
Implementation of Machine Learning for Breath Collection
Paulo Santos
1,2
, Valentina Vassilenko
1,2
, Fábio Vasconcelos
1
and Flávio Gil
2
1
Laboratory for Instrumentation, Biomedical Engineering and Radiation Physiscs (LibPhys-UNL), Faculdade de Ciência e
Tecnologias da Universidade NOVA de Lisboa, Campus FCT UNL, 2896-516 Caparica, Portugal
2
NMT, S.A., Edíficio Madan Parque, Rua dos Inventores, 2825-282 Caparica, Portugal
Keywords: Exhaled Air, Selective Air Acquisition, Air Sampling/Monitoring, Breath Rhythm Imposition, Modelled
Breath Algorithm, Average Time of Expiration, Machine Learning Algorithm.
Abstract: Economic and technologic progresses states the analysis of human’s exhaled air as a promising tool for
medical diagnosis and therapy monitoring. Challenges of most pulmonary breath acquisition devices are
related to the substances’ concentrations that are source (oral cavity, esophageal and alveolar) dependent and
their low values (in ppb
v
- ppt
v
range). We introduce a prototype that is capable of collecting samples of
exhaled air according to the respiratory source and independent of the metabolic production of carbon dioxide.
It also allows to access the breathing cycle in real-time, detects the optimized sampling instants and selects
the collection pathway through the implementation of an algorithm containing a machine learning process. A
graphical interface allows the interaction between the operator/user and the process of acquisition making it
easy, quick and reliable. The imposition of breath rhythm led to improvements in accuracy of obtaining
samples from specific parts of the respiratory tract and it should be adapted according to their age and
physiological/health condition. The technology implemented in the proposed system should be taken into
consideration for further studies, since the prototype is suitable for selectively sampling exhaled air from
persons according to its age, genre and physiological condition.
1 INTRODUCTION
The detection and measurement of exhaled
substances is advantageous as a reliable, reproducible
and non-invasive diagnostic and prognostic tool in a
wide variety of medical conditions to assess different
vital organ functions (Miekisch et al., 2004;
Baumbach et al., 2009; Di Francesco et al., 2005;
Manolis et al., 1983; Miekisch et al., 2006; Amman
et al., 2007; Dweik et al., 2008). The human exhaled
air accommodates a complex mixture of molecules
which are expelled in every breath (~75% of nitrogen,
~15% of oxygen, ~5 of carbon dioxide (CO
2
) and
~6% of water vapour, inorganic compounds, volatile
organic compounds (VOCs) and aerosols). By
measuring the concentration of those molecules, it is
possible to quantify each person’s individual score
reflecting the state of health (Lourenço et. al, 2014).
There are different main targets in the analysis of
exhaled air capable to identify potential diseases, but
VOCs are the most studied and interesting to look for
as biomarkers of pathological conditions (Miekisch et
al., 2004; Baumbach et al., 2009; Di Francesco et al.,
2005; Manolis et al., 1983; Miekisch et al., 2006;
Amman et al., 2007; Dweik et al., 2008; Lourenço et
al., 2014; Mazzatenta et al., 2013). The concentration
of these compounds in the exhaled air varies
depending on the respiratory origin of exhaled air to
be analyzed, including oral cavity, esophageal and
alveolar air (Phillips et al., 1999; Di Natale et al.,
2014; Ruzsanyi et al., 2013).
Furthermore, the concentration of most of the
VOCs present in the exhaled air is very low (ppb
v
–
ppt
v
or µgl
-1
– ngl
-1
range). Thus, the detection of such
small amounts in fractions of exhaled air from
different respiratory origins has revealed itself one of
new challenges to overcome in the most recent
pulmonary breath sampling devices.
Even though there are several studies in this field,
the clinical importance of these compounds is yet to
be discovered. This work does not aim to evaluate any
group of compounds or specific VOCs. Instead, focus
will be given to the process of exhaled air sampling
according to user’s characteristics by evaluating the
influence of imposing a controlled breath rhythm.
These aspects obviously can influence the studies
involving the analyses of samples containing these
compounds.
Santos P., Vassilenko V., Vasconcelos F. and Gil F.
Implementation of Machine Learning for Breath Collection.
DOI: 10.5220/0006168601630170
In Proceedings of the 10th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2017), pages 163-170
ISBN: 978-989-758-216-5
Copyright
c
2017 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
163
1.1 Breath Sampling Devices
Multiple apparatus and methods are used in breath
studies, which in general are performed with patients
either providing their breath for storage and
subsequent later analysis (offline analysis) or
breathing directly into the analyzer for immediate
analysis (online analysis). Different approaches are
used, depending on the breath constituents to analyze,
being gas-phase the more indicated for VOC analysis
(Beauchamp et al., 2015). Nevertheless, controlling
breath sampling is crucial to enable the identification
of part of the respiratory tract from which the sample
derived and to ensure that comparative data is
generated between studies. The control is actually
made by using CO
2
, flow, pressure temperature or
humidity sensors (Beauchamp et al., 2015).
However, there are several constraints while
sampling the exhaled air for analysis (Alonso et al.,
2013). Despite different breath sampling
methods/devices used and several types of analysis
developed in the last decade, most of them are lacking
in accuracy and precision in the collection of an
exhaled air sample (Alonso et al., 2013). The
technology used in exhaled air collection, introduce
high variability in breath samples due to: the way the
air is expelled, the breath frequency, the length and
depth of the breath cycle and the mental and physical
condition of the patient (Basanta et al., 2007; Droz et
al., 1986; Risby, 2008).
1.2 Respiratory Cycle Monitoring
The real time monitoring of the patient’s respiratory
cycle allows the identification of respiratory phases
and the definition of the instants for breath collection.
The identification of the alveolar air portion assumes
critical importance due to the presence of diverse
constituents from endogenous origin in equilibrium
with the alveolar capillary blood vessels.
Presently the most used method for identification
of the different phases of the breathing cycle is the
capnography which allows to monitor the
concentration or partial pressure of carbon dioxide
(PCO
2
) in the respiratory gases by providing
information about the production of carbon dioxide,
pulmonary perfusion, alveolar ventilation and
respiratory patterns (Bhavanishankar et al.,
1995;
Mimoz et al., 2012; Bhavanishankar et al.,
1992).
Yet, the use of capnography has some limitations
regarding the collection of selective samples of
exhaled air, because it varies with (a) the inherent
variation of breath composition and concentration of
each constituent throughout the breathing cycle; (b)
the speed of the breath, which affects the composition
of the mixture between alveolar air and dead space
air; (c) the depth and frequency of breathing, which
control changes from autonomous to conscious
breathing, when a person is asked to provide a sample
of breath.
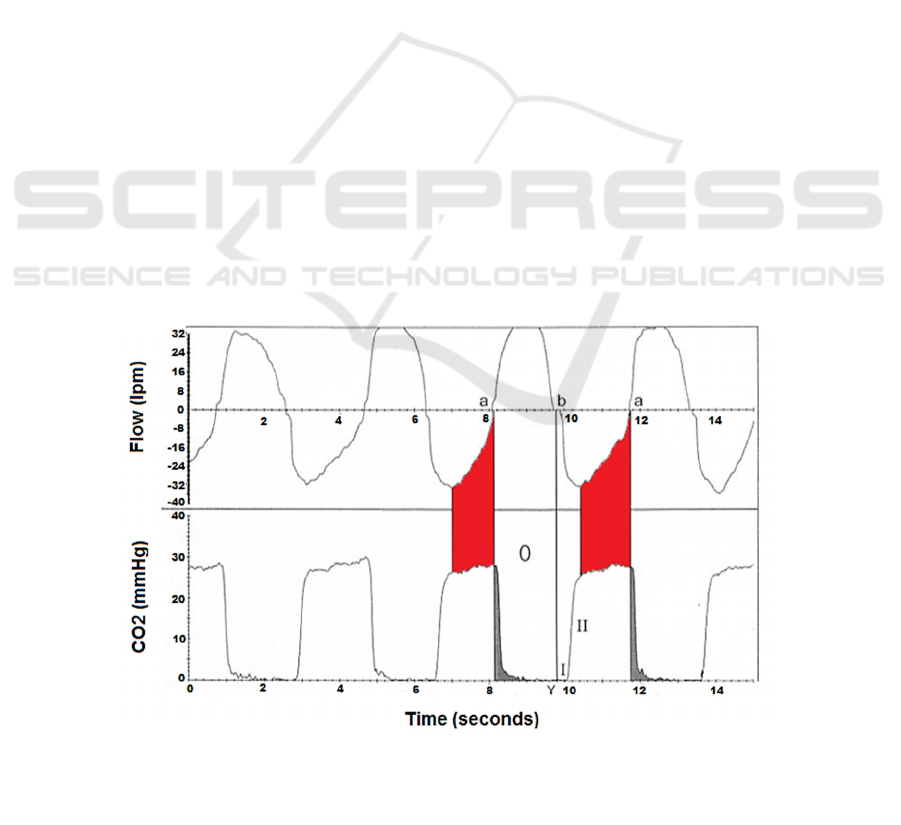
Figure 1: Graphical comparison between respiratory flow rate (at the top) and time capnogram (at the bottom). The ab segment
represents inspiration and the ba segment represents expiration on the respiratory waveforms. The red area represents the
alveolar air region, while the shaded area under the CO
2
curve represents the inspiratory phase of the respiratory cycle, thus
constituting rebreathing. (Adapted from Bhavani-Shankar and Philip, 2000).
BIODEVICES 2017 - 10th International Conference on Biomedical Electronics and Devices
164
Despite the possibility of diagnose several diseases,
the modifications in the shape of capnograms (related
with such diseases) also difficult clear identification
of the expiratory segments (Kodali et al., 2013).
The problems remaining to be solved comprise
the question of how to achieve accurate, selective and
repeatable sampling, how to ensure easy and safe
handling, and maybe most importantly, the issue of
sample stability to allow a proper chemical analysis.
Therefore, the actual research in breath analysis tries
to pursue a suitable device and a precise protocol for
sampling exhaled air independently of the subject’s
metabolic production of CO
2
, the smoking habits, the
type of food eaten, the stomach, esophagus and mouth
condition of the patients.
Bear that in mind, this particularly work aims to
describe the influence of the implementation of
machine learning for selective breath sampling by
using a novel technology where a respiratory cycle
model is adapted to individual breathing
characteristics of the user.
2
BREATH MODELLING & ITS
IMPLEMENTATION
Due to the above mentioned limitations of the
capnography and, since the measurement of the
respiratory flow rate may yield the same effect of
determining the respiratory phases in a cheaper and
easier way, both were compared to identify the region
corresponding to the alveolar air and to modulate it in
a mathematical function. By overlapping a time
capnogram with a fluxogram (Bhavani-Shankar and
Philip, 2000), the area related to the end-tidal breath
was clearly identified (figure 1). Considering that,
only a flowmeter can be used for selective assessment
to the last segment of the expiration in a fluxogram
which corresponds to the alveolar region with higher
CO
2
concentration.
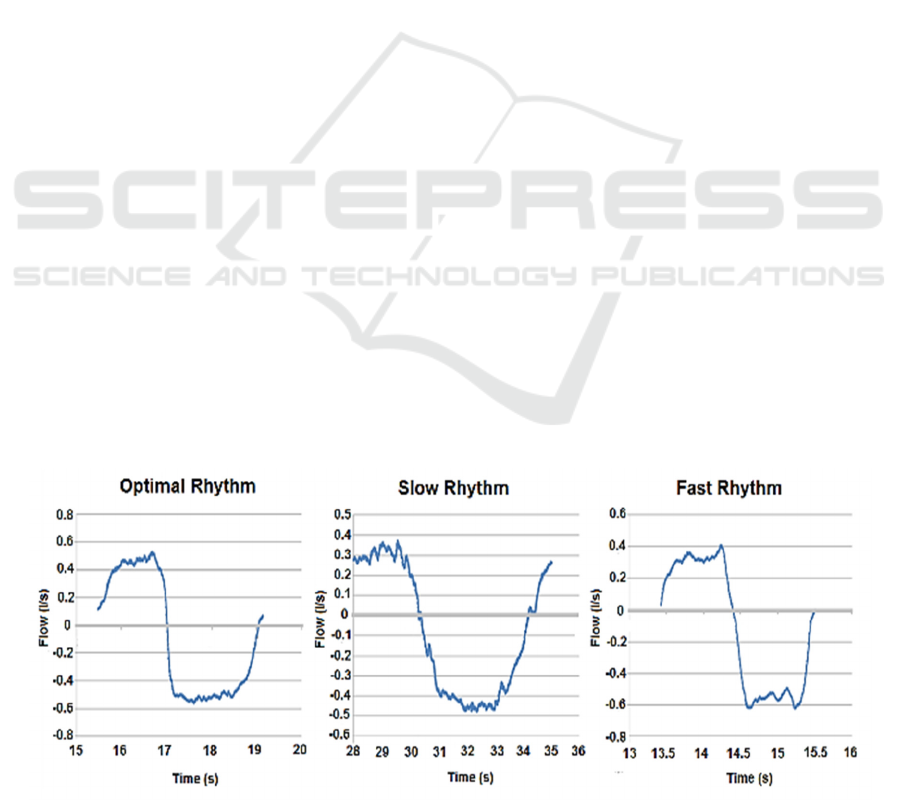
2.1 Respiratory Cycles’ Modelling
The collection of selective portions of exhaled air by
using respiratory flow measurements, implies the use
of reference respiratory rhythms for the users to
follow. By measuring the exhaled air flow of multiple
subjects and by determining the total time of each
respiratory cycle and the transition between
respiratory phases (inspirations and exhalations),
Vassilenko et. al. (2013) were able to calculate
average signals that best describe three breathing
rhythms (slow, normal and fast). The average signals
for the three respiratory rhythms are shown in figure
2 and were used as references for development of
mathematical models which precisely characterises
breath rhythms of every patient (Vassilenko et al.,
2013).
Since it overcomes the disadvantages regarding
the imprecise identification of selective portions of
exhaled air (associated with variable depth and
frequency of breathing), the proposed method for
monitoring and selective sampling of exhaled air
through respiratory flow sensing represents a reliable
alternative method to capnography approaches.
2.2 Implementation of Respiratory
Cycles’ Models
The prototype developed by the authors performs real
time flow measurements and captures alveolar air by
synchronizing modelled respiratory cycles with the
user’s breathing cycle. The prototype comprises
hardware cells controlled by an intelligent control
software loaded on several computing devices
Figure 2: Representation of the average signals obtained for each pace imposed to tested individuals (Vassilenko et al., 2013).
Implementation of Machine Learning for Breath Collection
165
(laptops, desktops, smartphones, tablets, etc.). The
hardware module is responsible for data acquisition,
processing and its transmission to the software, and
for channeling the portion of exhaled air through the
sampling or elimination outlets.
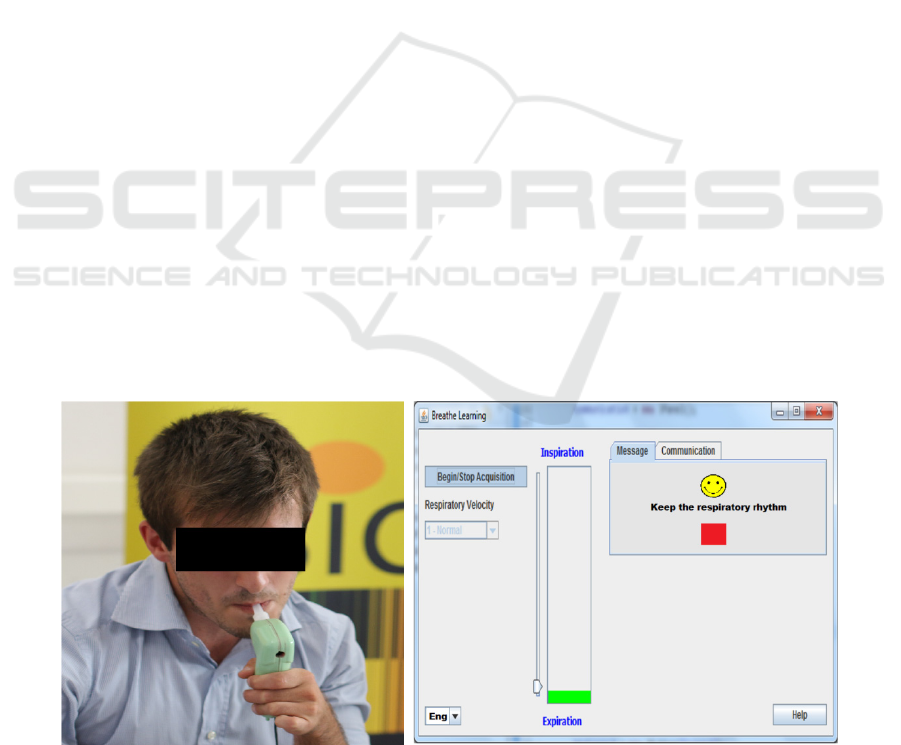
The software comprises a graphical interface
that imposes a breathing pace to the user according to
its age, gender and physiological state and, by using
an algorithm identifies the instants of sampling and
communicates with the hardware to trigger the
sample to be stored either in a bag or go directly to an
analytical analyser. Both of that software components
were updated with the implementation of a machine
learning process in the algorithm and the imposition
of breath rhythm to the user according to its age.
The algorithm implemented in the intelligent
control software was configured to: measure the
user’s respiratory flow; detect user’s breathing
frequency; distinguish inspiratory and expiratory
breath phases; synchronize the user’s respiratory
cycle with the representative and modeled respiratory
cycle; and to calculate the average time of expiration
of the user. The average time of expiration allows the
selection the fraction of exhaled air to sample.
The machine learning process implemented in
the algorithm of the software is based on the
continuous calculation and saving of the average
exhalation time values, allowing the prediction of the
time of occurrence of a new expiration and,
consequently, the prediction of the precise time-frame
for the acquisition of the fraction of exhaled air to
sample. By this way, the machine learning process
learns the respiratory cycle of the user, and test it on
the modelled respiratory intrinsically contained in the
algorithm of the software.
In addition to the definition of global variables of the
operation and from the subject (genre, age and
physiological/health condition), the graphical
interface also provides a feedback mechanism for
communicating with the user/operator. This feedback
mechanism presents a central part of the system
because it provides multiple indicators for showing
the breathing rhythm to be followed by the user or if
the moments of breath air acquisition are occurring.
According to the information defined in the
graphical interface, the user is asked to breathe
according to a specific respiratory rhythm (figure 3).
When the breathing pace of the user is matched the
representative and modelled respiratory cycle, the
initial and final instant of the exhaled air’s fraction of
interest is identified in the respiratory cycle. This
information is communicated with the remaining
system of device in order to sample the portion of
interest of exhaled air between these instants. This
process ensures that only a fraction of exhaled air is
diverted to a collection reservoir or directly analysed
by an analytical analyser.
3 TESTS OF PERFORMANCE
To evaluate the effectiveness of the machine learning
process implemented on the software of the prototype
and the influence of a breath rhythm imposition, two
groups of individuals with different age groups (15
patients between 2 and 5 years old – children – and
30 within 18 and 27 years old – university students)
were asked to make breathing test in the prototype.
The patients had to achieve the beginning of breath
collection and, simultaneously, the minimum number
Figure 3: Prototype for alveolar air collection used on experimental tests (on the left) and the graphical interface related with
breath rhythm imposition to the user (on the right).
BIODEVICES 2017 - 10th International Conference on Biomedical Electronics and Devices
166
of cycles, the time required to start breath sampling
and the average time of exhalation (ATE) were
registered. This method was applied two times for
each individual, in which firstly patient’s autonomous
breath rhythm was suggested and then with a
respiratory pace imposition to the subject through the
feedback present on the graphical interface.
3.1 Number of Respiratory Cycles
The results show that the number of cycles needed to
begin breath sampling are lower when a breath
rhythm was imposed to both groups of patients. More
specifically, when the university students breathed
autonomously, the number of cycles registered till the
acquisition started are higher (9.70 ± 2.22; mean ±
standard deviation) comparably with the same
number for an imposed breathing (8.56 ± 2.12). The
results are more evidently with children when
comparing the number of respiratory cycles needed to
initiate the sampling by an autonomous breathing
(17.61 ± 3.31) and an imposed one (13.93 ± 2.49).
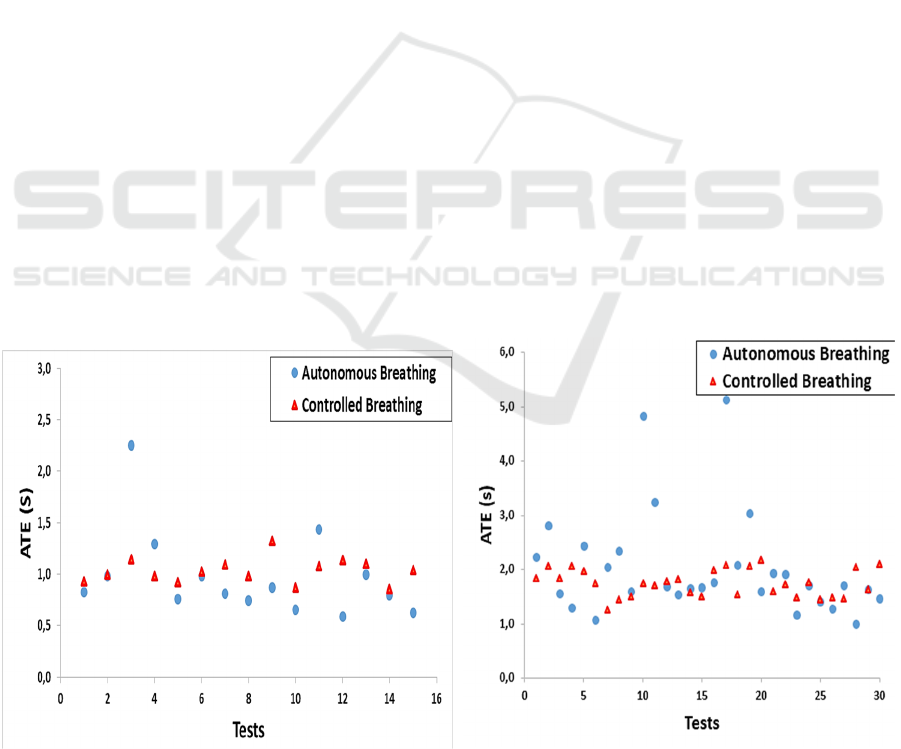
3.2 Average Time of Exhalation
The results presented in figure 4 illustrate the
comparison of the average time of exhalation (ATE)
between an imposed/controlled breathing rhythm and
an autonomous rhythm of the patients, and the
relationship of such feature for two aging groups.
For both aging groups (children and university
students), when respiratory rhythm was autonomous,
the distribution of ATEs is significantly uneven when
compared with the distribution of ATEs for an
imposed breathing rhythm. The values of the standard
deviation for an autonomous breathing (424 and 966
ms, for children and university students, respectively)
are almost 4 times higher when compared with the
corresponding values of standard deviation for the
imposed rhythm (120 and 250 ms, for children and
university students, respectively). For both
acquisition methods, the average values of ATEs are
also significantly lower for children (974 and 1032
ms, for autonomous and controlled breathing,
respectively) comparably to the older university
students (2031 and 1752 ms, for autonomous and
controlled breathing, respectively).
3.3 Time Required to Start Breath
Sampling
Figure 5 displays box and whiskers plots related to
the time necessary to begin sampling the portion of
interest of exhaled air in order to distinguish both
procedures of breath sampling (with and without an
imposed rhythm) for both aging groups.
The time required to start breath sampling
presents several differences regarding the type of
breathing applied to the patients. For children (2-5
years old), the time needed to begin sampling the
portion of interest of exhaled air with a controlled
rhythm of breathing (32.89/31.88-34.60/s;
median/interquartile range/) is lower when compared
with an autonomous breath rhythm of the patient
(35.51/33.65-41.06/s). However, this decrease in the
Figure 4: Distribution of results of average time of exhalation (ATE)) for free breath cycles (autonomous breathing) and for
an optimized imposed rhythm (controlled breathing) with children (on the left) and university students (on the right).
2 - 5 years
18 - 27 years
Implementation of Machine Learning for Breath Collection
167
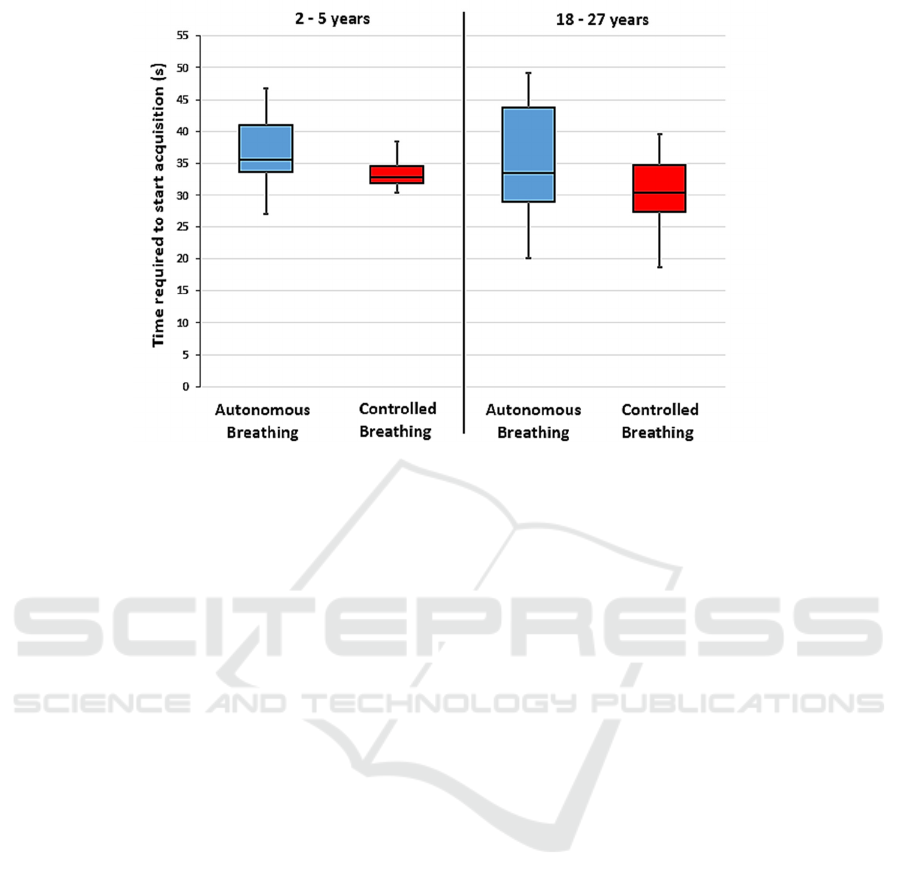
Figure 5: Time required to start breath sampling for free breath cycles (autonomous breathing) and for an optimized imposed
rhythm (controlled breathing) with children (on the left) and university students (on the right). Data are displayed in box and
whiskers plot (box depicts median with first and third quartiles, whiskers show first quartile – 1.5 interquartile range and third
quartile+1.5 interquartile range).
time required to start the sampling is not so evidently
for university students (18-27 years old) where, for an
autonomous breathing (33.59/29.04-43.73/s), this
required time is similar compared with time obtained
for an imposed breathing rhythm (30.41/27.48-
34.79). Of note, the decreased interquartile range of
the time need for breath sampling with the controlled
rhythm for both groups of patients compared with the
time obtained for an autonomous rhythm.
4 DISCUSSION
The results of performance tests applied to the
prototype show that, when concerning the number of
respiratory cycles and time needed begin the breath
sampling, the imposition of breath rhythm to the
patients (children and university) is more efficient
since less time is spent and the user is not required to
make unnecessary long breaths, which can lead to
fatigue (Roussos et al., 1996). This increased
efficiency in start of selective exhaled air sampling is
related with a quicker prediction of the time of
occurrence of a new expiration and, consequently, the
prediction the precise time-frame for its collection
which are ultimately related with the machine
learning process implemented in the prototype. These
results of the prototype’s performance tests are more
evident for children, where the suggestion of an
appropriated breath rhythm have crucial importance
due to their inability of autonomously maintain a
breath rhythm.
The results obtained for average time of
exhalation (ATE) show that the breath rhythm
imposed to patients should be adapted according to
their aging group and physiological/health condition.
Moreover, the stabilized values of ATE and the lower
interquartile range of the time required to begin
sampling the portion of interest of exhaled air, for
both aging groups, indicates the imposition of an
aging-suitable breath rhythm as the reliable way of
using the prototype for collection of exhaled air.
The majority of the existent breath samplers and
ventilators comprise several algorithms to analyse
respiration cycles of the user in order to detect
inspiration and expiration phases and to,
consequently, determine the time-window for breath
sampling. However, and for cases of dyspnea with
erratic respiratory rhythms, that determined time-
window for sampling can be too short and can
brought up multiple difficulties when obtaining such
small portions of exhaled air. Only the system
patented by Capnia, Inc. (patent number
WO2015143384 A1, 2015) is configured to impose a
breath frequency to users (young children and non-
cognizant patients) in order to avoid those erratic
respiratory episodes. Even so, that imposed frequency
does not adapts and “learns” with the user’s breathing
pace such as the proposed system does.
BIODEVICES 2017 - 10th International Conference on Biomedical Electronics and Devices
168

The protocol necessary to use the prototype, in
which the patient has to follow the directions given
by the system and try to maintain the breathing with
the same rhythm that appears on the graphical
interface, also suggests the introduction of
improvements in the accuracy and precision on
obtaining samples of a specific part of the respiratory
tract, which consequently led to the increase in the
repeatability of the analysis applied to these samples.
Furthermore, it is excluded the introduction of
variability during breath sampling related with
breathing frequency, amplitude of the respiratory
cycle, the mental and physical condition of the
patient, as well as, the method applied by the person
who asks for the patient to breathe.
5 CONCLUSIONS
The research work demonstrated herein presents a
suitable and novel technology and related protocol of
using it for selectively sampling exhaled air regarding
the subject’s: metabolic production of CO
2
, smoking
habits, type of consumed food, stomach, esophagus
and oral cavity conditions. Moreover, the
implementation of a user-dependent’s respiratory
cycle model on the prototype used in this work could
allow a more accurate way to collect portions of
exhaled air according to the exhaled air’s respiratory
origin. This collection is done from single or multiple
exhalations, for online or posterior analytical analysis
for medical diagnosis and/or therapy monitoring, in a
quick, reliable, non-invasive way, applied at any
stage of life.
The imposition of a respiratory rhythm
according to the characteristics of the user (age,
gender and physiological/health condition) and the
machine learning process implemented on the
prototype led to improvements in the accuracy in
sampling breath from specific parts of the respiratory
tract and decreases the variability of the samples
related with breath frequency, amplitude of the breath
cycle, mental and physical condition of the patient.
However, the implemented algorithm have to be
optimized for better performance in real healthcare
environments and the respiratory rhythm appearing in
graphical interface should be interactively adapted
according to all age groups, especially to the elderly
and children who have more difficulty to follow this
method. We also believe that future and similar
applications for mobile devices should be developed
to help the patients to learn and train the respiratory
rhythm while the respective portable sampling
equipment for analysis is not commercially available.
The final application should be suitable to different
group stages simplifying the breath sampling process.
ACKNOWLEDGEMENTS
The authors would like to thank all volunteers that
offered their time to perform tests for the acquisition
of their respiratory cycles and for the tests of
performance of the prototype. We thank to
parents/guardians of the children who executed the
same tests, for authorize their participation and to the
daycare of FCT (center of pre-school education) for
providing space and conditions to its implementation.
The authors would also thank the Fundação para a
Ciência e Tecnologia (FCT, Portugal) for co-
financing the PhD grant (PD/BDE/114550/2016) of
the Doctoral NOVA I4H Program.
REFERENCES
Miekisch, W, Schubert, JK & Noeldge-Schomburg, GFE
2004, ‘Diagnostic potential of breath analysis - focus on
volatile organic compounds’, Clinica Chimica Acta,
vol. 347, pp. 25-39.
Baumbach, JI 2009, ‘Ion mobility spectrometry coupled
with multi-capillary columns for metabolic profiling of
human breath’, J. Breath Research, vol. 3, pp. 16.
Di Francesco, F, Fuoco, R, Trivella, MG & Ceccarini, A
2005, ‘Breath analysis: trends in techniques and clinical
applications’, Microchemical Journal, vol. 79, pp. 405-
410.
Manolis, A 1983, ‘The diagnostic potencial of breath
analysis’, Clinical Chemistry, vol. 29, pp. 5-15.
Miekisch, W & Schubert, JK 2006, ‘From highly
sophisticated analytical techniques to life-saving
diagnostics: Technical developments in breath
analysis’, Trac-Trends in Analyt. Chem., vol. 25, pp.
665-673.
Amann, A, Spanel, P & Smith, D 2007, ‘Breath analysis:
the approach towards clinical applications’, Mini
reviews in medicinal chemistry, vol. 7, pp. 115-129.
Dweik, RA & Amann, A 2008, ‘Exhaled breath analysis:
the new frontier in medical testing’, Journal of Breath
Research, vol. 2, no. 3, 030301.
Lourenço, C & Turner, C 2014, ‘Breath analysis in disease
diagnosis: methodological considerations and
applications’, Metabolites, vol. 4, pp. 465-498.
Mazzatenta, A, Di Giulio, C & Pokorski, M 2013,
‘Pathologies currently identified by exhaled
biomarkers’, Respiratory Physiology & Neurobiology,
vol. 187, pp. 128-134.
Phillips, M, Herrera, J, Krishnan, S, Zain, M, Greenberg, J
& Cataneo, R 1999, ‘Variation in volatile organic
compounds in the breath of normal humans’, Journal of
Implementation of Machine Learning for Breath Collection
169

Chromatography B: Biomedical Science and
Applications, vol. 729, pp. 75-88.
Di Natale, C, Paolesse, R, Martinelli, E & Capuano, R 2014,
‘Solid-state gas sensors for breath analysis: A review’,
Analytica Chimica Acta, vol. 824, pp. 1-17.
Ruzsanyi, V 2013, ‘Ion mobility spectrometry for
pharmacokinetic studies-exemplary application’,
Journal of Breath Research, vol. 7, no. 4, 046008.
Beauchamp, J 2015, ‘Current sampling and analysis
techniques in breath research - results of a task force
poll’, Journal of Breath Research, vol. 9, 047107.
Alonso, M & Sanchez, JM 2013, ‘Analytical challenges in
breath analysis and its application to exposure
monitoring’, Trends in Analytical Chemistry, vol. 44,
pp. 78-89.
Basanta, M, Koimtzis, T, Singh, D, Wilson, I & Thomas,
CL 2007, ‘An adaptive breath sampler for use with
human subjetcs with an impaired respiratory function’,
Analyst, vol. 132, no. 2, pp. 153-163.
Droz, PO & Guillemin MP 1986, ‘Occupational exposure
monitoring using breath analysis’, J. Occup. Med., vol.
28, no. 8, pp. 593-602.
Risby, TH 2008, ‘Critical issues for breath analysis’,
Journal of Breath Research, vol. 2, 030302.
Bhavanishankar, K, Kumar, AY, Moseley, HSL &
Ahyeehallsworth, R 1995, ‘Terminology and the
current limitations of time capnography – A brief
review’, Journal of Clinical Monitoring, vol. 11, pp.
175-82.
Mimoz, O, Benard, T, Gaucher, A, Frasca, D & Debaene,
B 2012, ‘Accuracy of respiratory rate monitoring using
a non-invasive acoustic method after general
anaesthesia’, Br. J. Anaesth, vol. 108, pp. 872-875.
Bhavanishankar, K, Moseley, H, Kumar, AY & Delph, Y
1992, ‘Capnometry and Anesthesia’, Canadian Journal
of Anaesthesia, vol. 39, pp. 617-632.
Kodali, BS 2013, ‘Capnography outside the operating
rooms’, Anesthesiology, vol. 118, pp. 192-201.
Bhavani-Shankar, K & Philip, JH 2000, ‘Defining segments
and phases of a time capnogram’, Anesth. Analg., vol.
91, no. 4, pp. 973-977.
Dias, F, Alves, J, Januário, F, Ferreira, JL & Vassilenko, V
2013, ‘Prototype and Graphical Interface for Selective
Exhaled Air Acquisition’, Proc. of the Intern. Conf. on
Biomedical Electronics and Devices, vol. 1, pp. 216-
219.
Roussos, C & Zakynthinos, S 1996, ‘Fatigue of the
respiratory muscles’, Intensive Care Med., vol. 154, pp.
1099-1105.
Capnia, Inc. 2015, ‘Selection, segmentation and analysis of
exhaled breath for airway disorders assessment’,
WO2015143384 A1.
BIODEVICES 2017 - 10th International Conference on Biomedical Electronics and Devices
170
