
A Real-time m-Health Monitoring System: An Integrated Solution
Combining the Use of Several Wearable Sensors and Mobile Devices
Salvatore Naddeo
1
, Laura Verde
2
, Manolo Forastiere
3
, Giuseppe De Pietro
1
and Giovanna Sannino
1
1
Institute of High Performance Computing and Networking (ICAR), National Research Council of Italy (CNR),
via Pietro Castellino 111, 80131 Naples, Italy
2
Department of Technology, University of Naples Parthenope, 80143 Naples, Italy
3
Neatec S.p.a. R&D Support, Via Campi Flegrei 34, 80078 Pozzuoli, Italy
Keywords:
Physiological Monitoring, Wearable Device, m-Health System, Continua Alliance Guidelines, Chronic
Diseases.
Abstract:
Nowadays the upsurge in the prevalence of chronic diseases represents an increasing burden on individuals
and society. Chronic diseases can require repeated and frequent hospital treatment to control vital parameters
of interest. The use of automatic instruments for a real-time monitoring of biological parameters constitutes
a valid instrument to improve the patient’s quality of life. The integration of mobile communications with
wearable devices has facilitated the shift of healthcare assistance from clinic-centric to patient-centric mon-
itoring. In this paper, a real-time monitoring system is proposed. The system is conceptualized to provide
an instrument for patients, by means of which they can easily monitor, analyse and save their own vital signs
using wearable sensors and an Android device such as a smartphone or tablet, offering an efficient solution in
terms of a decrease in time, human error and cost.
1 INTRODUCTION
During the recent decade the demographic changes in
developed countries resulting in a more elderly pop-
ulation and the increasing prevalence of chronic dis-
eases have contributed to the need for a constant mon-
itoring of the state of patients’ health.
According to the World Health Organization
(World Health Organization, 2016), chronic diseases
such as coronary heart disease, cancer, chronic ob-
structive pulmonary disease and diabetes mellitus
type 2 constitute the leading cause of mortality in the
world, representing about 60% of all deaths. Chronic
diseases are primarily attributable to heart failure, cur-
rently the main cause of death in most western coun-
tries. The 2016 Heart Disease and Stroke Statistics
update of the American Heart Association (AHA)
reported that 15.5 million people in the USA suf-
fer from cardiovascular disease, this prevalence in-
creasing with age for both women and men (Sanchis-
Gomar et al., 2016). In Europe, in the last 12 months
the prevalence of people reporting heart problems
was 9.2% for both sexes (Townsend et al., 2016).
In particular, in Italy cardiovascular diseases are the
main cause of death, responsible for 44% of all
deaths (Centro nazionale di epidemiologia, sorveg-
lianza e promozione della salute dell’Istituto superi-
ore di sanit
`
a, 2016).
Chronic diseases also have a negative impact on
the quality of people’s life. Patients suffering from
these pathologies must, often, carry out a monitor-
ing of physiological parameters such as heart rate and
blood pressure as well as take control of the main
risk factors that can aggravate their state of health. In
less dangerous cases, it is convenient to monitor pa-
tients outside the hospital. On the one hand,in fact,
such patients can face their illness in a family con-
text that helps to speed up their recovery time. On
the other, this strategy implies a considerable saving
of resources, allowing social health facilities and per-
sonnel to be assigned to patients with more severe dis-
eases.
Therefore, an efficient solution for the monitor-
ing of a patients’ state of health is required, which
is able to collect, record and analyse vital signs, and
so support preventive care, diagnosis and rehabilita-
tion planning. Moreover, the automation of physio-
logical data capture and its visualisation on a device
Naddeo S., Verde L., Forastiere M., De Pietro G. and Sannino G.
A Real-time m-Health Monitoring System: An Integrated Solution Combining the Use of Several Wearable Sensors and Mobile Devices.
DOI: 10.5220/0006296105450552
Copyright
c
2017 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

reduces the risk of errors in manual harvesting. This
lower risk of error results in increased efficiency, re-
duced costs and improved vital qualities in an area
such as healthcare one where human error can really
make the difference between life and death. The most
innovative aspect of the adoption of a tele-monitoring
system is represented by the means by which patients
and healthcare professionals communicate and inter-
act. Patients are directly involved in managing their
health and wellness.
Mobile devices, such as smartphones or tablets,
constitute the perfect instrument to monitor the vital
parameters of a patient. Thanks to the use of appro-
priate wearable sensors, it is possible to collect and
analyse the data coming from these devices to moni-
tor the patient’s state of health.
In this work we present a real-time m-health mon-
itoring system for people suffering from chronic dis-
eases that enables the collection, sharing and ex-
change of physiological data, such as blood pressure,
heart and respiration rate and ECG signals. The sys-
tem is not limited only to the acquisition of such data
but also enables the analysis of vital signs. The phys-
iological data are captured using wearable systems
compliant and not to Continua Health Alliance guide-
lines (Carroll et al., 2007), one of the most respected
communication standardization protocol.
2 RELATED WORK
Mobile healthcare applications constitute an instru-
ment for individuals to keep track of their health con-
dition, to take more responsibility for their lifestyle
and to improve the efficiency of care by providing
high quality data to health professionals. Such med-
ical data are often acquired by means of the use of
wearable devices. Interest in the research and devel-
opment of smart wearable systems is increasing in
both the academic world and industry, to promote the
realization of devices that comply with the required
standards of effectiveness, interoperability, cost, pri-
vacy and ethics (Lmberis and Dittmar, 2007; Konstan-
tas, 2007; Chan et al., 2012). These systems are able
to measure vital signs, such as body and skin temper-
ature, heart rate, blood pressure, blood oxygen sat-
uration (SpO2), electrocardiograms (ECG), electron-
cephalograms (EEG) and respiration rate.
To implement an m-health solution a level of stan-
dardization is necessary to ensure an easy and quick
integration between the wearable device (e.g. a blood
pressure monitor or pulse-oximeter) and the gateway
device (e.g. a smartphone). The interoperability
among all devices that compose a telehealth system
is regulated by the guidelines of the Continua Health
Alliance.is necessary which describe a set of interna-
tionally established standards and frameworks to en-
sure interoperability of devices (Carroll et al., 2007).
Several examples of monitoring systems are de-
scribed in literature useful for the monitoring of phys-
iological data taken from wearable devices. Unfor-
tunately, not all the presented systems use devices
that follow the Continua Health Alliance guidelines.
Kakria et al. (Kakria et al., 2015), for example, pro-
pose a real-time monitoring system to collect data
about heart rate, blood pressure and body tempera-
ture using wearable devices non-compliant with the
Continua Health Alliance guidelines. The same lim-
itation applies to the device used by PhysioDroid
(Banos et al., 2014), a mobile system to monitor
heart rate, body temperature and respiration rate, and
to the system realized by Forastiere et al.(Forastiere
et al., 2016) for a monitoring of a patient’s own well-
ness. The proposed system, instead, supports devices
compatible with the Continua Health Alliance design
Guidelines. In addition, the open architecture of our
framework allows an integration with wearable de-
vices that use other communication and data access
protocols to provide a system that can monitor pa-
tients integrating data coming from several medical
devices, unlike the system proposed by (Park et al.,
2016). They develop an m-health application limit-
ing the integration to only certified devices. While,
Szydlo et al (Szydło and Konieczny, 2016) present a
data acquisition module, implemented as a mobile ap-
plication to integrate several medical devices, whether
or not compliant or not with the Continua Health Al-
liance guidelines, but without analysing the acquired
data.
Many mobile healthcare systems are aimed at
patients with cardiac diseases, diabetes, hyperten-
sion, or hyperthermia, limiting the acquisition and
monitoring to only one set of physiological data, and
sometimes providing an analysis such as (Gay and
Leijdekkers, 2007; Lv et al., 2010; Rodrigues et al.,
2014; Guo et al., 2013; Lee et al., 2016), Sense-
View (http://www.senseview.mobi/), and SimpleEye
(https://simpleeye.com/platforms/android/bluetooth-
pulse-oximeter/). Our proposed system, however,
is not limited to capturing and monitoring in real
time vital signs but also to allows data processing
and analysis locally, to better evaluate whether health
activities have been performed planned and to assess
whether the desired results are being achieved.
Moreover, in literature there are platforms that
collect the physiological data and send it to a care
center for processing and analysis. These solutions
do not process the medical data locally on mobile de-
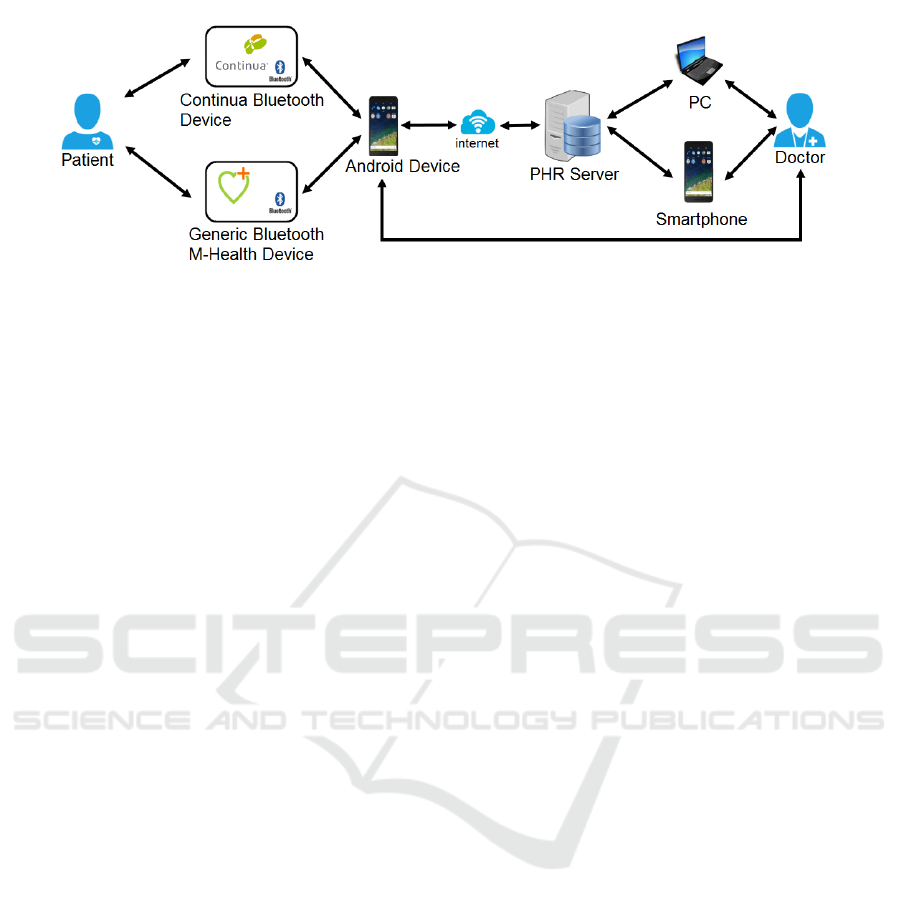
Figure 1: System Structure.
vice, but the signal needs to be continuously trans-
ferred to a health center. For example, the Euro-
pean Union-funded research project AMON (Anliker
et al., 2004) has an objective realizing a wrist-worn
medical monitoring and alert system. The data are
transmitted via GSM to a medical center. Unfortu-
nately, for heart monitoring the system is technically
limited by the noisy ECG signal that is acquired on
the wrist through the realized device and is not ap-
propriate for the diagnosis of cardiac abnormalities.
The Epi-medics project (Rubel et al., 2005) is another
project for ECG monitoring that records and analyses
ECG signals and generates alarms. In this case, also,
the monitoring system uses its own sensor device, not
interfaced with other sensor devices. Bisio et al. (Bi-
sio et al., 2015), instead, proposed a platform for pa-
tients suffering from a heart failure, able to monitor
data coming from the pulse oximeter to measure the
saturation of peripheral oxygen and a weighting scale
to measure the body weight, using devices compliant
with the Continua Health Alliance standards. More-
over, Al-Taee et al.(Al-Taee et al., 2015) present a
platform to support the self-management of diabetes
using several medical sensors which are not compli-
ant the guidelines.
3 MONITORING SYSTEM
The proposed system is able to monitor several health
parameters using multiple sensors. The acquired
physiological data are processed and analysed locally
on a mobile device. A report of the analysis and the
original files are saved, can be visualized whenever
the user wants and are sent to the medical specialist.
The scheme in the figure 1 shows the structure of
the system, a set of interconnected blocks in which
the data flows start from the patient and arrive at the
medical specialist. A patient can monitor his/her own
vital signs using an Android device, which is easy to
use and able to capture and store the data from the
wearable sensors. Once the acquisition has been com-
pleted, the Android device sends the data to a remote
Personal Health Record (PHR) server, which the doc-
tor can access to monitor the patient’s health state. In
the following section the system architecture is ex-
plained in detail.
3.1 System Architecture
The system has a modular structure, in which ev-
ery module performs a specific set of operations, as
shown in the figure 2.
The Health Device Profile (HDP) module is re-
sponsible for the transmission of data from the wear-
able devices to the mobile devices using the Blue-
tooth protocol. Moreover, it is possible to connect
the proposed system with an external PHR, as shown
in the figure 1, and/or Decision Support Systems. In
the interaction with these systems, the adoption of
the Continua Alliance standard, using an appropri-
ate wrapper, allows a fast and accurate data trans-
lation in accordance with the two Health Level 7
standards (http://www.hl7.org/implement/standards):
Fast Healthcare Interoperability Resources (FHIR)
and Personal Healthcare Monitoring Report (PHMR).
The FHIR Standard (Bender and Sartipi, 2013) is use-
ful to represent and exchange information between
several types of monitoring devices, for a correct syn-
tactic and semantic interoperability and appropriate
efficiency between information systems and biomed-
ical devices. Moreover, in order to improve the
data dissertation in a tele-monitoring application, the
PHMR (Wolf et al., 2009) was introduced, which is
able to translate personal healthcare monitoring infor-
mation into electronic medical record systems includ-
ing a representation of the measurements captured.
The data, that are received by the HDP module,
will be forwarded to the other modules connected
with it, the Storage module and the Signal Analysis
module. The first one is used to save physiological
data and a patient’s analysis report in the device in-
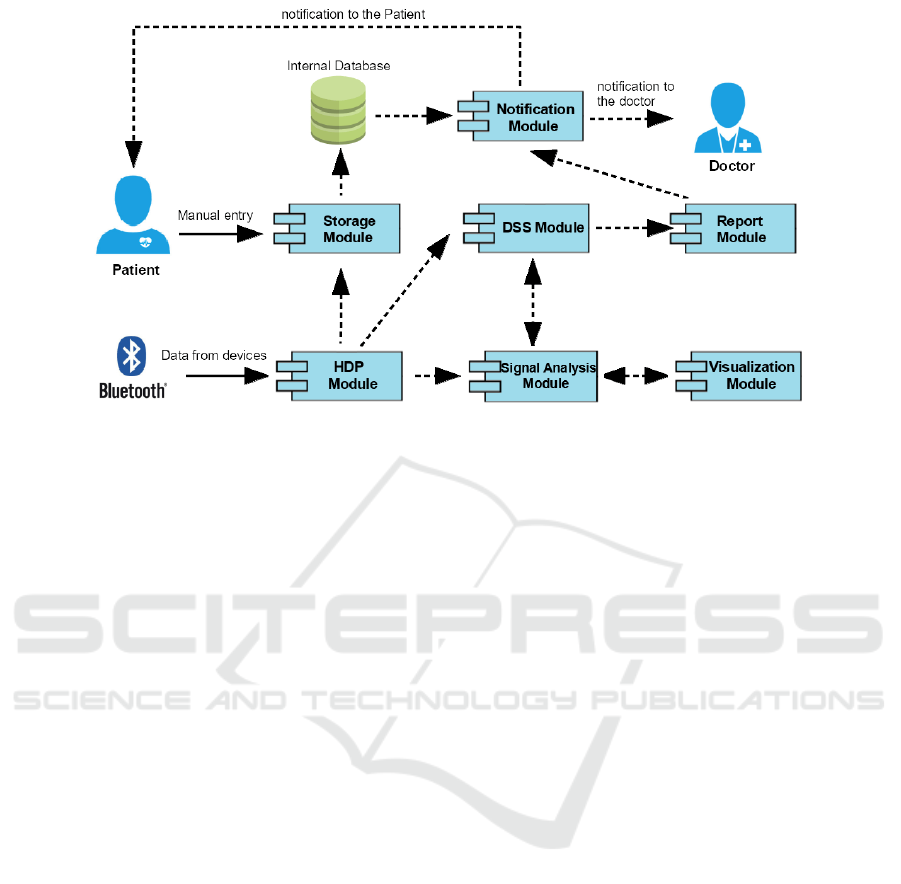
Figure 2: System Architecture.
ternal memory. SQLite database is used to store mea-
surement data acquired from the mobile health device
and/or data from manual measurement that the patient
performs with devices not equipped with a Bluetooth
connection. In the first case, the Storage Module re-
ceives data from the HDP Module, while in the sec-
ond the data are directly inserted by the user. Col-
lected and analysed data, during the monitoring, con-
stitute the Personal Health Record (PHR) of the pa-
tient (Tang et al., 2006). To access the data contained
in the PHR the doctor, through appropriate devices,
must interact with a remote server to visualize any de-
sired data. This operation is fundamental when there
are anomalies that generate an alert. In this situa-
tion the specialist visualizes all the patient’s measure-
ments and can decide to change the therapy, perform
in depth examinations or modify the monitoring plan.
The monitored data, besides being saved, can be
analyzed, using the Signal Analysis Module. In de-
tail,such analysis can include:
• Filtering data to remove the additive noise that
can distort the signal and the resulting interpre-
tation. It is possible to choose between four types
of filter: high-pass and low-pass (Chen and Chen,
2003), recursive (Cuomo et al., 2016) and Han-
ning filters (Verde et al., 2015). The implemented
filters are characterized by appropriate parameters
such as the cut-off frequency that the user can set
indicating the desirable value;
• Data processing, whereby the signals can be anal-
ysed to extract characteristic parameters, useful to
evaluate the patient’s health state.
Data obtained from the HDP and Signal Analy-
sis modules are sent to the DSS Module. This mod-
ule constitutes the Decision Support System, apable
of supporting and improving the real-time monitoring
and analysis using ”the medical specialist’s knowl-
edge”. The data are, in fact, compared with selected
threshold values to check the patient’s state of health.
If the module discovers a warning situation, it asks
the Report Module to generate a message to be sent
to the doctor via the Notification Module.
All acquired data and analyses are saved in the ap-
propriate reports, realized by the Report Module. The
system saves a report with all measurement data once
a day, which is then sent to the medical specialist at
the time scheduled by the user. Moreover, the sys-
tem can create a warning report message, attaching
the report files, if an analysis of the data using the
DSS Module reveals an abnormal situation in the pa-
tient’s state of health.
The Notification Module is the part of the software
that is responsible for notifying messages generated
by the system to the doctor and the patient. The mes-
sages can be of two types:
• Alerts, that instructs the user to perform the de-
sired measurements at scheduled time;
• E-mail messages, sent to the medical specialist in-
dicated by the user. Such messages include any
report of the patient’s measurements.
Finally, the Visualization Module is the interface
between the system and the users. It shows the real
time measurements acquired from the wearable de-
vices, the analysis data and the report files, whenever
the user chooses.

4 USE-CASE
The realized monitoring system can be used with pa-
tients suffering from cardiovascular diseases. These
patients have to constantly monitor characteristic phi-
siological data, such as blood pressure and heart rate.
Therefore, they must report these data, very often col-
lected manually over several days, to their medical
specialists during rountine follow-up visits.
The manual collection of physiological data can
increase the risk of errors, and the recording of erro-
neous values can change the evaluation of patient’s
state of health. To avoid this problem it is possible
to automate the process for capturing and monitor-
ing vital signs, as performed by the proposed system.
Moreover, this system allows the patients to monitor
their own physiological data at home using appropri-
ate wearable devices without the necessity of going to
a hospital center, providing a complete clinical picture
to the medical specialist.
The fundamental vital signs, in order to perform
a monitoring of a patient suffering from cardiovascu-
lar disease, are the heart rate, respiration rate, ECG
signal, blood pressure and oxygen saturation. There-
fore, the patient, using an appropriate wereable de-
vice, such as Zephyr Bioharness BH3, A&D Medical
UA-767PBT-C and Nonin 9560 Onyx 2 (described
in the following subsection), can capture and mon-
itor the relevant parameters, by means of a mobile
device, such as a smartphone or tablet, on which the
tele-monitoring application has been installed.
4.1 Medical Devices
The measuring accuracy of the sensor has a direct im-
pact on the accuracy of the heart parameter measure-
ment in real-time monitoring systems. Therefore, the
selection of an accurate heart parameter monitoring
device plays an important role in the early detection
of any possible heart disease.
Zephyr Bioharness BH3 is a multisensory belt
used to monitor heart rate, breathing rate and posture
in real-time. The selection of the Zephyr Bioharness
BH3 device was made on the basis of the accuracy of
the acquired physiological data, low cost and comfort
for patient comfort. This instrument is able to cap-
ture the vital signs in three different ways: with an
elastic belt in which the sensors are integrated, with a
shirt with the sensors integrated inside or with a and
holder connected with common cardiac electrodes, as
shown in the figure 3.
The second measurement parameter in our mon-
itoring system is the evaluation of blood pressure.
Blood pressure is an index of the force of the blood
Figure 3: Zephyr Bioharness BH3.
pushing against the walls of the arteries as the heart
pumps blood. It is measured as both the pressure
when the heart beats pump blood (the systolic pres-
sure) and the pressure when the heart is at rest be-
tween beats (the diastolic pressure). To monitor the
patient’s blood pressure the realized system uses the
A&D Medical UA-767PBT-C blood pressure monitor.
An acute rate of these parameters is considered as
an early indicator which supports medical specialists
in the diagnosis of serious diseases. Additionally, the
blood oxygen saturation and pulse rate can be indices
of possible alterations, monitored in our system by us-
ing the Nonin 9560 Onyx 2. The blood pressure mon-
itor and the pulse oximeter are illustred in the figure
4.
Figure 4: A&D Medical UA-767PBT-C and Nonin 9560
Onyx 2.
These three devices uses the Bluetooth protocol to
communicate with the monitoring software installed
on the Android device. The communication between
the realized system and the Nonin 9560 Onyx 2 and
the UA-767PBT-C follows the Continua Health Al-
liance guidelines. Although the Zephyr Bioharness
BH3 is not certified for this standard, a dedicated li-
brary is available enabling its connection with the mo-
bile devices.
4.2 Mobile Application
The system was implemented for mobile devices,
such as a smartphone or tablet, developed by using
the Java Programming Language through the use of

Eclipse IDE and the Android Software Developer Kit
(SDK). The mobile system offers several functionali-
ties. At the first access the user must complete a Reg-
istration form, in which he/she inserts personal infor-
mation such as name, surname, date of birth, gender,
email address. In detail, the e-mail address is both
that of the user and that of the medical specialist who
will receive the user’s report containing the measure-
ment of the physiological data and the analysis of the
estimated values. Such an e-mail will be sent at the
time indicated in the registration phase.
After the registration, the user can choose any of
the operations in the main menu shown in the screen-
shot in the figure 5.
Figure 5: Screenshots of the Homepage and History of
Measurement.
In detail, the user can perform the following func-
tionalities:
• Search Bluethooth Devices: the system searches
for Bluethooth devices and shows them to the
user. The user can choose to collect his/her pre-
ferred wearable devices able to execute different
the measurements and analyses. If the user con-
nects to the Zephyr Bioharness BH3, for example,
he/she can monitor in real-time physiological data
such as the heart and breath rate or the ECG sig-
nal, as shown in the figure 6.
Figure 6: Screenshot of the ECG monitoring.
During the signal capture, noise can add to the
useful signal distorting its interpretation and the
resulting diagnosis. To avoid this problem the user
can filter the captured signal choosing a filter of-
fered by our system, described in section 3.1. In
addition, it is possible to extract the characteristic
parameters of the Heart Variability Index (HRV).
The HRV describes the variations of both the in-
stantaneous heart rate and RR intervals, useful to
evaluate the heart state and any possible anoma-
lies due to the presence of arrhythmias (Townsend
et al., 2016);
• Specifications: information about cardiac dis-
eases and healthy lifestyles is provided, useful for
the prevention of these disorders;
• Manual Data Entry: the user can directly insert
measurement data such as blood pressure, blood
oxygen saturation, pulse rate and weight, indicat-
ing the date and time when he/she made this mea-
surement;
• Loading Report and EDF file: any report with
the recorded measurements can be saved and ex-
ported in pdf and European Data Format (EDF)
format. EDF is the most used standard to ex-
change and store biological and physical signals
(Kemp and Olivan, 2003). The user can choose
this functionality to upload these reports and files,
thanks to which the specialist can monitor the
user’s progress;
• History of Measurements: a calendar with a his-
tory of all the measurements performed is dis-
played.
4.3 Evaluation of Performance
The performance of the proposed system has been
evaluated in terms of the allocation of memory and
CPU used by the mobile application during the real-
time monitoring. The first test consisted of tracking
memory and CPU usage during a monitoring period
of 15 minutes so as to assess over time the trend of
these quantities. The real-time monitoring feature
was tested on two different devices with two differ-
ent Android versions: a Samsung GT-i9505 (S4) with
the Android 5.0.1 version and a HUAWEI GRA-L09
(P8) with the Android 6.1 version. The performance
of these analyses showed good results, as reported in
the figures 7 and 8.
The obtained results indicate that the application
is efficient in the use of system resources, which is
very important considering that it is designed to run
on a mobile device. The memory used by the applica-
tion in the real-time monitoring feature is constantly
less than 32 MB, increasing slightly applying when
the filters are applied, and the use of the CPU is low.
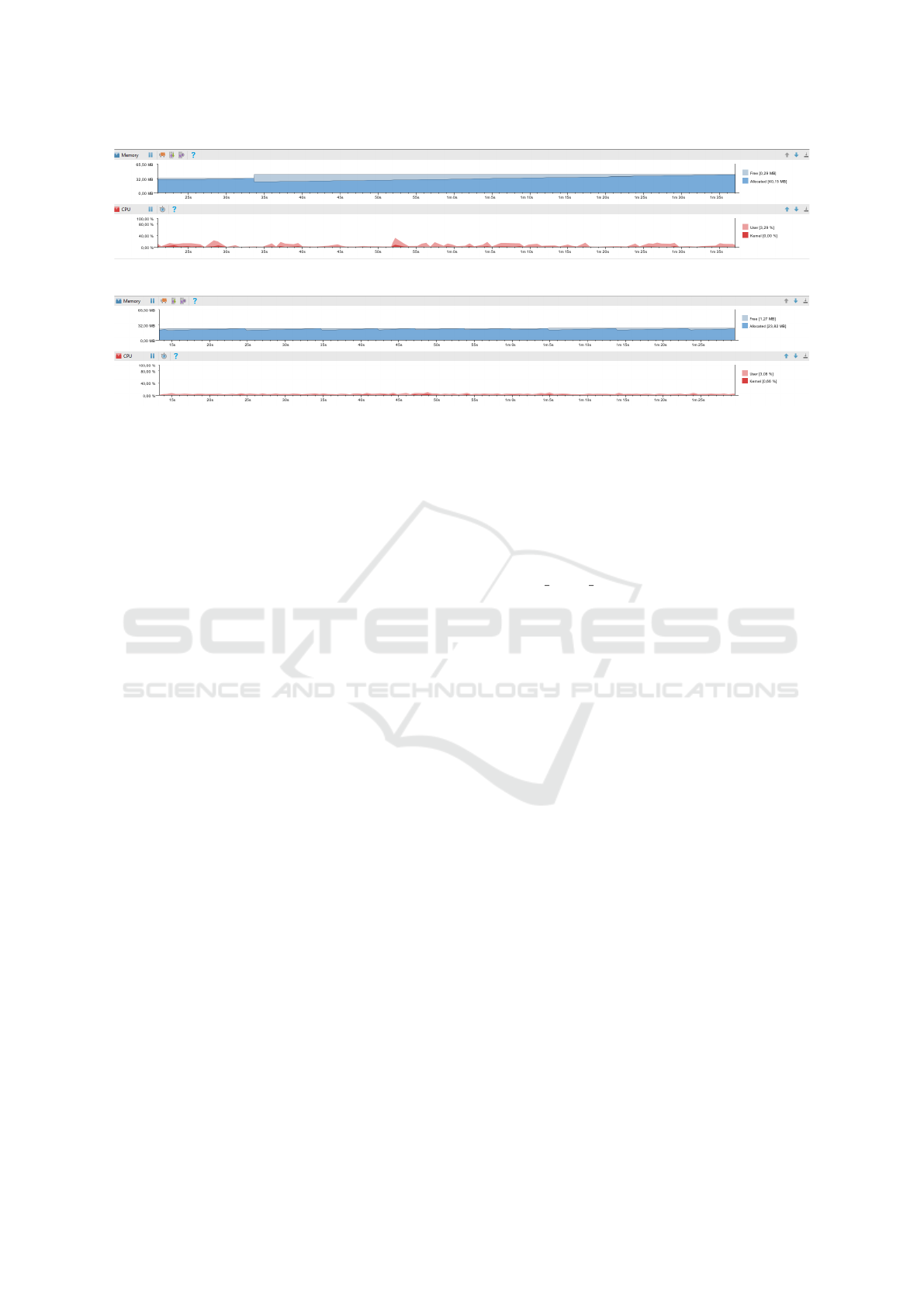
Figure 7: Performance on Samsung GT-i9505
Figure 8: Performance on HUAWEI GRA-L09
To evaluate the CPU use, we compared the per-
formance of our system with that of the SenseView
App (http://www.senseview.mobi/), which is one of
the most used apps on the market to connect with the
Zephyr Bioharness BH3. The results show that our
proposed system occupies, during the instantaneous
monitoring, about 0,4 % of CPU, while the CPU used
by the SenseView App is about 0,2 %. The RAM
used, instead, is less for our proposed app (21 MB)
than that used by the SenseView App (52 MB). This
means that the realized system can be run on mid-
range mobile devices without degrading the device
performance.
5 CONCLUSIONS
In recent years the prevalence of chronic diseases
has increased due to the rise in life expectancy and
changes in lifestyle, and thus people suffering from
these pathologies often need a continuos monitoring
of their vital signs. The mobile health field can pro-
vide new access opportunities for treatment and med-
ical services, constituting a valuable support instru-
ment for both patients and doctors.
In this paper we have presented a physiological
monitoring application designed for Android mobile
devices. The user can visualize his/her own vital
signs information, collected by means of an instru-
ment, easy and fast to use, such as a smartphone or
tablet and appropriate wearable devices. The system
does not only monitor these parameters but also ana-
lyzes them, allowing the medical specialist to make a
more accurate analysis. The system provides a good
performance in terms of memory and CPU used, in
comparison with other systems on the market.
ACKNOWLEDGEMENTS
This work has received funding from the European
Unions Horizon 2020 Framework Programme for
Research and Innovation under grant agreement no
727528 (KONFIDO) and the project ”eHealthNet”
PON03PE 00128 1. The authors would like to ac-
knowledge support from Neatec S.p.A.
REFERENCES
Al-Taee, M. A., Al-Nuaimy, W., Al-Ataby, A., Muhsin,
Z. J., and Abood, S. N. (2015). Mobile health plat-
form for diabetes management based on the internet-
of-things. In Applied Electrical Engineering and
Computing Technologies (AEECT), 2015 IEEE Jor-
dan Conference on, pages 1–5. IEEE.
Anliker, U., Ward, J. A., Lukowicz, P., Troster, G., Dolveck,
F., Baer, M., Keita, F., Schenker, E. B., Catarsi,
F., Coluccini, L., et al. (2004). Amon: a wear-
able multiparameter medical monitoring and alert sys-
tem. IEEE Transactions on information technology in
Biomedicine, 8(4):415–427.
Banos, O., Villalonga, C., Damas, M., Gloesekoetter, P., Po-
mares, H., and Rojas, I. (2014). Physiodroid: Combin-
ing wearable health sensors and mobile devices for a
ubiquitous, continuous, and personal monitoring. The
Scientific World Journal, 2014.
Bender, D. and Sartipi, K. (2013). Hl7 fhir: An agile and
restful approach to healthcare information exchange.
In Proceedings of the 26th IEEE International Sym-
posium on Computer-Based Medical Systems, pages
326–331. IEEE.
Bisio, I., Lavagetto, F., Marchese, M., and Sciarrone, A.
(2015). A smartphone-centric platform for remote
health monitoring of heart failure. International Jour-
nal of Communication Systems, 28(11):1753–1771.
Carroll, R., Cnossen, R., Schnell, M., and Simons, D.
(2007). Continua: An interoperable personal health-

care ecosystem. IEEE Pervasive Computing, 6(4):90–
94.
Centro nazionale di epidemiologia, sorveg-
lianza e promozione della salute dell’Istituto
superiore di sanit
`
a (2016). Il portale
dell’epidemiologia per la sanit
`
a pubblica.
http://www.epicentro.iss.it/focus/cardiovascolare/
cardiovascolari.asp/.
Chan, M., Est
`
eve, D., Fourniols, J.-Y., Escriba, C., and
Campo, E. (2012). Smart wearable systems: Current
status and future challenges. Artificial intelligence in
medicine, 56(3):137–156.
Chen, H. and Chen, S. (2003). A moving average based
filtering system with its application to real-time qrs
detection. In Computers in Cardiology, 2003, pages
585–588. IEEE.
Cuomo, S., De Pietro, G., Farina, R., Galletti, A., and San-
nino, G. (2016). A revised scheme for real time ecg
signal denoising based on recursive filtering. Biomed-
ical Signal Processing and Control, 27:134–144.
Forastiere, M., De Pietro, G., and Sannino, G. (2016). An
mhealth application for a personalized monitoring of
ones own wellness: Design and development. In Inno-
vation in Medicine and Healthcare 2016, pages 269–
278. Springer.
Gay, V. and Leijdekkers, P. (2007). A health monitoring
system using smart phones and wearable sensors. In-
ternational journal of ARM, 8(2):29–35.
Guo, X., Duan, X., Gao, H., Huang, A., and Jiao, B. (2013).
An ecg monitoring and alarming system based on an-
droid smart phone. Communications and Network,
5(03):584.
Kakria, P., Tripathi, N., and Kitipawang, P. (2015). A real-
time health monitoring system for remote cardiac pa-
tients using smartphone and wearable sensors. In-
ternational journal of telemedicine and applications,
2015.
Kemp, B. and Olivan, J. (2003). European data format
plus(edf+), an edf alike standard format for the ex-
change of physiological data. Clinical Neurophysiol-
ogy, 114(9):1755–1761.
Konstantas, D. (2007). An overview of wearable and im-
plantable medical sensors. Yearbook of medical infor-
matics, 7(1):66–69.
Lee, J. M., Hirschfeld, E., and Wedding, J. (2016).
A patient-designed do-it-yourself mobile technology
system for diabetes: Promise and challenges for a new
era in medicine. JAMA, 315(14):1447–1448.
Lmberis, A. and Dittmar, A. (2007). Advanced wearable
health systems and applications-research and develop-
ment efforts in the european union. IEEE Engineering
in Medicine and Biology Magazine, 26(3):29–33.
Lv, Z., Xia, F., Wu, G., Yao, L., and Chen, Z. (2010). icare:
a mobile health monitoring system for the elderly. In
Proceedings of the 2010 IEEE/ACM Int’l Conference
on Green Computing and Communications & Int’l
Conference on Cyber, Physical and Social Computing,
pages 699–705. IEEE Computer Society.
Park, H. S., Cho, H., and Kim, H. S. (2016). Development
of a multi-agent m-health application based on various
protocols for chronic disease self-management. Jour-
nal of medical systems, 40(1):1–14.
Rodrigues, D. F., Horta, E. T., Silva, B. M., Guedes,
F. D., and Rodrigues, J. J. (2014). A mobile health-
care solution for ambient assisted living environments.
In e-Health Networking, Applications and Services
(Healthcom), 2014 IEEE 16th International Confer-
ence on, pages 170–175. IEEE.
Rubel, P., Fayn, J., Nollo, G., Assanelli, D., Li, B., Restier,
L., Adami, S., Arod, S., Atoui, H., Ohlsson, M., et al.
(2005). Toward personal ehealth in cardiology. results
from the epi-medics telemedicine project. Journal of
electrocardiology, 38(4):100–106.
Sanchis-Gomar, F., Perez-Quilis, C., Leischik, R., and Lu-
cia, A. (2016). Epidemiology of coronary heart dis-
ease and acute coronary syndrome. Annals of Trans-
lational Medicine, 4(13).
Szydło, T. and Konieczny, M. (2016). Mobile and wearable
devices in an open and universal system for remote pa-
tient monitoring. Microprocessors and Microsystems,
46:44–54.
Tang, P. C., Ash, J. S., Bates, D. W., Overhage, J. M., and
Sands, D. Z. (2006). Personal health records: defini-
tions, benefits, and strategies for overcoming barriers
to adoption. Journal of the American Medical Infor-
matics Association, 13(2):121–126.
Townsend, N., Wilson, L., Bhatnagar, P., Wickramasinghe,
K., Rayner, M., and Nichols, M. (2016). Cardiovas-
cular disease in europe: epidemiological update 2016.
European heart journal, page ehw334.
Verde, L., De Pietro, G., Veltri, P., and Sannino, G.
(2015). A noise-aware methodology for a mobile
voice screening application. In Advances in Sensors
and Interfaces (IWASI), 2015 6th IEEE International
Workshop on, pages 193–198. IEEE.
Wolf, K.-H., Schirmer, S., Marschollek, M., and Haux, R.
(2009). Representing sensor data using the hl7 cda
personal healthcare monitoring report draft. In MIE,
pages 480–484. Citeseer.
World Health Organization (2016). Chronic diseases and
health promotion. http://www.who.int/chp/en/.
