
Home Monitoring in Portugal
An Overview on Current Experiences
Ana Dias
1
, Madalena Vilas Boas
1
, Daniel Polónia
1
, Alexandra Queirós
2
and Nelson Pacheco Rocha
3
1
Department of Economics, Management, Industrial Engineering and Tourism, University of Aveiro,
Campo Universitário de Santiago, 3810-193 Aveiro, Portugal
2
Health Sciences School, University of Aveiro, Campo Universitário de Santiago, 3810-193 Aveiro, Portugal
3
Department of Medical Sciences, University of Aveiro, Campo Universitário de Santiago, 3810-193 Aveiro, Portugal
Keywords: Telemedicine, Teleconsultation, Home Monitoring, Portuguese National Health Service.
Abstract: This paper aims to be a contribution to the discussion on the issue of innovation in healthcare since, in the
author’s perspective, the health sector, and particularly the Portuguese National Health Service, needs
changes in its "business model". There is a need of redirecting care provision to the citizen’s natural
environment, namely considering the opportunities offered by information and communication
technologies. For this purpose the authors surveyed projects already implemented in Portugal, within the
Portuguese National Health Service, related to home monitoring, in order to make a critical analysis of the
state of the art of ongoing projects. In this study, the authors identified four pilot experiences of home
monitoring, all targeted at chronic disease. In spite of some results of these experiments are already known,
there is a shortage of available information and scientific evidence, both about the implementation processes
themselves and about their clinical, technical and economic evaluation, which, in the opinion of the authors,
also hinders their assessment and dissemination.
1 INTRODUCTION
The Portuguese National Health Service (Serviço
Nacional de Saúde - SNS) presents difficulties in the
coordination between levels of care, particularly
among primary healthcare and hospital care, which
has an impact on patient access to healthcare (Barros
and Simões, 2007).
Traditionally, acute diseases were the main
concern of health systems, a situation that has
changed over the last century, as a result of advances
in biomedicine and public health, with a significant
impact on the eradication of certain infectious
diseases. What is questioned today is whether, with
regard to the organizational model of health systems,
they fit the current reality where chronic diseases are
predominant (Dias, 2015).
Data from the National Health Survey (INS,
2014) are indicative of the new challenges of the
Portuguese SNS. In 2014, more than half (52.8%) of
the population aged 18 years, was overweight
(50.9% a decade ago). The symptoms of depression
also worsened, affecting more the retired population
(36.5% of the retired population had symptoms of
depression, compared to 18,5% of the employed
population). Also the percentage of people who
reported consuming prescribed drugs increase
sharply with age: more than 90% of the population
over 65 years. Comparing the results for chronic
diseases collected in two surveys (2005-2006 and
2014) it is clearly an increase of the percentage of
population affected by these diseases (INS, 2014).
The aging process that the Portuguese population
is suffering further enhances this scenario. The
National Statistics Institute (Instituto Nacional de
Estatística - INE) forecasts that the potential
sustainability index (i.e. the ratio between the
number of people aged between 15 and 64 and the
number of people aged 65 and over) may decrease
abruptly: in Portugal, between 2012 and 2060, this
index, in one of the most likely scenarios can change
from 340 people in working-age for every 100
elderly to 149 people in working-age for every 100
elderly, a value that can decrease to 111 people in
working-age for every 100 elderly in the worse-case
scenario (INE, 2014a).
We are at a very particular moment of our
history in which a "demographic transition” is
Dias A., Vilas Boas M., Poløsnia D., Queirøss A. and Pacheco da Rocha N.
Home Monitoring in Portugal - An Overview on Current Experiences.
DOI: 10.5220/0006220603770382
In Proceedings of the 10th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2017), pages 377-382
ISBN: 978-989-758-213-4
Copyright
c
2017 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
377
combined with “an epidemiological transition" and
"this combination of phenomena is confronting us
with a crisis (…) which comes as an opportunity to
look critically at what has been done and, based on
that, project us in the future with more appropriate
tools and skills to new circumstances." (OPSS, 2016,
p. 31).
This study thus seeks to contribute to the
discussion on the theme of innovation in healthcare
in Portugal, taking advantage of the opportunities
offered by information and communication
technologies. In particular, given the home
monitoring potential, which is supported on the
progress achieved in mobile technologies, as well as
its relevance to chronic diseases, this study aims to
analyze the viability of experiences already
implemented in Portugal related to home monitoring
of patients with chronic diseases.
2 RELATED WORK
In Portugal, via the 3571/2013 Order, published in
the Official Gazette on March the 6
th
, 2013, the
Ministry of Health, assuming that the use of
telemedicine allows the observation, diagnosis,
treatment and monitoring in a more convenient place
for patients, particularly at home, states that "the
services and facilities of the National Health Service
(SNS) should increase the use of information and
communication technologies in order to promote and
ensure the provision of telemedicine services to [its]
users" (p.8326).
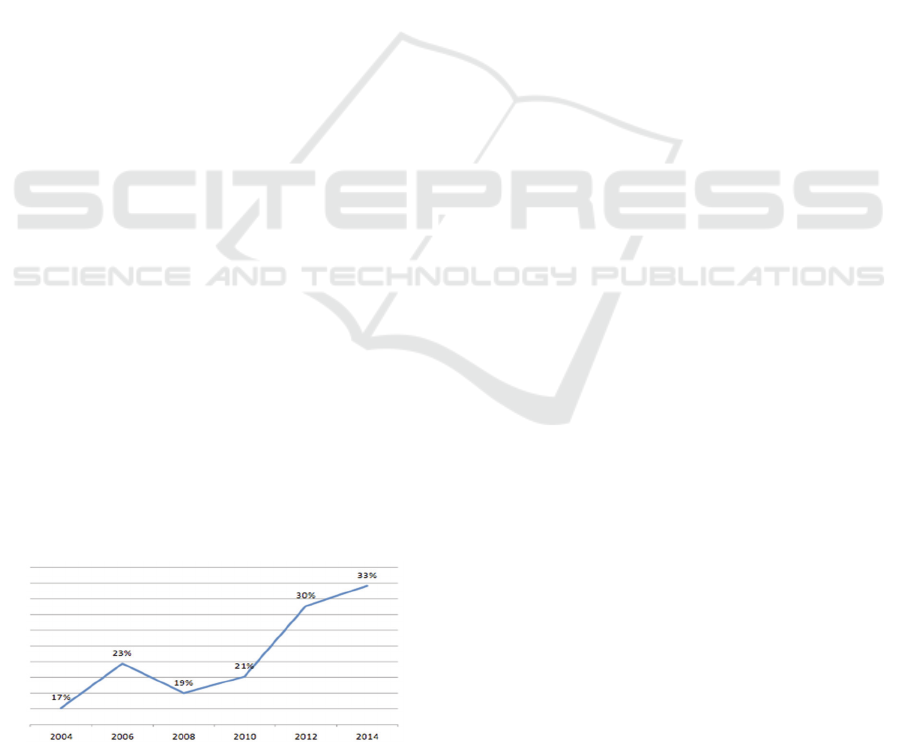
According to INE, on its Survey on the Use of
Information and Communication Technologies in
Hospitals (INE, 2014b), one third of the Portuguese
hospitals developed telemedicine activities in 2014,
an increase of 16 percentage points in ten years (12
percentage points in the last four years) (Figure 1).
However, the degree of implementation of
telemedicine is quite different in public hospitals
(51%) and private hospitals (15%).
Figure 1: Proportion of hospitals with telemedicine,
Portugal, 2004-2014 (Source: INE, 2014b).
Telemedicine activity can take many forms,
ranging from remote diagnosis (teleradiology and
telepathology) to remote care provision, such as
teleconsultation or home monitoring. Within
telemedicine activities, the most used was
teleradiology (i.e. the exchange of images to discuss
cases and for diagnosis), being reported by 84% of
hospitals that refer having telemedicine. On the
other hand, only 31% of hospitals that report having
telemedicine provide teleconsultation (i.e. 10% of
the total hospital’s number) (INE, 2014b).
As a result of the telemedicine development,
Portugal is involved in several international projects
to promote the cooperation between healthcare
professionals. In particular, there are some projects
with the African Countries with Portuguese as an
Official Language (Países Africanos de Língua
Oficial Portuguesa - PALOP) (Borja-Santos, 2013).
In October 2013 it was launched a telemedicine
platform between Portugal and several PALOP
(Noronha, 2013) but, previously, there were other
projects. For example, in 2012 a project between
Portugal and São Tomé and Príncipe allowed an
estimated saving of 180,000 euros in the transfer of
patients to Portugal and allowed to save one million
euros to the Portuguese Ministry of Health
(Noronha, 2013). Portugal is also part of a
telemedicine network with Angola and the
University Hospitals of Geneva that allows technical
support for diagnosis and treatment of Angolan
patients.
In addition to the experiences within the PALOP,
there are others being carried out between Portugal
and Spain. Since 2003 the southern region of the
Algarve has participated in a telemedicine project in
conjunction with the Spanish region of Andalusia,
with the aim of creating new communication
channels between the Algarve and Andalusia and,
inside the Algarve, between the health centers and
the hospitals in the region, with the installation of
telemedicine equipment in all health centers (Portal
da Saúde, 2005).
With regard to teleconsultation, in 2007, it was
launched in Portugal the “Linha de Saúde 24”,
which provides counselling and referral in a disease
situation, accessible through the phone (or chat for
people with special needs) as well as therapeutic
counselling to clarify particular questions and
provide support related to matters as medication
(Saúde 24, s.d.).
Within a group of other innovative projects in
this area, out of the governmental sphere, the authors
highlight two: the "Patient Innovation", a social
network for patients who, sharing experiences about
HEALTHINF 2017 - 10th International Conference on Health Informatics
378

their illness, can develop solutions to their real
problems, from therapeutic support to proper
medical equipment (Pinho, 2013) and a private
service that allows traveler teleconsultations
(Consulta do Viajante, 2016).
Specifically, in the region of Alentejo (one of the
most aged and sparsely populated regions of the
country) several teleconsultation experiments
(Oliveira et al., 2014) were reported, dating back to
1998, in order to respond to challenges such as
desertification, isolation, low population density,
poverty, lack of medical resources in several
specialties as well as poor public transports, all of
which have acted as barriers to access to healthcare
in the region. It should be noted that the Alentejo
region represents approximately one-third of
Portugal’s continental territory, but it is home to
only 5% of its population. Teleconsultations are
available in 15 medical specialties, ranging from
Neurology to Pediatric Surgery. The network
includes 20 primary care units and five hospitals,
covering almost 30,000 km
2
and around 500,000
people. A comprehensive assessment of the costs
and consequences of the program is currently
underway, since it is stated that there is a lack of
evidence of its cost-effectiveness, which, according
to Oliveira et al. (2014), hinders the sustainment and
realization of the promise of innovative solutions,
wherever it is implemented.
Regarding the autonomous islands, the Azores
already belongs to several networks, which allows
the realization of teleconsultation to determine the
clinical need of the patient's displacement to
mainland to carry out consultations and exams
(Mourato, 2014). In the Azores the use of
teleconsultation in Nursing is also frequent,
particularly in decision support in the treatment of
wounds. Furthermore, there is already
teleconsultation in various health centers in the
archipelago in the following specialties:
Nephrology, Pediatric Cardiology, Neonatology and
Endocrinology.
Home monitoring can improve disease
prevention, facilitate chronic disease management,
including disease self-management, enable
personalization of care, and improve productivity in
healthcare, thus allowing a more rational use of
health services (Queirós et al., 2013; Queirós et al.,
2017). In Portugal, according to the Order
8445/2014 of June the 30th, 2014, the Ministry of
Health stressed the need to improve the capacity of
health monitoring, prevention, detection and
treatment of disease in innovative ways, including
through models of care in order to maintain people
in their homes, promoting their autonomy and
encouraging personal responsibility by adopting
healthy lifestyles. However, there are no studies
reporting the current experiences of home
monitoring in Portugal.
3 METHODS
Considering the lack of evidence of current
Portuguese home monitoring experiences, the
present study has the following main objectives:
To make an inventory of projects already
implemented in Portugal, within the SNS in
the area of home monitoring, particularly
focused on the chronically ill, and preferably
projects involving primary healthcare, which
is believed that will assume an increasingly
central role in the management of chronic
disease.
To make a critical analysis of the state of the
art of ongoing projects.
The authors consulted the Central Administration
of the Health System (Administração Central do
Sistema de Saúde - ACSS) in order to retrieve
information on projects related to home monitoring
already implemented by the SNS.
Subsequently, an additional survey was
conducted to analyze if there were publications that
best described these experiences and others in the
same area, and possible results already obtained.
Finally, the authors conducted a survey on the
web pages of SNS hospitals to search for innovative
projects in general, and home monitoring in
particular. For this purpose, the web pages of 41
hospitals were identified and analyzed.
4 HOME MONITORING
EXPERIENCES IN PORTUGAL
With data provided by the ACSS it was possible to
identify three projects related to home monitoring
already implemented by the Portuguese SNS. In the
area of Pulmonology, a home monitoring pilot
program of chronic obstructive pulmonary disease
was developed, funded by the ACSS and supported
by Shared Services of the Health Ministry (Serviços
Partilhados do Ministério da Saúde - SPMS), the
government agency for eHealth, in partnership with
five hospitals, covering a total of 75 patients with
severe disease (15 per hospital). These patients were
selected in each hospital by their attending
Home Monitoring in Portugal - An Overview on Current Experiences
379

physician, based on their prior history of chronic
obstructive pulmonary disease. This home
monitoring pilot program began in 2013 and was
implemented in a phased manner in the five
institutions, namely: Hospital of Faro (Algarve) -
beginning in August 2013 (Phase 1); Hospital Pêro
da Covilhã (Cova da Beira) - beginning in March
2014; Hospital and University Center of Coimbra -
beginning in May 2014; Hospital of Viana do
Castelo (Alto Minho) - beginning in October 2014
and Hospital of Portalegre/Elvas (North Alentejo) -
beginning in October 2014. Five private companies
were also involved in the project and were
responsible for the installation of the monitoring
devices and their maintenance and for the process of
gathering information and transfer it to health
professionals. Each patient was assigned the
following monitoring devices: blood pressure
measuring device, pulse oximeter, thermometer,
odometer, device monitoring heart rate and mobile
phone. The clinical teams of the hospitals were
actively involved in the monitoring of patients
integrated in the program and also in their education.
According to SPMS (2014), under this pilot
program, patients are monitored in their homes. The
respective data are then analyzed twice a day by the
Pulmonology teams of involved hospitals, trying to
reduce the aggravation of their clinical situation,
thus avoiding new hospital admissions.
The objectives and results to be achieved in 2016
within the home monitoring program for chronic
obstructive pulmonary disease include (ACSS,
2016): raising the quality of services provided to
citizens, promoting the continuous monitoring of
their health condition; reducing at least one episode
of annual hospitalizations as a result of the
deterioration of the patients medical condition;
reducing at least three episodes of urgency per year;
reducing at least two episodes of outpatient
consultation per year, and follow, proactively and
continuously, the fluctuations of the health
conditions of each patient.
In terms of preliminary results of this pilot
program, according to Pereira (2016), these have
been encouraging, both in terms of satisfaction and
health indicators, having already been released some
results of an evaluation carried out in the Local Unit
of the Alto Minho, namely the reduction in 50% of
visits of these patients to emergency services, as
well as a decrease in the number of hospitalizations
(70%). Pereira (2016) also states that in these five
hospitals, 61% of patients considered the quality of
the service as "very good or excellent”. Although the
final overall results are not yet available due to the
late start in one of the hospitals, interim evaluations
reveal both a reduction in the number of hospital
admissions or visits to the urgency services of
patients, more evident in some hospitals.
More recently, in November 2015, the “Home
Monitoring Plan” was adopted for the definition of
sites for the realization of home monitoring and its
articulation with the rules of the SNS.
In this context, and for the year 2016, it was
contracted activity for the implementation of other
two home monitoring pilot programs: a Pilot
Program for Home Monitoring of Acute Myocardial
Infarction and a Pilot Program for Chronic Heart
Failure. Like the pilot program of chronic
obstructive pulmonary disease, it was planned that
the program would be implemented in five hospitals
covering a group of 75 patients (15 per hospital).
In the case of the chronic heart failure, and in the
absence of results which can be explained due to the
program's newness, it should be noted that from
conventional remote monitoring to more recent
strategies, using cardiac devices or implantable
hemodynamic monitors, this is a topic under active
investigation, but, despite previous meta-analyses of
small studies have documented the potential benefit
of home monitoring, major randomized clinical trials
have failed to demonstrate the positive impact of this
strategy. In addition, data on the value of the latest
monitoring devices are contradictory, since some
studies have documented potential prognosis benefit
while others cannot confirm it (Sousa et al., 2014).
As a result of the literature review carried out in
scientific databases, the authors found a concrete
example in Portugal of assessment of a home
monitoring experience in cardiac patients, with four
hospitals involved. This study, of 2013, indicates
that the introduction of home monitoring has the
ability to reduce in 25% the costs of monitoring the
patients (Costa et al., 2013).
To broaden the scope of this research, and to
identify innovative projects, in general, and home
monitoring, in particular, the authors decided to
search for information on the web pages of the SNS
hospitals. From the 41 organizations identified six
refer teleconsultation activities on the following
areas: Dermatology (referred by three
organizations), Pediatric Cardiology (two
organizations), Internal Medicine, Endocrinology,
Rheumatology, Oncology, Neurosurgery, Pediatrics,
Gynecology, Ophthalmology, Genetics, Imaging and
Pathology (all referred only by one organization).
However, no organization mentions any home
monitoring experiment.
HEALTHINF 2017 - 10th International Conference on Health Informatics
380

5 DISCUSSION
The main purpose of this study was to give visibility
to the experiences already implemented in Portugal
related to home monitoring of patients with chronic
conditions, which the authors believe could permit
not to repeat known errors as well as to replicate
successes, after being properly evaluated and
contextualized. However, it is clear that, although
some results of these experiments have been
reported in this paper, there is a shortage of
scientific evidence regarding, on one hand, the
implementation process and, on the other hand, the
evaluation of these experiences, what is conflicting
to what is defended in the eHealth Action Plan 2012-
2020 - Innovative healthcare for the 21st century
(Commission of the European Union, 2012),
namely: “It is essential to measure and assess the
added value of innovative eHealth products and
services to achieve wider evidence-based eHealth
deployment and create a competitive environment
for eHealth solutions.” (p.13)
Regarding the home monitoring pilot projects
identified in this work the authors would like to
stress that the pathologies covered by the pilot
projects correspond to chronic diseases and that they
are also within the group of priority areas identified
by the Portuguese government in 2013.
Concerning these same projects the authors also
want to highlight the fact that in the group of
institutions covered by these projects, there are no
institutions coming from primary healthcare, at least
not in an explicit and formal way. As mentioned
before, the authors consider that the primary
healthcare services must increasingly be involved
because of their close proximity to the patient and
their informal careers as well as due to their abilities
in the management of chronic disease, even because
one of the main purposes of home monitoring is to
reduce the number of admissions or visits to the
hospital emergency services. It is important to
emphasize the significance of primary healthcare in
the organization of health systems, recalling what in
1978 was stated in the Declaration of Alma Ata
(WHO, 1978) on the importance to be given to this
level of care: “Primary healthcare is essential
healthcare based on practical, scientifically sound
and socially acceptable methods and technology
made universally accessible to individuals and
families in the community through their full
participation and at a cost that the community and
country can afford (…) It is the first level of contact
of individuals, the family and community with the
national health system bringing healthcare as close
as possible to where people live and work, and
constitutes the first element of a continuing
healthcare process.” (p.1-2)
Concerning the results obtained from the
research on the hospital’s web pages, the authors
would like to highlight the scarce information
available with regard to innovative experiences, as
well as the complete lack of publicizing information
about home monitoring. This, from the author’s
point of view, can raise questions in particular
regarding the opportunities created for patients to
participate in these experiences and create obstacles
to ensure the equity required in healthcare provision.
Despite the fact that, as it has also been
demonstrated in this work, home monitoring
experiences in Portugal are still small, in number
and in size, still the authors would like to discuss the
importance of what is (or not) revealed to the public:
whether information regarding the experiences as a
whole whether information on the criteria for
inclusion of patients in these experiments. Another
purpose of this advertising is, from the author’s
point of view, to emphasize the need to make the
whole process more transparent, with particular
interest to patients and also to other health
professionals and institutions, a similar progress that
what has been achieved with respect to clinical trials
since 2011. Since then, the information on clinical
trials with medicines for human use, which are
underway in the European Union, is accessible to all
European citizens from the portal "EU clinical trials
Register" and, more recently, through the
international network of clinical trials registers of
the World Health Organization. In Portugal, Law
21/2014 of the 16th April, amended by Law 73/2015
of the 27th July, envisages the creation of the
National register of clinical trials. Still, and going
back to experiences that are developed within the
SNS in Portugal, and highlighting once again the
difficulties, specifically in this study, on the
collection of information on ongoing initiatives, the
authors would like to discuss the pertinence of
creating a platform for registering, monitoring and
disseminating results of these experiences, similar to
what is already being done in the clinical trials
domain.
6 CONCLUSION
In Portugal, within the SNS, the authors identified
four pilot experiences of home monitoring, all
targeted at chronic disease, but with no direct
involvement of primary healthcare, at least explicit
Home Monitoring in Portugal - An Overview on Current Experiences
381

in contracts that were made between the ACSS and
the primary healthcare services. This somehow
contradicts the need to direct primary care for the
prevention, with a view to achieve further gains in
health outcomes as well as improvements in terms of
efficiency.
The authors would also like to point out the
difficulty in getting information related to home
monitoring experiences taking place in the SNS,
from one source, which, from our point of view,
should be either the ACSS or the SPMS. In the
author’s point of view, if this information is not
someway centralized, the evaluation and subsequent
dissemination of these experiences will be more
difficult to achieve.
It should also be noted that it was not possible to
identify evaluation methods with the purpose of,
systematically, evaluating experiences, so that the
decisions can be based on accurate information, it
can be possible to learn from mistakes as well as to
innovate by sharing and replicating successful
experiences, although this is one of the EU
guidelines for the eHealth Action Plan 2012-2020
(Commission of the European Union, 2012).
REFERENCES
ACSS (2016). Termos de referência para contratualização
hospitalar no SNS – Contrato Programa 2016.
Barros, P. P. and Simões, J. D. A. (2007). Health systems
in transition: Portugal – Health system review. The
European Observatory on Health Systems and
Policies.
Borja-Santos, R. (2013). Ministério quer que serviços de
saúde apostem mais na telemedicina. Jornal Público.
Available in:
https://www.publico.pt/sociedade/noticia/ministerio-
quer-que-servicos-de-saude-apostem-mais-na-
telemedicina-1586809.
Commission of the European Union (2012). eHealth
Action Plan 2012-2020 - Innovative healthcare for the
21st century.
Consulta do Viajante (2016). Available in:
http://www.consultadoviajante.com/sobre.html.
Costa, P. D., Reis, A. H. and Rodrigues, P. P. (2013).
Clinical and economic impact of remote monitoring on
the follow-up of patients with implantable electronic
cardiovascular devices: An observational study.
Telemedicine and e-health, 19(2), pp. 71–80.
Dias, A. (2015). Integração de cuidados de saúde
primários e hospitalares em Portugal: uma avaliação
comparativa do modelo de unidade local de saúde
(Tese de Doutoramento). Universidade de Aveiro,
Portugal.
INE (2014a). Projeções de População Residente 2012-
2060. Lisboa: Instituto Nacional de Estatística.
INE (2014b). Inquérito à utilização das tecnologias de
informação e da comunicação nos hospitais 2014.
Lisboa: Instituto Nacional de Estatística.
INS (2014). Inquérito nacional de saúde 2014. Available
in:
http://www.insa.pt/sites/INSA/Portugues/ComInf/Noti
cias/Documents/2015/Novembro/11INS2014.pdf.
Mourato, P. (2014). Telemedicina generaliza-se até final
do ano. Available in:
http://www.dn.pt/portugal/acores/interior/telemedicina
-generalizase-ate-final-do-ano-3960209.html.
Noronha, N. (2013). Rede de telemedicina entre Portugal e
PALOP avança em 2014. Available in:
http://lifestyle.sapo.pt/saude/noticias-
saude/artigos/rede-de-telemedicina-entre-portugal-e-
palop-avanca-em-2014.
Oliveira, T.C., Bayer, S., Gonçalves, L., and Barlow, J.
(2014). Brief Communication-Telemedicine in
Alentejo. Telemedicine and e-Health. 20 (1)
OPSS (2016). Relatório de Primavera 2016 - Saúde:
Procuram-se novos caminhos. Observatório Português
dos Sistemas de Saúde. Available in:
http://www.opss.pt/node/488.
Pereira, J. (2016). Telemedicina em Portugal.
NewsPharma MyPneumologia. Available in:
http://www.mypneumologia.pt/entrevistas/208-
telemedicina-em-portugal.html
Pinho, L. (2013). Patient Innovation é uma rede social
para doentes. Jornal Público. Available in:
http://p3.publico.pt/actualidade/ciencia/8400/patient-
innovation-e-uma-rede-social-para-doentes.
Portal da Saúde (2005). Portugal e Espanha implementam
a Telemedicina no Algarve. Available in:
http://www2.portaldasaude.pt/portal/conteudos/a+saud
e+em+portugal/investigacao+e+desenvolvimento/tele
medicina.htm.
Queirós, A., Carvalho, S., Pavão, J., Da Rocha, N.P.
(2013). AAL information based services and care
integration. In HEALTHINF 2013 - Proceedings of the
International Conference on Health Informatics, pp.
403-406. ISBN: 978-989856537-2.
Queirós, A., Pereira, L., Dias, A. and Rocha, N. (2017).
Technologies for Ageing in Place to Support Home
Monitoring of Patients with Chronic Diseases. In
HEALTHINF 2017 - Proceedings of the International
Conference on Health Informatics
.
Saúde 24 (s.d.). Quem somos. Available in:
http://www.saude24.pt/PresentationLayer/ctexto_00.as
px?local=15.
Sousa, C., Leite, S., Lagido, R., Ferreira, L., Silva-
Cardoso, J., and Maciel, M.J. (2014). Telemonitoring
in heart failure: A state-of-the-art review. Revista
portuguesa de cardiologia, 33(4), pp.229-239.
SPMS (2014). Telemonitorização DPOC. Available in:
http://spms.min-saude.pt/2014/04/telemonitorizacao-
dpoc-2/.
WHO (1978). Declaration of Alma-Ata. International
Conference on Primary Health Care, Alma-Ata,
USSR, 6-12 September 1978.
HEALTHINF 2017 - 10th International Conference on Health Informatics
382
