FEV are key readings for the diagnosis
of COPD. The measurement results are transmitted via
Bluetooth LE. As today’s Smartphones support this
battery-saving connection standard, the Vitalograph
copd-6 bt provides a sound hardware foundation for
telemedical mHealth apps.
For data interchange the proprietary Terminal I/O
protocol
6
is used which operates on top of Bluetooth
LE GATT
7
. The basic idea behind this protocol is that
a client (e. g., a Smartphone) has to request credits
from the server (i. e., the Vitalograph copd-6 bt). For
each message the client has to pay credits. So, the
client is able to make a specific number of requests
without having to wait for a response from the server.
The application of such proprietary protocols impedes
the development of mHealth apps since only a limited
number of devices supports the respective protocol.
As a common communication standard is not in sight,
app developers are in great need of other approaches
that enhance device interoperability.
4
see https://aws.amazon.com/sns
5
see https://vitalograph.com/product/162427
6
see (Stollmann Entwicklungs- und Vertriebs-GmbH,
2014)
7
see (Bluetooth SIG, Inc., 2017)
3 RELATED WORK
In the context of device interoperability in mHealth
apps, a lot of work is done concerning the back-end
systems. For this purpose, these systems introduced
harmonized data models for health data and provide
generic interfaces so that any kind of mHealth app
can use them to collect and share heath data. One
of the biggest systems is the HealthVault (Bhandari,
2012). It supports various health-related data types ran-
ging from fitness data to entire personal health records.
The HealthVault acts as a middleman between the
data producers—i. e., the mHealth apps—and the data
consumers—i. e., analysis systems. Concerning app-
sided device interoperability and information security,
such a system provides no help. Google Fit (Mishra,
2015) is another back-end for storing and processing
health data. Google’s system deals with fitness data
(e. g., the heart rate), only. Google Fit provides in-
terfaces for app developers which enhance the device
interoperability and facilitate the reading of sensors
in third-party devices—at least for devices that are
supported by Google Wear
8
. As especially medical de-
vices are not supported by Google Wear, (O’Donoghue
and Herbert, 2012) discuss, how Smartphones can be
connected with these devices. However, their solution
aims for physical connections and not for harmonized
communication standards.
(Kouris and Koutsouris, 2014) recommend to use
IoT techniques to solve this problem. In their proposal
all sensors are connected to the Internet and send their
data to a Cloud-based database which is also accessi-
ble for mHealth apps. Even though there are secure
transfer protocols for health data (e. g., (Mare et al.,
2014)), a permanent and unrestricted transmission of
such sensitive data to an unknown server is ineligi-
ble for most users. For that reason, (Gardner et al.,
2009) introduce an approach with which the patient
stays in total control over his or her data; the mHealth
app has full access to the health data while external
services (e. g., apps for physicians) only get access as
long as the patient grants it. In (Murad et al., 2013)
an mHealth app is introduced which relies on a full
encryption of the health data when the data is stored
or transmitted. Yet, both approaches assume that only
external entities constitute a threat for the security of
health data. However, as studies prove, two out of
three apps handle their data either carelessly or even
maliciously (Enck et al., 2010).
Thus, none of these approaches solves the device
interoperability and information security issues of
mHealth apps. Despite the benefit of mHealth apps
especially the device incompatibility and the mis-
8
see https://www.android.com/wear
HEALTHINF 2018 - 11th International Conference on Health Informatics
30

Da il yR epor t {
p a t i e n t I d ( i n t ) : P a t i e n t ID ,
r e c o r d I d ( i n t ) : Re cor d ID ,
d a t e ( s t r i n g ) : Dat e o f R e p ort ,
q1 ( bo o l e a n ) : Answer t o Q u e s t i o n 1 ,
. . .
}
Listing 1: The ChronicOnline Data Model (excerpt).
trust in app developers repel patients from using such
apps (Murnane et al., 2015). For this reason, we intro-
duce a general approach dealing with both issues in
the following sections.
4 INTEROPERABILITY AND
SECURITY REFLECTIONS
In order to come up with a design methodology for
interoperable and secure mHealth apps, a secure data
management, data input techniques, and defined data
access conditions are required. Our solution to this is
built upon the PMP. When looking at the ChronicOn-
line app, it does not take advantage of the full potential
of the ECHO back-end and the prevailing hardware.
With its analytic functions and notification services,
the back-end is able to process more complex data
such as location data or respiratory data in addition to
the replies to the disease-specific questionnaire. By
the integration of medical devices, the ChronicOnline
app becomes a full-fledged telemedicine solution.
Therefore we extend the ChronicOnline app by ad-
ding location services
9
. Studies show that the location
can have a relevant influence on the progression of a di-
sease (Kn
¨
oll and Moar, 2011). Moreover, we provide
support for various third-party Bluetooth respiratory
monitors. The measurement results are added to the
electronic health record (see Section 4.1 for its data
model) and transferred to the ECHO back-end. There,
the data can be automatically pre-analyzed which not
only unburdens the physicians in charge, but also re-
sults in a faster feedback for the patients. As a conse-
quence this enhanced app has to deal with increasing
interoperability and security issues.
Amulet, a tiny Smart Device operating as an infor-
mation hub, tries to solve both problems (Hester et al.,
2016). It confirms the user’s identity and identifies
any available devices in the surrounding belonging to
him or her. Then, Amulet ascertains that only trusted
third-party devices can be used for the metering and
ensures a secure connection to these devices. Moreo-
9
Keep in mind, that location based services in general
constitute a severe threat to a user’s privacy (Marcelino and
Silva, 2018).
Da i l y R e p o r t {
. . .
q5 ( bo o l e a n ) : Answer t o Q u e s t i o n 5 ,
l a t ( i n t ) : L a t i t u d e ,
l o n ( i n t ) : L o n gi t u d e ,
p e f ( i n t ) : Peak E x p i r a t o r y Flow ,
f e v ( i n t ) : F o r c e d E x p i r a t o r y Volume ,
. . .
}
Listing 2: The Extended Data Model (excerpt).
ver, Amulet provides mechanisms to protect the health
data against external attackers. In order to transfer the
data to (trusted) servers for further processing, Amu-
let is able to connect to a Smartphone and use it for
transmission. Unfortunately, this approach has a se-
vere drawback: The user has to possess another device
in addition to his or her Smartphone and the actual
medical device. This causes further costs and it is un-
practical since the user has to carry the Amulet all the
time. The PMP (see Section 4.2) is a middleware for
application platforms which provides similar features.
4.1 The Internal Data Model
The ChronicOnline app sends up to eleven boolean
values, representing the answers to the questionnaire,
to the ECHO back-end. For this reason, its data model
for the data exchange is quite plain (see Listing 1). In
addition to the questionnaire answers, a daily report
entails an ID for the patient and for the report itself as
well as the submission date. Please note that authoriza-
tion data to confirm the identity of the submitter is not
part of this data model. The authorization is managed
via the authorization header of the HTTP protocol.
We add latitude and longitude to this basic schema
to support location data as well as entries for the most
relevant COPD readings, including the Peak Expira-
tory Flow and the Forced Expiratory Volume among
others (see Listing 2).
Since the JSON format is well-suited for the data
exchange between the app and the back-end, but not
for the data processing within the app, we apply wrap-
per classes for the conversion of such JSON files to
Java objects and vice versa.
4.2 Overview of the PMP
We use the PMP in order to realize interoperability and
security features as needed by mHealth apps. We give
a brief overview of the PMP at first and describe in de-
tail the new components, which are developed in this
work in the next section. The PMP is an intermediate
layer between apps and the operating system. It pre-
The Privacy Management Platform - An Enabler for Device Interoperability and Information Security in mHealth Applications
31
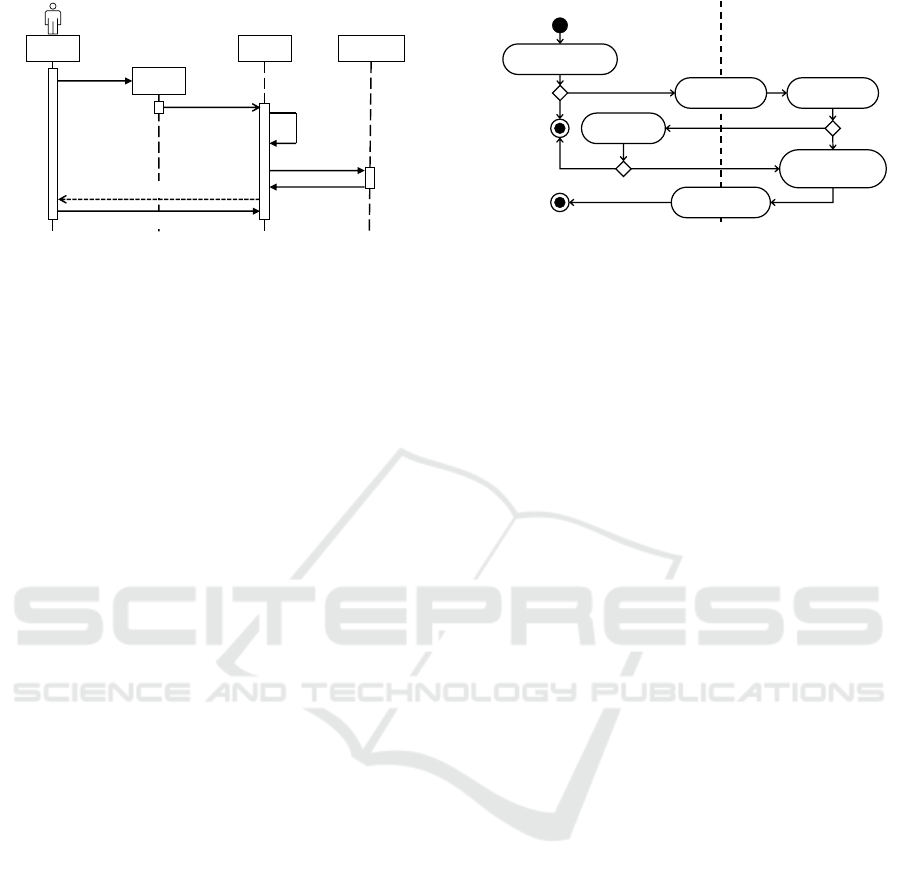
USER
APP
PMP
RESOURCE
REPOSITORY
Install
Register
Determine
Required
Resources
Download
Add Resource
Available Privacy Settings
Initial Policy Rule
Figure 3: The Registration of an App at the PMP.
vents any (potentially malicious) app from accessing
sensitive data.
When an app needs access to such data, it has to ask
the PMP for permission. The PMP operates several
data provisioning services, the so-called Resources.
Each Resource is responsible for a certain type of
data but it is not committed to a certain technology;
e. g., the Location Resource is able to provide location
data from a GPS provider or from a network provider.
Thereby it can adapt its functionality to the available
hardware. In addition to it, the user can define how
accurate the data should be in order to obfuscate his
or her private data. Further Resources can be hooked
into the PMP at runtime need-based.
A Resource defines Privacy Settings which restrict
the usage of the corresponding Resource. By default,
there is a Privacy Setting for granting or permitting
the usage of a Resource. Furthermore, a Privacy Set-
ting can be more specific depending on the type of
Resource. For instance, the Location Resource can
reduce the location’s accuracy.
At installation time an app has to register at the
PMP. The PMP identifies which Resources are requi-
red and installs missing Resources if necessary. The
user then postulates an initial policy rule for this app
defining, which data should be given to the app and
how accurate this data should be. This registration
process is shown in Figure 3.
Since the user is able to deny that an app gets
access to a certain Resource, the app model of the
PMP encapsulates logically coherent parts of the app
in so-called Service Features. So, the withdrawal of
access rights simply deactivates the affected Service
Features but the app itself can still be executed. More-
over, the user can modify access rights of individual
Service Features at runtime. The permission allocation
is shown in Figure 4.
The PMP is primary a fine-grained permission sy-
stem with additional privacy features (e. g., data obfus-
cation). However, in the context of interoperability
and uncertainty of available hardware, the PMP serves
a dual purpose. Each Resource is abstracted from a
Intent to Use
Service Feature
x
[else]
[Service Feature
x
Enabled]
Request
Required Data
Privacy Policy
Lookup
Calculate
Requested Data
(via Resources)
Adjust Policy
Rules
Execute Service
Feature
x
[Access
Permitted]
[Access Granted]
[Access
Granted]
[Access Permitted]
PMPUSER
Service
Feature
x
is
not Available
Service
Feature
x
is Available
Figure 4: The PMP’s Permission Allocation Process.
certain technology and can have several implemen-
tations. As a consequence, the app developer only
has to request a certain type of data (e. g., respiratory
data) and the dedicated Resource ensures that it gets
this data from the available hardware (e. g., a Vitalo-
graph copd-6 bt). If no hardware providing this kind
of data is available—which is similar to a user-defined
prohibition to use the hardware via the PMP—then
the app gets informed and adapts to this condition by
deactivating affected Service Features.
The PMP is able to degrade an app’s functionality
when it cannot access all of its requested data. Services
Features can be deactivate instead of feeding an app
with random data—in the context of mHealth apps, the
usage of random medical values is inappropriate. For
this reason, the PMP’s data obfuscation for health data
is severely restricted. For further details on the PMP,
please refer to the literature (Stach and Mitschang,
2013, Stach, 2013, Stach and Mitschang, 2014, Stach,
2015).
5 DESIGN OF MHEALTH PMP
RESOURCES
In the following we introduce five PMP Resources
which are developed for mHealth apps, namely a se-
cure
authentication
Resource, a
metering
Resource,
a
localization
Resource, a
data storage
Resource, and
a
connection
Resource. In addition, a Resource for he-
alth data
encryption
is introduced. Finally, we revise
the ChronicOnline app with the help of these Resour-
ces.
5.1 The Dialog Box Resource
In the ChronicOnline app a user has to enter creden-
tial information which is sent to an ECHO server for
verification. While the back-end is operated by a trus-
ted organization (e. g., a hospital), any developer can
implement apps for ECHO. Thus the front-end is po-
HEALTHINF 2018 - 11th International Conference on Health Informatics
32

tentially insecure—yet the user has to reveal his or her
login data to it.
In order to solve this problem, we introduce an
isolated Dialog Box Resource. An app can invoke the
dialog box and specify the displayed text as well as
where the entered information should be forwarded to.
The server’s response is sent back to the invoking app.
In this way, the dialog box is completely generic and
can be used in any context where the user has to enter
private data. The dialog box is executed as a part of
the PMP and is completely isolated from the invoking
app. No information is passed to the app except for
the back-end’s reply. The user cannot only grant or
permit the usage of the dialog box, but also specify
which back-ends are legit recipients.
5.2 The Metering Resource
One of the biggest problems for mHealth apps is the
integration of third-party medical devices as there is
currently no uniform standard for intercommunication
with such devices. This is why most of the currently
available apps support some hand-picked medical de-
vice only.
That is why we introduce a Metering Resource with
a simple, yet generic interface. Since most modern
medical devices exchange their data with Smartphones
via a Bluetooth connection, we focus our work on this
kind of connection. As there is no common Bluetooth
transmission protocol, the Metering Resource has to
be able to support several protocols. Currently, the
Terminal I/O protocol is supported. However, further
protocols (e. g., Android Wear) or other connection
standards can be supported in the future due to the mo-
dular expandability of PMP Resources. The Metering
Resource defines no fixed schema for health data, but
processes this data as a JSON object with an attribute
for every measured value.
As the Metering Resource autonomously connects
to any available device, an app developer simply has to
request the health record from the Resource. However,
concerning information security, the app should not be
able to read the health record. Thus, the PMP encrypts
the JSON object containing the health data. As a con-
sequence, authorized Resources can process the health
data while (potentially malicious) apps cannot access
the data. Nevertheless, sometimes an app needs access
to certain values of the health data, e. g., in order to
display the data. For this purpose, the Unsealer Re-
source (see Section 5.6) can be used in order to decrypt
certain excerpts of the record.
The user is able to restrict which devices are al-
lowed to provide health data for a certain app. For
instance, s/he can permit an app to use the Metering
Resource, but only a certain kind of data from a speci-
fic device is sent back by the Resource.
5.3 The Location Resource
Since the location of a reading can be relevant, we in-
troduce a special Location Resource for mHealth apps.
Normally, in Android an app has to subscribe for lo-
cation updates and the system sends any update to the
app. This causes a high battery drain. However, such a
behavior is not necessary in the context of a mHealth
app which requires location data only once after the
metering is executed. As a consequence the Location
Resource supports two modes of operation: An app
can request periodical location updates or only a single
location. The Resource arranges the (un)subscription
automatically. Android supports several location pro-
viders, e. g., a Wi-Fi-based or a GPS. Our Location
Resource requests the most accurate provider which is
currently available.
In order to respect the user’s privacy, the Loca-
tion Resource provides a Privacy Setting to reduce the
accuracy of the location data. The user sets a maxi-
mum accuracy in meters. If the provided location data
is more accurate, the Resource adds a random factor
depending on the user settings to the latitude and lon-
gitude in order to reduce the accuracy. The user is also
able to use completely randomized or mocked location
data.
5.4 The Secure Database Resource
Since Android stores its data in a clear-text reada-
ble form, attackers may harvest all stored data. The
file system encryption is no solution for this threat,
since the data is decrypted as soon as the system is
fully booted. So, sensitive data such as health data
requires additional security features. The
S
ecure
D
ata
C
ontainer (SDC) is a Secure Database Resource for
the PMP (Stach and Mitschang, 2016). It encrypts
the stored data with AES-
256
encryption and only the
PMP has the key. The SDC has a fine-grained access
control to share the stored data with selected apps. Per-
formance measurements show that the thereby caused
overhead is within reasonable limits.
We tailor the SDC slightly to our requirements:
The database’s internal data model is comparable to a
key-value store. The Secure Database Resource opera-
tes with JSON objects and adopts the therein defined
keys and values directly. As several stored JSON ob-
jects can use a common key, an internal id is applied
to each object. The database’s primary key consists
of the internal id and the key from the JSON object.
The Database Resource’s interface is minimalistic, yet
The Privacy Management Platform - An Enabler for Device Interoperability and Information Security in mHealth Applications
33
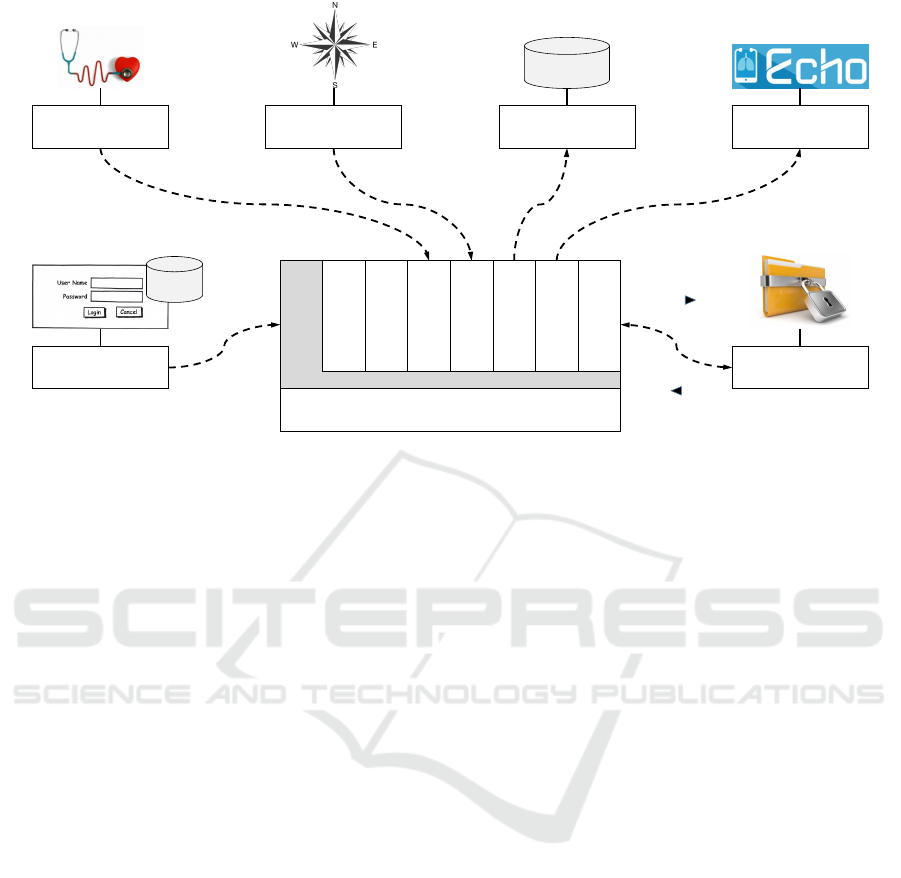
Revised ChronicOnline App
Login SF
Respiratory SF
Location SF
Storage SF
Transfer SF
Display Data SF
Questionnaire SF
Message SF
Dialog Box Resource
Metering Resource
Location Resource Database Resource Connector Resource
Unsealer Resource
Internal
Storage
Account
DB
Sealed Health RecordSealed Health RecordLocation Data
Access Token
Unsealed Excerpt
Sealed Health Record
Sealed
Health Record
Figure 5: Relations Between the Service Features of the COPD App and the PMP Resources.
demand-actuated. A JSON object can be stored, obtai-
ned, and deleted via its key.
5.5 The Connector Resource
Nowadays, most apps do not only operate locally on
a single Smartphone, but include various external ser-
vices. This is why almost every app requests the per-
mission to establish a network connection. The user is
not even informed about this request. However, an app
having this permission is able to upload sensitive data
to any server. To use external services in a secured
way, we introduce the Connector Resource. Within
the Connector Resource various trusted external ser-
vices are specified. An app is able to either upload
data to or retrieve data from one of these services (e. g.,
the ECHO back-end or Amazon’s SNS). Additional
domain-specific information protection policies can be
applied within the Connector Resource (such as the
Mobile access to Health Documents profile (Moehrke,
2017b) or the Audit Trail and Node Authentication
profile (Moehrke, 2017a)), if they are supported by the
back-end.
Concerning interoperability, the Connector Re-
source handles any interface changes of the external
services for the apps. That is, adjustments have to be
made only at the Resource and not for every app. Addi-
tionally, the app’s network access is heavily restricted.
It is only able to use the Resource’s interface and the
user can block any external services s/he has no trust
in.
5.6 The Unsealer Resource
As mentioned above, health data gets encrypted by the
PMP before it is passed to an app. So, apps cannot
access this sensitive data directly. As health data is
only processed in Resources, this encryption means no
limitation for the user (cf. (Weerasinghe et al., 2009)).
If an app still needs access to health data (e. g., to
display it), we introduce the Unsealer Resource which
decrypts selected values. The user is able to define
which excerpt of the data should be revealed. To that
end, the Resource provides a domain-specific selection
(e. g., general information, lung-related content only,
etc.) in order to facilitate the configuration.
5.7 Revised ChronicOnline App
Based on these Resources, we revise the Chronic-
Online app by including sensor data (e. g., respiratory
meters or location sensors) while regarding device in-
teroperability and information security.
After the user has answered the questionnaire, the
revised app expects respiratory data from a connected
device via the Metering Resource. The user only has
to push the “Lung Monitor” button and the connection
and data transfer is arranged automatically by the PMP.
When the measured data is available, the results of
the questionnaire are applied to the DailyReport (see
Listing 2) and the location data is inquired. Then, the
complete DailyReport object is stored internally (e. g.,
if the data cannot be transmitted immediately) and is
transferred subsequently to the ECHO back-end (see
Figure 6a). Please note, that for this capture any data
HEALTHINF 2018 - 11th International Conference on Health Informatics
34
Device ID:
0000167630
PEF:
333
FEV075:
3.83
FEV1:
4.47
FEV10:
591
F1/F10:
76 %
FEF2575:
3.97
Date:
20
-08-
15
Time:
13:49:23
Lat
:
48.75
Lon:
9.11
Reset Message Box
History Transfer Data
Lung Monitor Location
Unseal Questionaire
(a) Unsealed Data Screen
Device ID:
0000167630
PEF:
N/A
FEV075:
N/A
FEV1:
N/A
FEV10:
N/A
F1/F10:
N/A
FEF2575:
N/A
Date:
20
-08-
15
Time:
13:49:23
Lat
:
48.75
Lon:
9.11
Reset Message Box
History Transfer Data
Lung Monitor Location
Unseal Questionaire
(b) Sealed Data Screen
Figure 6: The ChronicOnline Privacy-Driven App.
is unsealed for demonstration purpose. The user is
informed in each step about the collected data. So,
s/he is in total control over the data. The effect of a
deactivated Unsealer Resource is shown in Figure 6b.
Without the Unsealer Resource only data which are
not related to any health issues are known to the app.
In order to react properly to the restriction of a
Resource, an app needs to define Service Features.
Figure 5 shows the
8
Service Features of the revised
ChronicOnline App (denoted as SF) and which Re-
sources are required for each of them. Not every Ser-
vice Feature necessarily requires data from a Resource
(e. g., the Questionnaire SF). The Service Features
have a modular design and can be plugged in and out
at runtime (e. g., when the corresponding Resource is
deactivated). In the app’s program flow these features
are skipped. However, since the authentication of the
user is mandatory, the Login SF and therewith the Di-
alog Box Resource cannot be deactivated or else any
other Service Feature is also deactivated.
6 ASSESSMENT
Concerning information security, the literature speaks
of
7
key protective goals, namely auditability, au-
thenticity, availability, confidentiality, integrity, non-
repudiation, and privacy (Dhillon and Backhouse,
2000, Cherdantseva and Hilton, 2013). The original
ChronicOnline app only fulfills the authenticity goal
and the confidentiality goal directly due to its login
mechanism and the auditability goal, the integrity goal,
and the non-repudiation server-sided due to the se-
curity mechanism of the ECHO back-end. However,
as soon as real health data is processed by the app,
the user cannot rely on the prevailing mechanisms.
Our revised app supports all
7
protective goals due to
the used Resources. The auditability as well as the
non-repudiation is guaranteed, since the PMP logs any
Resource access of an app. The authenticity is given
via the login mechanism and since the login data is
not shared with the app, it cannot commit an identity
theft. The availability is given, as all data is stored on
the device using mature database technologies. The
confidentiality is ensured, since any app functionality
is only usable after the login process is completed.
The integrity is guaranteed since any relevant data
is encrypted and therefore cannot be manipulated by
third-parties. Privacy is retained, as the user decides,
which data can be used by an app and s/he can specify
for any non-health data how accurate or even rando-
mized it should be provided. As an app cannot access
any data without using the PMP, data access is strictly
constrained by the Resources’ interfaces. Thus, from
an information security’s point of view the revised app
satisfies all requirements.
Concerning device interoperability, the modular ex-
pandability of the Resources turns out to be beneficial.
For instance, support for additional devices can be ad-
ded to the Metering Resource need-based at runtime.
An app developer only has to code against a Resource’s
interface, no matter which hardware is actually avai-
lable. Therefore, complex and labor-intensive coding
is required only once (for the Resource) and it can be
reused many times (in the apps). Additionally, due to
their generic design the Resources are usable in many
different application scenarios even for non-mHealth
apps. Thus, from an interoperability’s point of view
the PMP Resources satisfy all requirements regarding
compatibility and reusability. Table 1 lists the key
contributions of the introduced Resources.
7 CONCLUSION AND OUTLOOK
The rising numbers of patients suffering from chro-
nic diseases are responsible for increasing treatment
costs as well as overburdened physicians. The usage
of a combination of Smartphones with medical devi-
ces, commonly referred to as mHealth, can provide
a remedy for this situation. Apps realizing the data
interchange between the Smartphone and the medical
device can be used autonomously by the patients for
telemedical screening of their condition. Unfortuna-
tely, these mHealth apps face two key challenges, na-
mely information security and device interoperability.
Each mHealth app has to reinvent the wheel concer-
ning these two issues. So, the development effort for
mHealth apps is unnecessary high and the quality of
The Privacy Management Platform - An Enabler for Device Interoperability and Information Security in mHealth Applications
35
Table 1: Feature Summary of the Resources Concerning Device Interoperability and Information Security Issues.
PMP Resource Device Interoperability Information Security
Dialog Box Resource
•
displayed dialog text can be tailored
to the app
•
entered data is not revealed to the app
•
evaluation mechanism can be substitu-
ted
Metering Resource
• support of different medical devices • data is transmitted encrypted
•
support of different transmission stan-
dards
• restriction of usable device types
Location Resource
• support of different location sensors • restriction of location accuracy
•
support of different modes of opera-
tion
• use of randomized location data
Database Resource • generic data model • full database encryption
Connector Resource
• support of different external services •
no dircet access to the network for the
app
• restriction of usable services
Unsealer Resource
•
all authorized Resources get unencryp-
ted data
•
apps have only limited access to health
data
information security and device interoperability featu-
res differs strongly from app to app. As mHealth apps
deal with sensitive data, a consistently high service
quality is badly required.
For this reason, we pursue four key objectives with
our work:
(I)
We analyze the ChronicOnline app re-
garding the collected data and used devices.
(II)
We
deduce a generic data model for mHealth apps from
this app.
(III)
We identify five recurring tasks within
mHealth apps for which device interoperability and
information security are key requirements. For each
of these tasks, we introduce a PMP Resource. Each
Resource is designed regarding device interoperability
and information security issues.
(IV )
We use these
extensions to revise the ChronicOnline app. With this
revised app, we assess the practical effect of our appro-
ach. Although our approach is based on Android, the
underlying concept can be applied to any application
platform.
As the evaluation results in Section 6 show, our ap-
proach meets the requirements of mHealth apps. Yet,
this is just a first protective measure. Modern Smartp-
hone applications commonly serve as data sources for
comprehensive stream processing systems realizing
the actual computation. These systems have access
to a wide range of sources. With the help of such
comprehensive stream processing systems, a lot of
knowledge about the patients can be derived. Even if a
user restricts access to a certain type of data on his or
her device, a stream processing system could be able
to retrieve this data from another source. Therefore
the privacy rules of each application also have to be
applied to affiliated services which process the appli-
cation’s data. Future work has to investigate, how the
PMP settings concerning information security can be
applied to a privacy mechanism for stream processing
systems such as the PATRON research project
10
(Stach
et al., 2017).
ACKNOWLEDGEMENTS
This paper is part of the PATRON research project
which is commissioned by the Baden-Wrttemberg Stif-
tung gGmbH. The authors would like to thank the
BW-Stiftung for the funding of this research.
10
see http://patronresearch.de
HEALTHINF 2018 - 11th International Conference on Health Informatics
36

REFERENCES
Bai, Y., Dai, L., and Li, J. (2014). Issues and Challenges in
Securing eHealth Systems. International Journal of
E-Health and Medical Communications, 5(1):1–19.
Bhandari, V. (2012). Enabling Programmable Self with
HealthVault. O’Reilly Media, Inc., Beijing, Cambridge,
Farnham, K
¨
oln, Sebastopol, Tokyo.
Bitsaki, M., Koutras, C., Koutras, G., Leymann, F., Steimle,
F., Wagner, S., and Wieland, M. (2016). ChronicOn-
line: Implementing a mHealth solution for monitoring
and early alerting in chronic obstructive pulmonary
disease. Health Informatics Journal, 23(3):197–207.
Bluetooth SIG, Inc. (2017). GATT Specifications.
https://www.bluetooth.com/specifications/gatt.
Chan, M., Est
`
eVe, D., Fourniols, J.-Y., Escriba, C., and
Campo, E. (2012). Smart Wearable Systems: Current
Status and Future Challenges. Artificial Intelligence in
Medicine, 56(3):137–156.
Cherdantseva, Y. and Hilton, J. (2013). A Reference Model
of Information Assurance & Security. In Proceedings
of the 2013 International Conference on Availability,
Reliability and Security, ARES ’13, pages 546–555.
de Toledo, P., Jimenez, S., del Pozo, F., Roca, J., Alonso, A.,
and Hernandez, C. (2006). Telemedicine Experience
for Chronic Care in COPD. IEEE Transactions on
Information Technology in Biomedicine, 10(3):567–
573.
Dhillon, G. and Backhouse, J. (2000). Technical Opinion:
Information System Security Management in the New
Millennium. Communications of the ACM, 43(7):125–
128.
Enck, W., Gilbert, P., Chun, B.-G., Cox, L. P., Jung, J.,
McDaniel, P., and Sheth, A. N. (2010). TaintDroid:
An Information-Flow Tracking System for Realtime
Privacy Monitoring on Smartphones. In Proceedings
of the 9
th
USENIX Conference on Operating Systems
Design and Implementation, OSDI ’10, pages 393–
407.
Fielding, R. T. (2000). Architectural Styles and the Design
of Network-based Software Architectures. PhD thesis,
University of California, Irvine.
Gardner, R. W., Garera, S., Pagano, M. W., Green, M., and
Rubin, A. D. (2009). Securing Medical Records on
Smart Phones. In Proceedings of the First ACM Works-
hop on Security and Privacy in Medical and Home-
care Systems, SPIMACS ’09, pages 31–40.
Hester, J., Peters, T., Yun, T., Peterson, R., Skinner, J., Golla,
B., Storer, K., Hearndon, S., Freeman, K., Lord, S.,
Halter, R., Kotz, D., and Sorber, J. (2016). Amulet:
An Energy-Efficient, Multi-Application Wearable Plat-
form. In Proceedings of the 14
th
ACM Conference on
Embedded Network Sensor Systems, SenSys ’16, pages
216–229.
Jafari, M., Safavi-Naini, R., and Sheppard, N. P. (2011). A
Rights Management Approach to Protection of Privacy
in a Cloud of Electronic Health Records. In Procee-
dings of the 11
th
Annual ACM Workshop on Digital
Rights Management, DRM ’11, pages 23–30.
Kn
¨
oll, M. and Moar, M. (2011). On the Importance of Locati-
ons in Therapeutic Serious Games: Review on current
health games and how they make use of the urban
landscape. In Proceedings of the 2011 5
th
Internatio-
nal Conference on Pervasive Computing Technologies
for Healthcare and Workshops, PervasiveHealth ’11,
pages 538–545.
Kouris, I. and Koutsouris, D. (2014). Identifying Risky
Environments for COPD Patients Using Smartphones
and Internet of Things Objects. International Journal
of Computational Intelligence Studies, 3(1):1–17.
Kumar, S., Nilsen, W., Pavel, M., and Srivastava, M. (2013).
Mobile Health: Revolutionizing Healthcare Through
Transdisciplinary Research. Computer, 46(1):28–35.
Marcelino, L. and Silva, C. (2018). Location Privacy Con-
cerns in Mobile Applications, pages 241–249. Springer,
Cham.
Mare, S., Sorber, J., Shin, M., Cornelius, C., and Kotz, D.
(2014). Hide-n-Sense: Preserving Privacy Efficiently
in Wireless mHealth. Mobile Networks and Applicati-
ons, 19(3):331–344.
Mattila, E., Korhonen, I., Salminen, J. H., Ahtinen, A., Ko-
skinen, E., S
¨
arel
¨
a, A., P
¨
arkk
¨
a, J., and Lappalainen, R.
(2010). Empowering Citizens for Well-being and Chro-
nic Disease Management with Wellness Diary. IEEE
Transactions on Information Technology in Biomedi-
cine, 14(2):456–463.
Milo
ˇ
sevi
´
c, M., Shrove, M. T., and Jovanov, E. (2011). Ap-
plications of Smartphones for Ubiquitous Health Mo-
nitoring and Wellbeing Management. Journal of Infor-
mation Technology and Applications, 1(1):7–15.
Mishra, S. M. (2015). Wearable Android: Android Wear and
Google FIT App Development. Wiley Online Library,
Hoboken, New Jersey.
Moehrke, J. (2017a). Audit Trail and Node Au-
thentication. Technical report, IHE International.
https://wiki.ihe.net.
Moehrke, J. (2017b). Mobile access to Health Docu-
ments (MHD). Technical report, IHE International.
https://wiki.ihe.net.
Murad, A., Schooley, B., and Abed, Y. (2013). A Secure
mHealth Application for EMS: Design and Implemen-
tation. In Proceedings of the 4
th
Conference on Wire-
less Health, WH ’13, pages 15:1–15:2.
Murnane, E. L., Huffaker, D., and Kossinets, G. (2015). Mo-
bile Health Apps: Adoption, Adherence, and Abandon-
ment. In Adjunct Proceedings of the 2015 ACM Inter-
national Joint Conference on Pervasive and Ubiquitous
Computing and Proceedings of the 2015 ACM Interna-
tional Symposium on Wearable Computers, UbiCom-
p/ISWC ’15 Adjunct, pages 261–264.
O’Donoghue, J. and Herbert, J. (2012). Data Management
Within mHealth Environments: Patient Sensors, Mo-
bile Devices, and Databases. Journal of Data and
Information Quality, 4(1):5:1–5:20.
Schweitzer, J. and Synowiec, C. (2012). The Economics of
eHealth and mHealth. Journal of Health Communica-
tion, 17(Supplement 1):73–81.
Siewiorek, D. (2012). Generation Smartphone. IEEE
Spectrum, 49(9):54–58.
The Privacy Management Platform - An Enabler for Device Interoperability and Information Security in mHealth Applications
37

Silva, B. M., Rodrigues, J. J., de la Torre D
´
ıez, I., L
´
opez-
Coronado, M., and Saleem, K. (2015). Mobile-health:
A Review of Current State in 2015. Journal of Biome-
dical Informatics, 56(C):265–272.
Stach, C. (2013). How to Assure Privacy on Android Phones
and Devices? In Proceedings of the 2013 IEEE 14
th
In-
ternational Conference on Mobile Data Management,
MDM ’13, pages 350–352.
Stach, C. (2015). How to Deal with Third Party Apps in a Pri-
vacy System — The PMP Gatekeeper. In Proceedings
of the 2015 IEEE 16
th
International Conference on
Mobile Data Management, MDM ’15, pages 167–172.
Stach, C., D
¨
urr, F., Mindermann, K., Palanisamy, S. M., Ta-
riq, M. A., Mitschang, B., and Wagner, S. (2017). PA-
TRON — Datenschutz in Datenstromverarbeitungssys-
temen. In Informatik 2017: Digitale Kulturen, Ta-
gungsband der 47. Jahrestagung der Gesellschaft f
¨
ur
Informatik e.V. (GI), 25.9-29.9.2017, Chemnitz, volume
275 of LNI, pages 1085–1096. (in German).
Stach, C. and Mitschang, B. (2013). Privacy Management
for Mobile Platforms – A Review of Concepts and
Approaches. In Proceedings of the 2013 IEEE 14
th
In-
ternational Conference on Mobile Data Management,
MDM ’13, pages 305–313.
Stach, C. and Mitschang, B. (2014). Design and Implemen-
tation of the Privacy Management Platform. In Procee-
dings of the 2014 IEEE 15
th
International Conference
on Mobile Data Management, MDM ’14, pages 69–72.
Stach, C. and Mitschang, B. (2016). The Secure Data Con-
tainer: An Approach to Harmonize Data Sharing with
Information Security. In Proceedings of the 2016 IEEE
17
th
International Conference on Mobile Data Mana-
gement, MDM ’16, pages 292–297.
Steimle, F., Wieland, M., Mitschang, B., Wagner, S., and
Leymann, F. (2017). Extended provisioning, security
and analysis techniques for the ECHO health data ma-
nagement system. Computing, 99(2):183–201.
Stollmann Entwicklungs- und Vertriebs-GmbH (2014). Ter-
minal I/O Profile: Client implementation guide. Techni-
cal report, Telit.
Weerasinghe, D., Rajarajan, M., and Rakocevic, V. (2009).
Device Data Protection in Mobile Healthcare Applica-
tions, pages 82–89. Springer, Berlin, Heidelberg.
HEALTHINF 2018 - 11th International Conference on Health Informatics
38
