
Identifying Key Components of Services in Healthcare
in the Context of out-Patient in Norway
Eunji Lee
SINTEF, Oslo, Norway
Keywords: Service Design, Healthcare, eHealth.
Abstract: This paper discusses components of service in healthcare. Four components of a service (service customer,
service worker, service setting and service process) were introduced. Yet these components have not been
explored in healthcare cases. We identified the key components through our case study with out-patient
histories, involving electronic health record systems. Based on our analysis we propose a set of components
to be considered for designing stakeholder-centred services in healthcare. The result of this study might be
useful to the health informatics researchers to better understand the service interactions in today’s healthcare
in a more analytic and holistic way by taking the service engineering perspective, at the same time to the
service engineering or design researchers to have a deeper insight of the services in healthcare and the
components to be considered when designing the services.
1 INTRODUCTION
The service delivery process in healthcare is
complex (Reichert, 2011); designing healthcare
services can therefore be challenging. Healthcare
services involve many actors, who work with
different agendas, have highly specific knowledge,
and who have tasks that are intertwined with other
organisations. eHealth, a healthcare service that is
supported by telecommunications and information
technology (Mitchell, 2000), complicates the service
delivery process even further. While eHealth
technologies break down barriers of time and place,
thus bringing people and resources together to
provide healthcare services in more efficient ways
(Hesse and Shneiderman, 2007), it also generates
various interactions between many actors and
systems which were absent in conventional health
service situations.
Involving eHealth technologies in today’s
healthcare service is not uncommon. For instance,
while a patient has a consultation with his/her
general practitioner (GP), the GP looks up the
information from the previous consultation(s)
through an electronic health record (EHR) system.
The use of such technology changes the healthcare
practices and consequently can affect patient’s life
(Rodolfo et al., 2014). Therefore, there is a need to
understand the complex service delivery process in
healthcare in an analytic and holistic approach. Such
approach might contribute to better assess the
existing services in healthcare, which can be a
starting point for designing improved services.
Gadrey (2002) introduced three components of a
service: service provider, customer/client/user, and
transformation of a reality. Fisk et al. (2013)
presented and defined four components of service
and the definitions are as below.
• Service customer: the recipient of the service
• Service worker: the contributor of the service
delivery by interacting with service customer
• Service setting: the environment in which the
service is delivered to the customer
• Service process: the sequence of activities
essential to deliver the service
Yet these components have not been fully
explored in today’s complex healthcare settings. Our
research question is “What are the key components
in out-patient services?”
The rest of this paper is organised as follows: We
first describe our research approach, context,
methodology, and methods for data collection and
analysis in Section 2. In Section 3, we introduce two
out-patient histories. We then present the results
from our analysis in Section 4 and discuss the results
in Section 5. In Section 6, we discuss the limitations
of this study. Finally, we conclude our study and
suggest future research in Section 7.
354
Lee E.
Identifying Key Components of Services in Healthcare in the Context of out-Patient in Norway.
DOI: 10.5220/0006170803540361
In Proceedings of the 10th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2017), pages 354-361
ISBN: 978-989-758-213-4
Copyright
c
2017 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

2 RESEARCH APPROACH
We applied a qualitative methodology to investigate
our research question. We conducted a multiple case
study using two out-patient histories in Norway from
September-October 2013. Case study is defined as
“scholarly inquiry that investigates a contemporary
phenomenon within its real-life context (Yin,
1994).” Multiple case study is instrumental study
which allows researchers to understand and analyse
several cases across settings thus leading better
theorising (Stake, 2005; Baxter and Jack, 2008).
Data was collected through conducting
document analysis, observations and interviews at a
surgical out-patient clinic in a hospital in Norway.
Due to ethical consideration, a chief nurse explained
two patients’ histories by showing the electronic
documents in an EHR system and other relevant
paper documents; no direct access to the EHR
system was given to the researcher. Semi-structured
interviews with the chief nurse followed after the
nurse’s explanations. To obtain deeper insight in the
histories, we conducted observations and
unstructured interviews of a secretary working at the
hospital’s post/document centre, a medical doctor
(specialist) and a health secretary working at the
clinic. During the observations, the researcher took
notes and some photos of the documents were taken.
All interviews were audio-recorded. Email
exchanges and telephone conversations
supplemented the data after the interviews.
Document analysis is a systematic method for
reviewing or evaluating documents, which is
unobtrusive and nonreactive when obtaining
empirical data (Bowen, 2009). Observation is a
useful data gathering method in naturally occurring
settings and it helps the researchers to understand
the users’ context, tasks, and goals (Rogers et al.,
2011). Unstructured and semi structured interviews
can be most suitable when the researchers want to
have a deeper insight of a problem domain that is
not familiar by giving the participants the chance to
educate the researchers. (Lazar et al., 2010).
Interviews and/or observation are often used to
establish credibility and minimise bias of the data
from document analysis, as a means of triangulation
(Bowen, 2009). Triangulation is a process of using
several sources of evidence to clarify meaning and
verify the repeatability of an interpretation (Stake,
2005).
We analysed the collected data of two out-patient
histories using qualitative content analysis
(Graneheim and Lundman, 2004). Thematic analysis
(Fereday and Muir-Cochrane, 2006) was used to
fine-tune the analysis.
3 INSIGHT OF THE PATIENT
HISTORIES
In this section, we introduce the patient histories and
explain how we analysed our data. First, we briefly
describe the two out-patient histories. Second, we
present the process of our analysis.
3.1 The Out-patient Histories
The first patient history covered a period of ten and
a half months. Different places were involved in this
case, including a GP centre and two hospitals.
Several stakeholders were involved: a patient, GP,
secretary, radiologist, minimum two specialists,
health secretaries, and nurses from the hospitals.
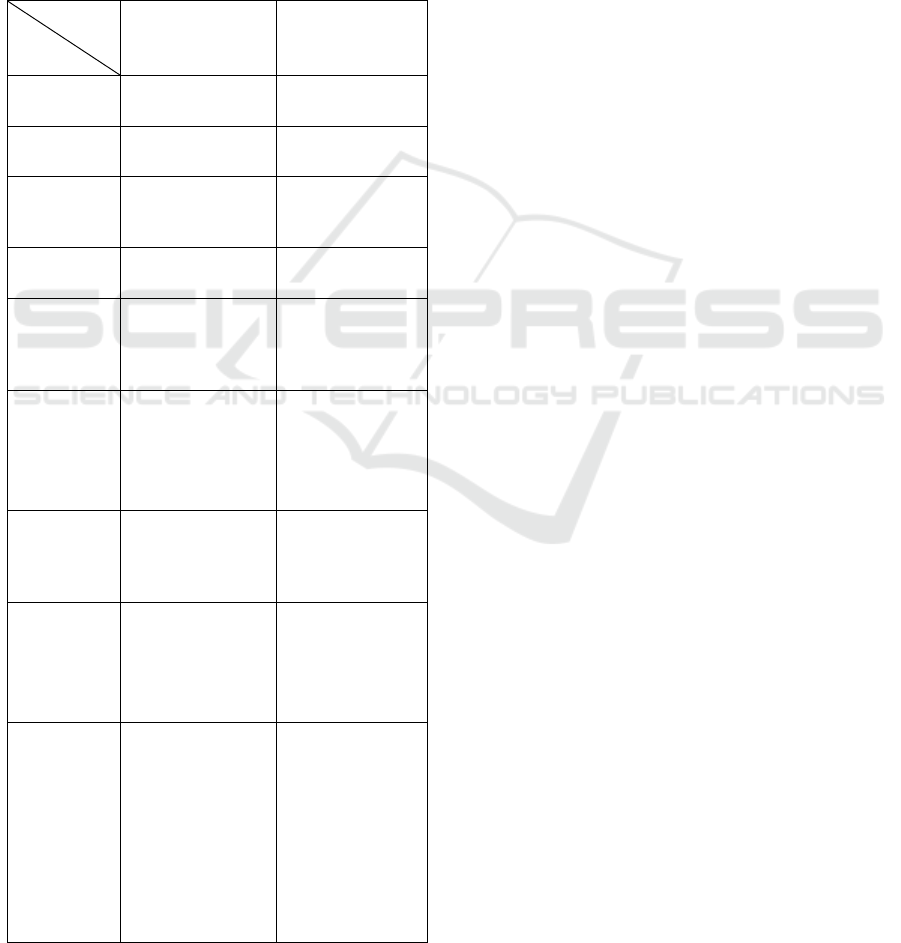
Three different health information systems were
used: a GP’s EHR system, a radiology information
system (RIS), and a hospital EHR system. These
systems were used to store and share the patient
related information. The GP’s EHR system and the
RIS could communicate with the hospital EHR
system in a limited degree (e.g., sending and
receiving electronic referrals or results of computed
tomography (CT)).
The second patient history covered a period of
two and a half months until the time of the interview
and was still ongoing. Different places were
involved in this case, including a GP centre and
three hospitals. Even more stokeholds were
involved: a patient, GP, radiologist, two
pathologists, minimum three specialists, secretaries,
health secretaries, and nurses from the different
hospitals. Four different health information systems
were used: a GP’s EHR system, a RIS, and two
different types of hospital EHR systems. The GP’s
EHR system and the RIS could communicate with a
hospital EHR system in a limited degree, like in the
first case. However, the other hospital EHR system
could not communicate with the three other systems
at all. Therefore, more interactions with physical
evidence, such as a postal letter, were generated to
cover the communication barrier (e.g., a specialist
received a referral via postal letter).
Figure 1 shows the communications between the
stakeholders in the first out-patient case and
Figure 2
shows the communications between the health
information systems in the first out-patient case.
Identifying Key Components of Services in Healthcare in the Context of out-Patient in Norway
355
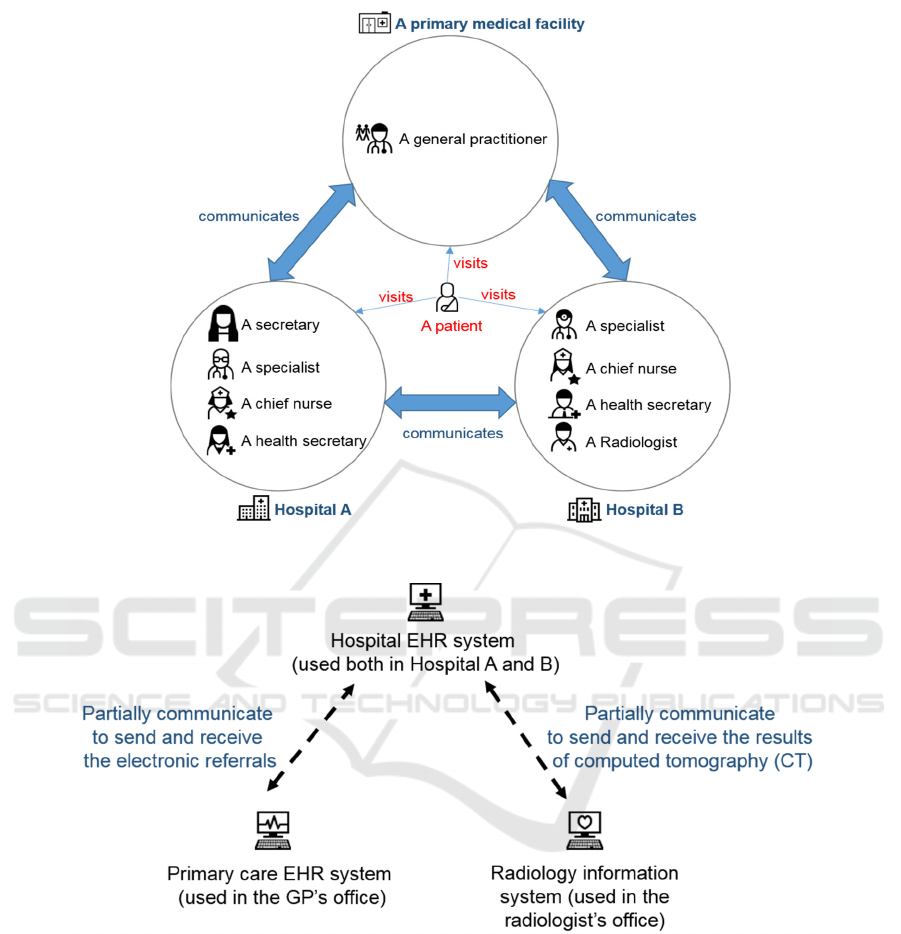
Figure 1: Communications between the stakeholders in the first out-patient case.
Figure 2: Communications between the health information systems in the first out-patient case.
3.2 Data Analysis Process
Based on the data collected in the researcher’s notes,
audio files, and photos taken, we constructed each
patient’s journey using excel spreadsheet. We
identified key components of services in healthcare
by improving the templates of the journeys in an
iterative manner.
We constructed the first version of the journeys
using a ‘service blueprint (Stickdorn and Schneider,
2010)’ method which includes the roles of the
involved stakeholders, the places where the events
happened, and the contexts of the events. We found
that the stakeholder is either service customer or
worker, and that the place is the service setting. We
learnt the events can be recognised as small units
constituting the entire service provision. Therefore,
we call the context of the event as sub-service
provision context and add it as a key component of
services in healthcare.
We then constructed the second version of the
journeys by improving the first version. While we
HEALTHINF 2017 - 10th International Conference on Health Informatics
356

were doing this, we discovered that some events
contain a sender, a receiver and an object. We also
added the date for each event in the second version.
We learnt that the date can be recognised as an
indicator in the service process.
Finally, we could develop a systematic template
that shows the patients’ journeys (third version). We
added the overall aim of the service and the
identifier for each event. We distinguished the event
involving a sender, receiver and object as a
touchpoint that indicates an interaction between two
stakeholders. We also found that each touchpoint
contains a communication channel that is used in
order to deliver the object to the receiver. We
identified the other events as actions when there is
no such interaction. We discovered that some
touchpoints are electronic-based, occurring in or
between the health information systems. For
example, an electronic referral was sent from a GP’s
EHR system to a Hospital A’s EHR system. We
found that these health information systems can be
seen as stakeholders that contribute to out-patient
services. In addition, we identified various types of
interaction in the patients’ histories: human-to-
human interaction (face-to-face or via telephone),
human-to-physical evidence interaction, and human-
to-computer interaction. We call the aim of the
service as service objective and the type of
interaction as service interaction type and add these
as key components of services in healthcare.
People producing or maintaining an EHR system
have influence on the interactions between a
healthcare professional and the EHR system. We
regard these people as secondary service workers.
A patient can be affected by an interaction between a
healthcare professional and an EHR system. In this
context, we regard the patient as a secondary
service customer.
4 COMPONENTS OF SERVICES
IN HEALTHCARE
In this section, we first present the key components
of services in healthcare, which we identified during
our data analysis. We then present two examples
(one for health service and one for eHealth service)
of the services according to the key components we
analysed from the patient histories.
4.1 Components of Health and eHealth
Services in Out-patient Context
The out-patient histories include interactions situated
in health service and in eHealth service. Here we
define a health service as a conventional medical
service not containing any interactions via electronic
channels. We define an eHealth service as a service
containing interactions via electronic channels. We
identified the key components of health service and
eHealth service separately.
The objective of the interactions situated in the
health services was treatment. Thus, the service
customers were the patients and the secondary
service customers might be family members of the
patients. The service workers were the healthcare
professionals from different groups and
organisations, like a GP and a nurse. The setting of
the interactions situated in the health services were
either a medical facility (e.g., a hospital) or a
location where the patient has a touchpoint (e.g., a
patient reads a postal letter at home or answers a
phonecall at work). The processes of the health
services were sequences of actions and touchpoints
of the patients and the healthcare professionals. We
found that the interaction type situated in the health
services was either human-to-human interaction
(e.g., a GP examines a patient.) or human-to-
physical evidence interaction (e.g., a GP reads a
postal letter from a hospital.). The health services
involved sub-services (smaller units constituting the
service) for the service objective (patient treatment).
The sub-service provision context of the health
services was either a service worker provides a
service to a service customer (e.g., a surgeon
operates on a patient to treat a disease.) or a service
worker provides a service to another service worker
(e.g., a health secretary in a hospital sends an out-
patient note to a GP via postal letter.).
The objective of the interactions situated in the
eHealth services was efficient communication
among healthcare professionals. Therefore, the
service customers were the healthcare professionals
from different groups and organisations, while the
patients became the secondary service customers.
The service workers of the eHealth were the health
information systems such as EHR and RIS, while the
secondary service workers might be people
producing or maintaining the health information
systems. The setting of the interactions situated in
eHealth service was the health information system
software. The processes of the eHealth services were
sequences of touchpoints via the health information
systems. We found that the service interaction type
Identifying Key Components of Services in Healthcare in the Context of out-Patient in Norway
357
situated in the eHealth services was human-to-
computer interaction (e.g., a specialist dictates an
out-patient note through an EHR system). The sub-
service provision context of the eHealth services was
a service worker provides an e-service to a service
customer (e.g., a GP’s EHR system stores a referral,
which can be seen electronically by a secretary in a
hospital’s post centre.)
Table 1 shows the
components we identified as the result of our data
analysis.
Table 1: Components of health and eHealth services in
out-patient context in a hospital in Norway.
Service
type
Component
Health
service
eHealth
service
Service
objective
Treatment
Efficient
communication
Service
customer
Patient
Healthcare
professional
Secondary
service
customer
Family member of
a patient
Patient
Service
worker
Healthcare
professional
Health information
system
Secondary
service
worker
None
People producing
or maintaining the
health information
system
Service
setting
A medical facility
or
a location where a
patient has a
touchpoint
Health information
system software
Service
process
Sequence of actions
and touchpoints of
a patient and health
professionals
Sequence of
touchpoints via
health information
systems
Service
interaction
type
Human to human
or
Human to physical
evidence
interaction
Human to
computer
interaction
Sub-service
provision
context
A service worker
provides
a service to a
service customer
or
A service worker
provides
a service to
a service worker
A service worker
provides an e-
service to a service
customer
4.2 Examples
In this section, we present two examples of the
services according to the key components we
identified. First, we show one example for health
service and then we show one example for eHealth
service.
The following example shows the components
we identified using a part of a hypothetical episode,
in which a patient visits a specialist in a hospital.
Service process: A patient comes to a
specialist’s office room, the specialist talks with
the patient about his/her condition, and then the
specialist examines the patient using a
stethoscope.
Service customer: The patient
Secondary service customer: A spouse of the
patient who accompanies the patient
Service worker: The specialist
Secondary service worker: None
Service setting: An office room for the
specialist at an out-patient clinic in a hospital
Service interaction type: Human to human (the
specialist to the patient) interaction
Sub-service context: A service worker (the
specialist) provides a service (examination with
stethoscope) to a service customer (the patient).
Service objective: Treatment
The following example shows the components
we identified using a part of hypothetical episode
that a specialist writes an out-patient note.
Service process: The specialist navigates to a
dictation module in a desktop-based EHR
system and dictates an out-patient note into the
system.
Service customer: The specialist
Secondary service customer: The patient
Service worker: The EHR system the specialist
uses
Secondary service worker: The people who
produce and maintain the EHR system
Service setting: A desktop-based EHR system
software
Service interaction type: Human to computer
(the specialist to the EHR software) interaction
Sub-service context: A service worker (the
desktop-based EHR system software) provides
an e-service (electronic dictation service) to a
service customer (the specialist).
Service objective: Efficient communication
HEALTHINF 2017 - 10th International Conference on Health Informatics
358

5 DISCUSSION
In this section, we discuss the above-mentioned
results. We especially focus on the additional
components we identified in the out-patient services
during the iterative process of our analysis.
5.1 Service Type: Service vs. e-Service
Characteristics of e-services are different from the
ordinary services since e-services involve
interactions via electronic channels. Väänänen-
Vainio-Mattila et al. (2009) claim that the
characteristics of the service experience
(inseparability, variability, perishability, and
intangibility) are recognised for ordinary services
and do not apply directly to e-services. Therefore,
the components affecting ordinary service and e-
service experience might be different from each
other. We identified components of health service
and eHealth service separately. We found that these
components are not contradictory each other, but
rather complement each other. For example, the
eHealth service in the sub-section 4.2 can be
followed after the health service in the sub-section
4.2 is done. But, it is also possible that an eHealth
service comes before or during a health service. For
example, the specialist can check the patient’s
information via the desktop-based EHR system
software (In other words, the desktop-based EHR
system software provides an electronic patient
information look-up service to the specialist.) before
the patient comes into his/her office. We suggest that
all of the components should be considered when
designing services in healthcare, because today’s
healthcare involves both health service and eHealth
service. Holmlid and Evenson (2008) also argued
that identifying clear genres (in this paper, we call
these service type) and the components offers
efficiency in service design.
5.2 Service Objective
In our case study, the purpose of the health service
was providing treatment to the patients. However, in
the eHealth service perspective, the purpose
becomes efficient communication among healthcare
professionals. Concerning these service objectives, it
might be beneficial to better orchestrate the actions
and touchpoints in service experience when
designing services in healthcare.
5.3 Secondary Service Customer and
Worker
In service dominant logic (Chandler and Vargo,
2011), interactions hidden from customers are not
considered in value co-creation (Wetter-Edman et
al., 2014). However, those interactions can affect the
customers’ service experience. For example, a
patient’s experience can be affected by the
interactions between his/her GP and an EHR system.
Alsos and Svanæs (2011) introduced the concept of
primary and secondary user in eHealth services
context. A primary user indicates a person who uses
an information system directly, and a secondary user
points out a person who relies on the primary user to
get information from the system and who is affected
by the primary user’s experiences with the system
(Alsos and Svanæs, 2011). In the eHealth service
context, the patient becomes a secondary service
customer and people producing/maintaining health
information systems become secondary service
workers. On the other hand, in a health service
context, the family members of a patient become
secondary service customers. Holmlid (2007) argued
that the customer’s customer (secondary service
customer) is as important as the customer in service
design. We postulate that considering not only
secondary service customer, but also secondary
service worker when designing a service, might
contribute to better understanding the whole service
delivery.
5.4 Service Interaction Type
A service consists of different types of interactions.
“The service perspectives become a challenge to
interaction design, and technology usage becomes a
challenge to service design (Holmlid, 2007).”
Paying attention on those types and considering
them in appropriate manners when evaluating and
designing service might be helpful to create
consistency in service provision.
5.5 Sub-Service Provision Context
In a broad and holistic perspective, a service can
contain several sub-services. For instance, an air
travel service consists of sub-services, such as
check-in, providing meal on the plane etc. In
healthcare, many actors are connected to each other
to solve specific tasks and eventually pursuit the
ultimate goal: maximising health of the population
in the society (Coast, 2004). Considering such sub-
service provision types, it would be helpful to better
Identifying Key Components of Services in Healthcare in the Context of out-Patient in Norway
359

coordinate various interactions between different
actors and systems in services in healthcare. In our
case, no ubiquitous computing or pervasive
technology originated sub-service was found.
However, it might appear more and more in future
services as the technology advances. Since the
interactions originated from ubiquitous computing or
pervasive technology happen without the customer’s
direct control (Cellary, 2015), it can be more
challenging for us to well integrate them in service
delivery.
6 LIMITATIONS
There are different types of eHealth service
depending on who communicates with whom. We
conducted our case study with eHealth services
where healthcare professionals communicate with
each other. Thus, the key components in other types
of eHealth service (e.g., telepsychiatry where a
psychiatrist communicates with a patient) might be
different from what we identified.
Our case study was conducted with desktop-based
eHealth services. Conducting a case study with a
mobile-based eHealth service might lead to the
results that are not the same as what we found from
our case study.
7 CONCLUSION
Our research reveals that out-patient care includes
interactions situated in both health service and in
eHealth service. We found that these two different
types of service consist of different components. We
expanded the Fisk et al. (2013)’s four components of
service (service customer, service worker, service
setting, and service process) for services in
healthcare by adding five new components: service
objective, service interaction type, sub-service
provision context, secondary service workers, and
secondary service customer. Considering these
components when evaluating service experience
might support an analytical way of understanding
the complexity in service delivery process in
healthcare. This understanding might contribute to
designing more stakeholder-oriented services in
healthcare.
There is a need for a holistic and stakeholder-
centred approach in designing and evaluating
eHealth services. “the effectiveness of emerging
eHealth technologies in improving the processes or
outcomes of healthcare is unproven (Pagliari,
2007).” We envision further research in the form of
empirical studies that consider the key components
of services in healthcare when evaluating or
designing services in healthcare. Investigating how
to present or document all the actions and
touchpoints of a service delivery process in more
holistic way might also be interesting. Our research
is based on document analysis, observation, and
interview because of the challenges in conducting
ethnography study with patients due to ethical
consideration. Thus, we are also interested in
investigating how to collect richer data that can
provide a deeper insight of services in healthcare.
ACKNOWLEDGEMENTS
The research presented here has been conducted
within the VISUAL project (project number 219606)
funded by the Research Council of Norway. Thanks
to Ragnhild Halvorsrud for helping me arranging
data collection activities for the case study, to Maja
Van Der Velden and Stefan Holmlid for guidance in
writing this paper, to our industrial partner for the
contribution. Above all, we thank the participants
who provided data for the case study.
REFERENCES
Alsos, O.A., Svanæs, D., 2011. Designing for the
secondary user experience. In INTERACT 2011, 13th
International Conference on Human-Computer
Interaction. Springer-Verlag. pp. 84–91.
Baxter, P., Jack, S., 2008. Qualitative case study
methodology: Study design and implementation for
novice researchers. The qualitative report 13, 544–
559.
Bowen, G.A., 2009. Document analysis as a qualitative
research method. Qualitative research journal 9, 27–
40.
Cellary, W., 2015. e-Service-dominant Logic. In AHFE
2015, 6th International Conference on Applied Human
Factors and Ergonomics and the Affiliated
Conferences. Procedia Manufacturing. pp. 3629–3635.
Chandler, J.D., Vargo, S.L., 2011. Contextualization and
value-in-context: How context frames exchange.
Marketing Theory 11, 35–49.
Coast, J., 2004. Is economic evaluation in touch with
society’s health values? BMJ 329, 1233–1236.
Fereday, J., Muir-Cochrane, E., 2006. Demonstrating rigor
using thematic analysis: A hybrid approach of
inductive and deductive coding and theme
development. International journal of qualitative
methods 5, 80–92.
HEALTHINF 2017 - 10th International Conference on Health Informatics
360

Fisk, R., Grove, S., John, J., 2013. Services Marketing An
Interactive Approach, Cengage Learning. USA, 4th
edition.
Gadrey, J., 2002. The misuse of productivity concepts in
services: Lessons from a comparison between France
and the United States. Edward Elgar Publisher.
Graneheim, U.H., Lundman, B., 2004. Qualitative content
analysis in nursing research: concepts, procedures and
measures to achieve trustworthiness. Nurse Education
Today 24, 105–112.
Hesse, B.W., Shneiderman, B., 2007. eHealth Research
from the User’s Perspective. American Journal of
Preventive Medicine 32, 97–103.
Holmlid, S., 2007. Interaction design and service design:
Expanding a comparison of design disciplines. Nordes
(Nordic Design Research).
Holmlid, S., Evenson, S., 2008. Bringing Service Design
to Service Sciences, Management and Engineering, in:
Hefley, B., Murphy, W. (Eds.), Service Science,
Management and Engineering Education for the 21st
Century, Service Science: Research and Innovations in
the Service Economy. Springer US, pp. 341–345.
Lazar, J., Feng, J.H., Hochheiser, H., 2010. Research
methods in human-computer interaction. Wiley.
Mitchell, J., 2000. Increasing the cost-effectiveness of
telemedicine by embracing e-health. J Telemed
Telecare 6, 16–19.
Pagliari, C., 2007. Design and Evaluation in eHealth:
Challenges and Implications for an Interdisciplinary
Field. J Med Internet Res 9.
Reichert, M., 2011. What BPM Technology Can Do for
Healthcare Process Support, in: Peleg, M., Lavrač, N.,
Combi, C. (Eds.), Artificial Intelligence in Medicine.
Springer Berlin Heidelberg, pp. 2–13.
Rodolfo, I., Laranjo, L., Correia, N., Duarte, C., 2014.
Design Strategy for a National Integrated Personal
Health Record. In NordiCHI ’14, 8th Nordic
Conference on Human-Computer Interaction: Fun,
Fast, Foundational. ACM. pp. 411–420.
Rogers, Y., Sharp, H., Preece, J., 2011. Interaction
Design: Beyond Human Computer Interaction, Wiley.
3rd edition.
Stake, R.E., 2005. Qualitative Case Studies, in: The SAGE
Handbook of Qualitative Research. Sage Publications,
pp. 443–466.
Stickdorn, M., Schneider, J., 2010. This is service design
thinking. Wiley.
Väänänen-Vainio-Mattila, K., Väätäjä, H., Vainio, T.,
2009. Opportunities and Challenges of Designing the
Service User eXperience (SUX) in Web 2.0, in:
Isomäki, H., Saariluoma, P. (Eds.), Future Interaction
Design II. Springer London, pp. 117–139.
Wetter-Edman, K., Sangiorgi, D., Edvardsson, B.,
Holmlid, S., Grönroos, C., Mattelmäki, T., 2014.
Design for Value Co-Creation: Exploring Synergies
between Design for Service and Service Logic.
Service Science 6, 106–121.
Yin, R., 1994. Case study research: Design and methods.
Sage publishing. Beverly Hills. CA,
Identifying Key Components of Services in Healthcare in the Context of out-Patient in Norway
361
