
ICT and Ageing in Lebanese Public Hospitals
A Resource based View Perspective on Capabilities
Nabil Georges Badr
1
, Charbel Chedrawi
2
and Jamil Arida
2
1
Grenoble Graduate School of Business, Grenoble, France
2
Universite Saint Joseph, Beirut, Lebanon
Keywords: ICT, Ageing, Lebanese Public Hospitals, Hospital Information System.
Abstract: This paper looks into the Lebanese healthcare system and its readiness to care for a growing elderly population
and how ICT is used and how it is perceived by the stakeholders. The paper presents concerns on ageing
population in Lebanon. It first addresses the status of hospital infrastructure in the country, and then discusses
some interviews regarding ICT plans with six general managers of large public hospitals in different regions
of Lebanon.
1 INTRODUCTION
Population ageing, which entails an increasing share
of older persons in the population, is a major global
demographic trend; a trend that is expected to
intensify during the twenty-first century, driven by
remarkable increases in life expectancy and falling
fertility rates. By 2050, old people will outnumber
children on earth (ESA, 2012).
This paper’s setting is the country of Lebanon, a
small middle-income developing country with a
population estimated at around four million,
characterized by unique socio-demographic features
that render the ageing of its population a complex
challenge (Saxena, 2008). A rapidly ageing society of
adults of 65+ years faced by the lack of clear
comprehensive government policy, the unavailability
of accurate comprehensive database and statistics,
limited capabilities of existing institutions
complicated by an increased pressure on a resources
deficient healthcare system (Sibai, 2014). Findings
from the Lebanese National Health Expenditures and
Utilization Survey (Ammar, 2009), indicate that,
while older adults constitute less than 10 % of the
population, they consume over 60 % of the health
care resources.
Key questions arise: Are Lebanese Public
Hospitals ready to face the demands from an ageing
population? What role could ICT have in this shift?
In an attempt to answer these questions, the paper
surveys a selection of 6 geographically distributed
Lebanese public hospitals serving a mixed
demography of patients in order to learn how these
hospitals face the demands of an ageing population
and identify the role of ICT implementations in
addressing this challenge. Grounded in the principles
of Resource-Based View theory (RBV), the paper is
organized as follows: First, an overview on the
relevant literature with respect to ICT
implementations for ageing societies. Followed by a
look into obstacles faced in developing countries with
a focus on the Lebanese healthcare system and related
ICT implementations. After the literature review a
section presents the methodology used in this
research. Then the paper is concluded with the
discussion and suggestions for further research.
2 BACKGROUND
Similar to the work of Bryson et al. (2007),
Rosenberg and Ferlie (2014), and Burton and Malone
(2014), this paper uses RBV theory as a springboard
in assessing the performance of Lebanese hospitals
towards caring for the aging population. A RBV
theoretical lens could shed light on the preparedness
and capability of Lebanese hospitals to deploy
internal resources in order to improve their
performance, under severe financing pressure.
Therefore, the RBV setting in this context does not
assume the existence of competitive market forces but
can be a useful assessment of the strategic potential
Badr N., Chedrawi C. and Arida J.
ICT and Ageing in Lebanese Public Hospitals - A Resource based View Perspective on Capabilities.
DOI: 10.5220/0006096102050212
In Proceedings of the 10th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2017), pages 205-212
ISBN: 978-989-758-213-4
Copyright
c
2017 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
205

of Lebanese public hospital organizations.
Furthermore, rather than financial performance,
healthcare capabilities towards the aging are
considered.
Literature on RBV links firm capability and
performance to its ability to use its tangible and
intangible resources (Eisenhardt and Martin, 2000).
Originally developed in private sector firms
(Wernerfelt, 1984), RBV theory argues that firms
with different resource profiles and capabilities
exhibit different performance levels. Thus, the
effective use of these resources yields ‘core
competences’. Core competences are key internal
resources, which, when effectively developed and
exploited into dynamic capabilities (Teece et al,
1997), allow organizations to perform. These
resources in healthcare could be human, such as
nursing staff for example, financial and infrastructure
such as number of beds, etc. and information
technology. Further, the “level of resource
constraint” in a public hospital setting may mimic
“market volatility” in the private sector.
2.1 ICT for Health in an Ageing
Society
New advances in technology make it possible to
integrate previously disparate facility systems to form
an “intelligent” hospital infrastructure (Blumenthal
and Glaser, 2007). A plethora of applications
generically referred to as ‘telemedicine’ (e.g. video
chat, mobile devices, and internet connected medical
monitors) is expected to extend the provider - patient
relationship boundary to remote areas positively
impacting healthcare for the ageing in developing
countries (Lucas, 2008). Assistive technologies have
been proposed to overcome elderly problems such as
fall risk, chronic disease, dementia, social isolation,
and poor medication management, etc. ICT is one of
these technologies along with robotics and
gamification (Khosravi and Ghapanchi, 2015).
In general, there is evidence of benefit to society
healthcare and patient care from access to
Information and Communication Technologies (ICT)
infrastructure, such as communication and systems
for data interchange (Anwar et al, 2011), or online
health information tools (Bolle, et al, 2015) with a
keen emphasis on integrated care for the ageing
(Merino et al, 2015). Progress in the field of health
information systems is rather directly correlated with
more quality and efficiency of care, where ‘‘with
more efficiency of care’’ may in future mean that care
will remain affordable (Haux, 2006). Patient access to
electronic medical records improved patient
communication (Cimino et al, 2002), however might
have impacted aspects of physician - patient
communication (Makoul et al, 2001). Poissant et al
(2005) found that the use of bedside terminals and
central station desktops saved nurses around 25% of
their overall time spent documenting during a shift.
That was encouraging. However, the authors found
conflicting evidence supporting undesirable
outcomes: bedside or point-of-care systems increased
documentation time of physicians by 17.5%. Early
empirical data on cost reductions was not very
consistent (Hillestad, et al, 2005). This could have
been be due to the variability of the health IT systems
in their features and implementations (Chaudhry, et
al, 2006). Later on, as technology advances were
introduced, the benefits of computerized physician
order entry systems CPOE were reported (Khajouei
et al, 2011). More recent studies show measurable
benefits emerging from the adoption of health
information technology; these benefits range from
efficiency and effectiveness of care (McCarthy,
2009), provider and patient satisfaction, preventive
care for chronic diseases (Wildevuur and Simonse,
2015) and patient safety (Buntin et al, 2011)
especially in developing countries where health
resources are scarce (Marful et al, 2015).
2.2 Obstacles to Public Healthcare ICT
in Developing Countries
Since the turn of the century, public authorities have
been encouraging healthcare organizations to adopt
new techniques and systems in order to deliver
services of high quality and low cost (Naranjo-Gil,
2009), especially where adoption of innovations tends
to be slow and fragmented (Fagerberg et al., 2005). In
the public healthcare context, legislation and donor
support are fundamental to the rise of propensity and
ability to adopt ICT into Healthcare even in its basic
capacities (Oak, 2007). In developing countries,
studies underscore the possibility of impact on the
cost of care as hindering the adoption of ICT into
healthcare practice (Panir, 2011), extending beyond
initial implementation over the full life-cycle of
operating and maintaining these systems (Cohen et al,
2015). Cost of acquisition and maintenance and the
lack of ICT skills have been known to present a
significant barrier to implementation of ICT into
hospitals of developing countries. Lack of skilled
resources (Bing-Jonsson, et al, 2015) and the
deficiency in ICT infrastructure hinder the
capabilities of developing countries to acquire and
develop electronic medical records for instance
(Anwar et al, 2011). Physicians may perceive a loss
HEALTHINF 2017 - 10th International Conference on Health Informatics
206

of professional autonomy (Esmaeilzadeh et al., 2015)
and English literacy and education levels could curb
the intention to use (Hasanain et al., 2015). The
increasing familiarity of a new generations of
healthcare practitioners is likely to lessen adoption
issues (Hennington and Janz, 2007). Thus,
organizational barriers to ICT adoption in healthcare
have been recognized in the form of structure,
policies, incentives and decision processes (Lluch,
2011).
2.3 Ageing and the Lebanese
Healthcare System
Research on ageing in Lebanon involves three
themes: living arrangements, social relations, and
health (Abdulrahim et al, 2015). Ageing was related
to health in terms of practices and social statuses that
encourage good health (Ajrouch et al. 2013), nutrition
(Boulos et al, 2014), and discussing threats to good
health such as chronic conditions (Waked et al, 2011),
even the role of religion (Chaaya et al, 2007). Yet, the
literature is scarce when it comes to discussing the
contribution of hospitals to the well-being of the
elderly in Lebanon. The Lebanese healthcare system
is described by a wide network of public (28) and
private (136) hospitals and counts 26 beds per 1000
population making this one of the highest ratios in the
Middle East; however, only 17% of these hospitals
and 16.6% of the beds are in the public sector. There
are few geriatricians practicing in the country; few
hospitals and health centers, both private and public,
have geriatric units. In 2011 the Ministry of Public
Health (MOPH) report (Table 1) shows that there
were 377,470 of elderly individuals in Lebanon, 65%
of them aged between 65 and 74. The number of
hospitals and the number of beds don’t reflect the
effective need (6 hospitals and 470 beds in Mount
Lebanon for 145,558 elder versus 5 Hospitals and 365
beds in Nabatieh for 26,033 elderly). Hospitalization
rates (days per year spent at hospitals) among older
people exceed 28 % which is almost two-fold the
national average (Kronfol, 2006). Older persons in
Lebanon continue to rely on their relatives for
healthcare. The transition from large extended
families to small nuclear ones, accompanied with
high rates of emigration among young Lebanese, an
increased entry of women into the labor force have
created a relative shortage in family members
available for the provision of care (Sibai and Kronfol
2011). Concerns are growing about providing the
elderly with a better quality of life (Silbermann et al.,
2015).
2.4 Development of ICT in Lebanese
Hospitals
In the Lebanon, the ICT sector witnessed significant
growth over the period stretching from 2009 to 2014,
growing by an average annual rate of 7.9% to reach a
market size of USD 381 million in 2014 (MOPH).
Though Lebanon has the required capacity,
innovation, and skills required to improve its ICT
sector, the country’s lack of adequate infrastructure
and regulations have so far slowed the development
of ICT in hospitals. Furthermore, budgetary
constraints and the lack of ICT competence in
physicians present a challenge in rolling out ICT
applications and services (Nicolian et al, 2015). Thus,
ICT empirical research in Lebanese hospitals is
limited and health data statistics present a daunting
task in a fragmented health information system.
Studies treating the use of technology tackled the
effect of total quality management implementation on
innovation skills of hospital staff (Aoun and Hasnan,
2015). Extant studies range from the discussion about
Healthcare IS for data mining (Shahin et al, 2014) to
a review job satisfaction of nurses is related to the
level of information system use in their work
(Maamari and Chaanine, 2013). Little research has
focused directly on ICT in the care of the aging.
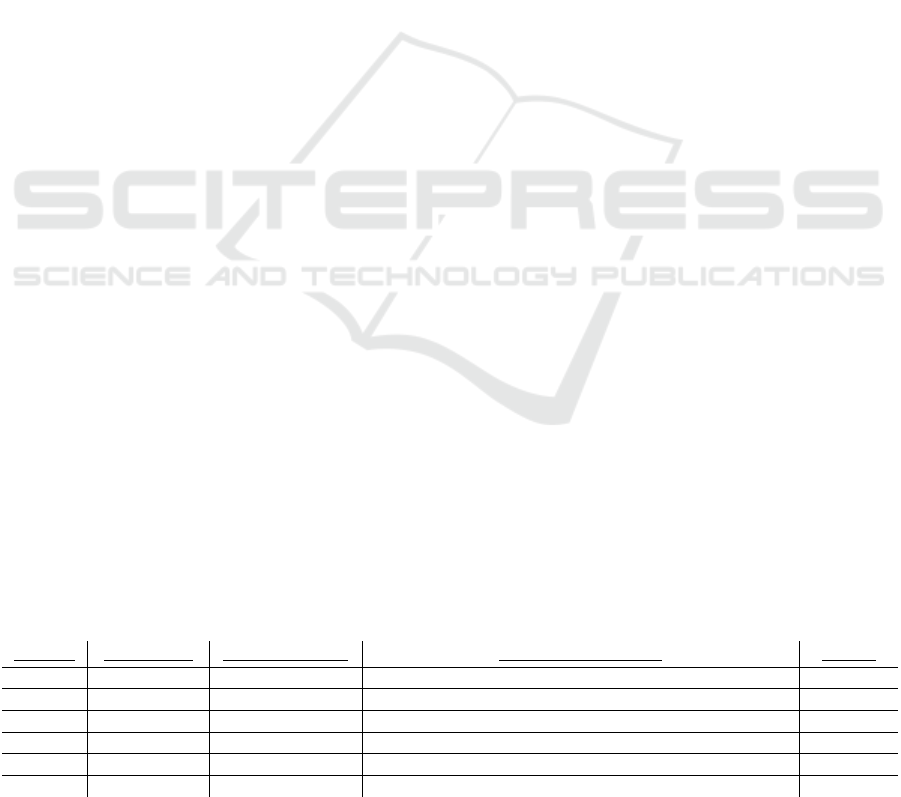
Table 1: Public hospitals capacity overview in relationship with the elderly in each region. Source: CAS, 2007 (The National
Survey of Household Living Conditions), and MOPH 2011.
Region Beirut Bekaa
Mount
Lebanon
Nabatieh
North
Lebanon
South
Lebanon
Total
Number of public
hospitals
2 5 6 5 7 3 28
Number of beds
in public Hospitals
595 430 470 365 455 235 2,550
Elderly population (% of
population in region)
36,156
(10%)
50,311
(13%)
145,558
(39%)
26,033 (7
%)
77,281
(21%)
42,131
(11%)
377,4
70
ICT and Ageing in Lebanese Public Hospitals - A Resource based View Perspective on Capabilities
207
3 METHODOLOGY
Our research employed a qualitative methodology in
an exploratory approach (Eisenhardt, 1989). Data
were collected by means of semi-structured
interviews conducted between May 2015 and May
2016. In this study we interviewed general managers
of six public hospitals, in six different regions in
Lebanon covering a cross section of the Lebanese
demography. Largest ranked by number of beds (by
MOPH, 2011), these hospitals have stated that they
have implemented or are in the process of
implementing components of a Hospital Information
System (HIS) as part of their ICT strategy. HIS
provides the underpinnings for health-related
decision-making that affect health outcomes of the
ageing (mortality, morbidity, disease outbreaks,
health status, disability, wellbeing). These hospitals
were coded (H1…H6) to maintain the desired
anonymity of the participants. Data consolidation was
carried out by means of the software N*VIVO.
Secondary data from documentation provided by the
hospitals showed (1) occupancy ratios and capacity;
(2) nursing staff information; (3) financing and
government support information; and (4)
infrastructure details mapped to the stages of the
electronic medical record adoption model suggested
by the Healthcare Information and Management
Systems Society (HIMMS).
4 DISCUSSION
4.1 Are Lebanese Public Hospitals
Ready to Face the Needs of an
Aging Population?
The study shows that the most likely answer is “No”
(Table 2). Major challenges were reported by the
informants in this study; mainly high occupancy
ratios and low capacity in terms of number of beds,
short-staffing on nurses, lack of adequate
infrastructure due to a reliance on self-financing, and
little government support.
(1) Hospitals reported challenges of high
occupancy ratios and low capacity in terms of number
of beds; “The hospital has 167 beds and still we face
a daily problem. Sometimes occupancy is above 90%
and the hospital cannot respond to the patients’ needs
as they sit in the emergency waiting (H6)”.
(2) The number of nurses is a major concern for
all the hospitals in this study, as they agreed that they
were adequately staffed by physicians and
understaffed on nurses. This issue is well summarized
by the informant of Hospital 4: “The number of nurses
is a major problem […] but the number of doctors is
adequate. The hospital performs 2000 surgeries
yearly and 70% of these patients are aged more than
65 years”
(3) The hospitals interviewed are still waiting for
the Ministry of Health to define a strategy for quality
health care. The General Manager of H6 explains:
“The government finances each hospital for its
expenses in proportion to the number of beds with a
plus related to the hospital needs. Public hospitals
cannot reject patients even if the hospital cost exceeds
the amount given by the government. The ministry of
health gives our hospital 6 billion Lebanese pounds
yearly (4 Million USD). This number is small if we
compare it to the needs of care for 167 beds. This
places a stress on our operating capability (H6)”.
(4) All hospitals concurred on the lack of
infrastructure to support the growth in demand and
conveyed that most of their operational budgets is
self-funded or financed through donations. “The
hospital upgrades its infrastructure from its own
budget”(H2) and the expansion plans are covered by
auto financing” (H3, H4, H5, H6)“Otherwise, most
of the expansions financing sources in all the public
hospitals in Lebanon come from donations and
contributions from Kuwait, Islamic Banks, Emirates
and Qatar (H1). This confirms the work of Saxena
(2008) and Sibai (2014).
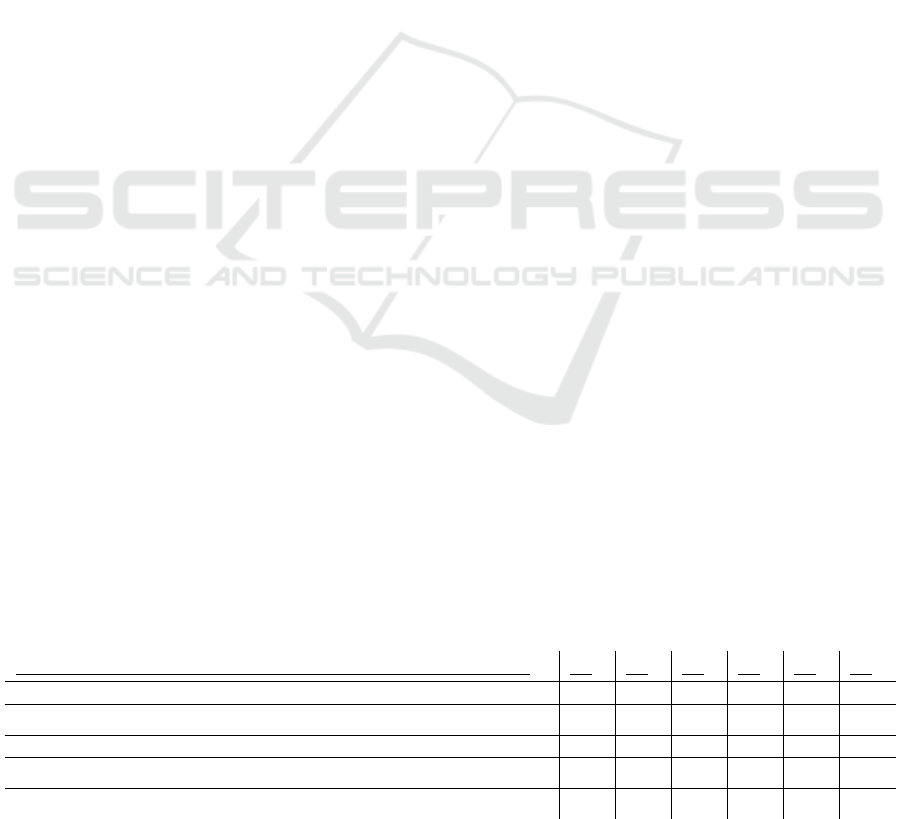
Table 2: Summary of empirical data (last column indicates hospital’s stated readiness to face the needs of an aging
population).
Hospital
Patients 65+ Occupancy ratios Major ailments treated Ready?
H1 50 % 90 + % Heart failure Yes
H2 55 % 85 + % Heart failure, chronic disease (Diabetes, etc.) No
H3 70 % 90 + % Heart failure and obesity No
H4 65 % 80 + % Heart failure Yes
H5 70 % 80 + % Heart failure No
H6 50 % 90 + % Prostate issues, broken hips, obesity, chronic diseases No
HEALTHINF 2017 - 10th International Conference on Health Informatics
208
4.2 ICT’s Role in the Enablement of
Care for the Ageing
The general manager of H6 gives a pertinent
summary on the perceived role of ICT in Lebanese
Public hospitals: “Today there is a greater need than
ever to leverage technology to improve health, quality
of life, and social connectivity for older adults, and
assist in clinical care and monitoring of more
impaired older adults. A variety of technology
solutions (such as Web-based applications, remote
sensing technologies, electronic health records and
other devices) support patient engagement. The
impact of ICT is indirect and is contingent on the
redesign of practices and structures also outside
health care. Improvements will only be realized if all
parties involved can coordinate their efforts to take
advantage of new technology.”
Elderly care is demanding, hospitals must have
the resources to act quickly and effectively with a
solid decision support system in order to minimize
errors and offer quality of care for the elderly (Smith
et al, 2006). In addition to a trained and experienced
staff in the needs of the ageing, “a solid database to
follow up each case is required in order to find the
appropriate solution” (H2). The GM of H4 indicated
that they have installed “24/7 monitoring systems of
health and activities, intelligent devices and
appliances, internet enabled services, predictive
behaviour models, and so on” in order to provide a
better quality of care for their elderly patients”. Such
innovations in stationary and mobile solutions would
allow practitioners to stay in continuous contact,
whether at the patient’s bedside, in examination
rooms, or in emergency treatment centers, to
effectively develop and deliver patient assessments,
and make more informed care decisions based on
collaborative treatment plans. This findings aligns
with the works of Lucas (2008) and Anwar et al.
(2011).
It is expected that such ICT technologies would
(1) Reduce the time of treatments (H1); (2) provide
better access to data for enhanced decision making,
preventive care and disease management (H1, H2,
H3, H4, & H5); and (3) improve interdepartmental
collaboration / Emergency services (H6).
For all 6 hospitals surveyed, the adoption of the
information system is of top importance. “The
adoption of the information system is prominent
practice for today’s hospital, in the use of equipment,
archive, and for more efficient medical results” states
the GM of H1 at the first stages of the interview. All
hospitals have described their adoption of the Health
IS system in advanced stage (Table 3). This is quite
an achievement considering that all these public
hospitals stated that they rely on self-funded
initiatives. Nurses and doctors document patient’s
vital signs in the system, physician prescription
history are tracked by the system, and PACS systems
are connected to the online medical history. (PACS is
the acronym for picture archive and communication
system, a computer network for digitized radiologic
images and reports).
Ultimately, addressing medical research
advancement benefits, the GM of H1 stressed that
“better access to data that can be studied and help to
get better solutions to face the ageing society”. ICT
has become necessary to manage routine function up
close, and monitor vital signs measurements and
control the administration and recording of
medications (type, dose & time). Agreeing, three
other hospitals (H3, H4, H5) pointed out that “ICT in
the form of an integrated information database aims
at disease management to help improve the
awareness and preventive care in the elderly patient
population”. Furthermore, the case summaries
emphasized the role of the hospital senior
management in encouraging adoption. “It was my
responsibility to oversee the implementation of the
new system and to follow it up step by step with the
different actors in order to achieve the results
needed.” Adds the GM of H3.
The Lebanese government did not engage with
any of the 6 hospitals in the decision to adopt their
HIS, such decision was taken by the board of
directors of each hospital independently.
Table 3: Level of HIS use in the hospital (Y= in use at the moment; Y*=Incomplete, but in process).
Level of Use (based on the HIMMS Model for EMR adoption maturity)
H1 H2 H3 H4 H5 H6
Nurses / doctors enter patient’s vital signs in the system Y Y Y Y Y Y
Physician prescription history tracked by the system Y Y Y Y* Y Y
PACS systems connected to online medical history Y Y* Y Y Y Y
Online medical history Y Y Y* Y Y Y
Automated pharmacy, laboratory, and radiology Y* Y Y Y* Y Y*
ICT and Ageing in Lebanese Public Hospitals - A Resource based View Perspective on Capabilities
209

Three of the hospital surveyed (H6, H3 and H1)
expressed a relatively low barrier to adoption: The
general manager of H6 disclosed that for the
relatively new hospital, HIS was part of the hospital
build out plans. Likewise, H3 pride themselves with
a continual development effort of the HIS: “We had
an integrated information system since the start […]
we develop it continuously based on the growing and
changing needs of the hospital”, affirms the GM. In
the case of H1, their GM shared that “there were no
obstacles in the implementation because all the staff
started using the system since the establishment of the
hospital. No transition was required since the staff
was recruited with an IT IS experience. […] When we
developed the implementation plan, we defined the
different roles of the major actors. I was following
each step to make sure that the plan is well executed.
This was time consuming but effective”. In contrast
the HIS in H5 is older and with limited with disparate
data stores that are not integrated. Obstacles such as
the qualification of the existing staff and the difficulty
of recruiting new talent into the public sector were
indicated. Additionally, budgets that need to be
approved by governmental authorities have not yet
been allocated to this hospital for the refresh of their
system. Budgetary concerns were raised by most
hospitals (H2, H3, H4, and H5), “The process was
time and energy consuming” (H3). “Significant
efforts and investments in time and expertise were
needed” (H6). However, the “novelty of technologies
used posed a reluctance in the staff to embrace new
technologies, with little evidence that this technology
will indeed be useful” (H6).
In H4, the GM reports an irregular focus on the
Information System build out. The lack of IT/IS
knowledge among the practicing staff presented
significant challenges. To encourage adoption and
assimilation, training and awareness sessions were
necessary to highlight the importance of the
implementation for the wellbeing of the patients.
Resistance to adoption was at different levels in
each hospital; at some, the senior staff was non
cooperative at the start (H2 & H5) and for others
healthcare personnel’s attitude towards new
technology was not always positive (H1, H6, H4).
Used to their traditional pen and ink methods, they
were slow to assimilate the benefits of ICT usage for
patient care (H6). The cooperation among project
implementation teams and between IT teams and the
hospital’s staff at all levels was a key issue in order to
reduce this resistance (H2).
5 CONCLUSIONS
Lebanese public hospitals are short of capable to face
the needs of an ageing population. This work has
achieved two objectives to help answer the research
question:
First, the use of RBV theory as a backdrop for this
study has underlined major challenges facing public
hospitals in their ability to use their resources to care
for an aging population. Informants have reported
resource constraints and limitations of multiple
dimensions, namely (1) high occupancy ratios and a
low capacity in terms of number of beds, (2) short-
staffed on nurses, (3) lack of adequate infrastructure
due to a reliance on self-financing, and (4) little
government support. Hospitals in the study
communicated occupancy ratios between 80% and
90%. Most of their patients are above 65 years of age
(reaching 65%). Major ailments treated are heart
failures, chronic disease (obesity, diabetes, blood
sugar, nervous system etc.) that require close
supervision and long residency periods. With this
burden, all hospitals express a lack of adequate
infrastructure and a relatively low capacity to handle
patients (number of beds); they are short-staffed on
nurses and face higher cost with little financing
support from the government. In spite of this self-
funded effort, most of these hospitals recognize the
value of an integrated information system in lowering
their costs and increasing their capabilities to deliver
quality elderly care.
Second, this paper extends the body of knowledge
of healthcare ICT in the country of Lebanon to
provide an account of ICT use in healthcare for the
ageing in public hospitals in settings where uses of
ICT could contribute to the effectiveness of Lebanese
public hospitals to provide quality care for an aging
population.
5.1 ICT as a Dynamic Capability in
Lebanese Public Hospitals
The informants of this study reported use of ICT to
care for the aging to have four significant benefits: (1)
Provide better access to data for an enhanced decision
making for treatment and medication; (2) potentially
reduce the time of treatments; (3) improve the
practice of preventive care, disease management and
promote wellbeing; and (4) improve the resource
allocation for better quality care. However, such
benefits were recognized to impose a significant
investment on hospitals. Investments that await
governmental or donor funding support must be
supplemented by commitment from senior
HEALTHINF 2017 - 10th International Conference on Health Informatics
210

management, continual development plans, and a
collaborative approach between all hospital staff to
raise the awareness on the benefits of ICT usage for
elderly patient care.
5.2 Research Limitation
This research presents a methodological limit that
may open up new avenues of future research. One of
the limitations of the study that worth mentioning is
that it relies on information provided by general
managers, thus potentially limiting the credibility of
information. The opportunity to expand the
interviews to IT managers of the hospitals would
provide deeper insights. Further, we are aware that
the results presented in this research depend strongly
on the context of the country. Their generalization
thus requires a certain reserve. Further research must
be done to advance the results of this study possibly
through action research potentially exploiting
principals of organizational development. This
approach could deepen the understanding on how
hospitals are transforming their healthcare practices
to improve their capacity for solving problems and
managing the challenges of care for the aging.
REFERENCES
Abdulrahim, S. Ajrouch. K., Antonucci, T., 2015 Aging in
Lebanon: Challenges and Opportunities. The
Gerontologist doi:10.1093/geront/gnu095.
Adler-Milstein J, Salzberg C, Franz C, Orav EJ, Newhouse
JP, Bates DW , 2013 Ann. Intern. Med.159:97–104.].
Ajrouch, K. J., Yount, K., Sibai, A. M., Roman, P., 2013. A
gendered perspective on well-being in later life:
Algeria, Lebanon, and Palestine. In S. McDaniel, and
Z. Zimmer, Eds., Global Ageing in the 21st Century,
pp.49–77. Surrey, UK: Ashgate Publishing.
Ammar, W., 2009. Health beyond Politics. WHO and
Ministry of Public Health in Lebanon.
Anwar, F., Shamim, A., Khan, S., 2011. Barriers in
adoption of health information technology in
developing societies. Int J Adv Comput Sci Appl, 2, 8.
Aoun, M., and Hasnan, N., 2015. Health-care technology
management: developing the innovation skills through
implementing soft TQM among Lebanese hospitals.
Total Quality Management and Business Excellence,
ahead-of-print, 1-11.
Bing-Jonsson, P. C., Foss, C., Bjørk, I. T., 2015. The
competence gap in community care: Imbalance
between expected and actual nursing staff competence.
Nordic Journal of Nursing Research,
0107408315601814.
Blumenthal D. and Glaser J., 2007. Information
Technology Comes to Medicine", NEJM Vol. 356,
24th, June 2007.
Bolle, S., van Weert, J. C., Daams, J. G., Loos, E. F., De
Haes, H. C., Smets, E. M., 2015. Online Health
Information Tool Effectiveness for Older Patients: A
Systematic Review of the Literature. Journal of Health
Communication, 20, 9, 1067-1083.
Boulos, C., Salameh, P., Barberger-Gateau, P., 2014.
Factors associated with poor nutritional status among
community dwelling Lebanese elderly subjects living
in rural areas: results of the AMEL study. The Journal
of Nutrition, Health and Aging, 18, 487–494.
Bryson J, Ackermann F, Eden C. Putting The Resource
Based View of Strategy and Distinctive Competencies
To Work in Public Organizations. Public Adm Rev.
2007; 67:702–17.
Buntin M. B., Burke, M. F., Hoaglin M. C. Blumenthal D.,
2011. The Benefits Of Health Information Technology:
A Review Of The Recent Literature Shows
Predominantly Positive Results. Health Affairs, 30,
no.3, 2011:464-471.
Burton CR, Rycroft-Malone J., 2014 Resource based view
of the firm as a theoretical lens on the organisational
consequences of quality improvement. Int J Health
Policy Manag. 2014; 3:113–5.
Chaaya, M., Sibai, A. M., Fayad, R., El-Roueiheb, Z., 2007.
Religiosity and depression in older people: Evidence
from underprivileged refugee and non-refugee
communities in Lebanon. Aging and Mental Health, 11,
37–44.
Cimino, J. J., Patel, V. L., & Kushniruk, A. W. (2002). The
patient clinical information system (PatCIS): technical
solutions for and experience with giving patients access
to their electronic medical records. Int J Med Inform,
68(1), 113-127.
Cohen, J. F., Coleman, E., Abrahams, L., 2015. Use and
Impacts of E-health Within Community Health
Facilities in Developing Countries: A Systematic
Literature Review. AISeL. ECIS 2015 Completed
Research Papers ECIS 2015 Proceedings.
Eisenhardt K.M., 1989, Building theories from case study
research, AOM review, Vol 14, N 4, pp. 532-550.
Eisenhardt, K. M. and Martin, J. A., 2000, Dynamic
capabilities: what are they? Strat. Mgmt. J., 21: 1105–
1121.
ESA, 2012 Population Division of the Department of
Economic and Social Affairs of the United Nations
Secretariat. World Population Prospects: The 2010,
2012 Revision.
Esmaeilzadeh, P., Sambasivan, M., Kumar, N., Nezakati,
H., 2015. Adoption of clinical decision support systems
in a developing country: Antecedents and outcomes of
physician's threat to perceived professional autonomy.
Int J Med Inform.
Fagerberg J., D.C. Mowery, R.R. Nelson, 2005, “Systems
of innovation: Perspectives and challenges” Oxford
handbook of innovation, Oxford University Press.
Hasanain, R. A., Vallmuur, K., Clark, M., 2015. Electronic
Medical Record Systems in Saudi Arabia: Knowledge
and Preferences of Healthcare Professionals. Journal of
Health Informatics in Developing Countries, 9, 1.
ICT and Ageing in Lebanese Public Hospitals - A Resource based View Perspective on Capabilities
211

Haux, R., Health information systems, past, present, future.
Int J Med Inform, 2006, 75, 268—281.
Hennington, A. and Janz, B. D., 2007 "Information Systems
and Healthcare XVI: Physician Adoption of Electronic
Medical Records: Applying the UTAUT Model in a
Healthcare Context," Comm. of the AIS: Vol. 19, 5.
Hillestad, R. et al, 2005 Health Information Technology:
Can HIT Lower Costs and Improve Quality? Santa
Monica, CA: RAND Corporation, 2005.
HIMSS EMR Adoption Model - HIMSS Analytics.
Khajouei, R., Wierenga, P. C., Hasman, A., & Jaspers, M.
W. (2011). Clinicians satisfaction with CPOE ease of
use and effect on clinicians' workflow, efficiency and
medication safety. Int J Med Inform, 80(5), 297-309.
Khosravi, P., and Ghapanchi, A. H., 2015. Investigating the
effectiveness of technologies applied to assist seniors:
A systematic literature review. Int J Med Inform.
Kronfol, N., 2006, “Rebuilding of the Lebanese health care
system: health sector reforms”, Eastern Mediterranean
Healh Journal, vol 12, pp 459-73.
Lluch, M., 2011. Healthcare professionals’ organisational
barriers to health information technologies. A literature
review. Int J Med Inform, 80, 12, 849-862.
Lucas, H., 2008. Information and communications
technology for future health systems in developing
countries. Social Science and Medicine, 66, 10, 2122-
2132.
Maamari, B., & Chaanine, J., 2013. Job satisfaction of the
modern information-system-using nurse in Lebanon.
Journal of Tech. Management in China, 8, 2, 120-136.
Makoul G, Curry RH, Tang PC. The use of electronic
medical records: communication patterns in outpatient
encounters. J Am Med Inform Assoc. 2001; 8, 6:610-5.
Marful, W. A., and Winter, A., 2015. When Information
Technology meets Healthcare in West Africa: A
Literature Review. Journal of Health Informatics in
Africa, 2, 2.
McCarthy, G. (2009). Deliver tangible ROI. Three
healthcare organizations see reduced costs, enhanced
efficiency and increased compliance with CPOE
systems. Health Manag Technol, 30(6), 26, 28-29.
Merino, M., Marqués, M., Egurbide, M., Romo, M.,
Rodríguez, I., García, M., de Manuel, E., 2015.
Deploying Integrated Care Models for Frail Elderly
Patients. International Journal of Integrated Care, 15, 5.
Mugdha R Oak, 2007. A review on barriers to
implementing health informatics in developing
countries, Journal of Health Informatics in developing
countries, vol 1, No. 1, 2007.
Naranjo-Gil, D., 2009. The influence of environmental and
organizational factors on innovation adoptions:
Consequences for performance in public sector
organizations. Technovation, 29, 12, 810-818.
Nicolian, N., Welch, C., Read, M., Roberts, M.,
Portsmouth, U. K., 2015. Critical organizational
challenges in delivering business value from IT: in
search of hybrid IT value models. Electronic Journal
Information Systems Evaluation Volume, 18, 2.
Panir, J.H., 2011 Role of ICTs in the Health Sector in
Developing Countries: A Critical Review of Literature.
February 15, 2011. Journal of Health Informatics in
Developing Countries.
Quivy R., Van Campenhoudt L., 1995, Manuel de
rechercheen sciences sociales, Dunod.
Qureshi, N. A., Kundi, G. M., Qureshi, Q. A., Akhtar, R.,
Hussain, L., 2015. An investigation Into the Adoption
and Use Issues of E-Health in Public Sector Hospitals
of Developing Countries. Mediterranean Journal of
Medical Sciences, 2, 1.
Rosenberg Hansen J, Ferlie E., 2014 Applying strategic
management theories in public sector organizations:
Developing a Typology. Public Management Review
2014. Sep17.
Saxena, P., 2008. Ageing and age-structural transition in the
Arab countries: Regional variations, socioeconomic
consequences and social security. Genus, 64, 37–74.
Shahin, A., Moudani, W., Chakik, F., Khalil, M., 2014,
April. Data mining in healthcare information systems:
Case studies in Northern Lebanon. In e-Technologies
and Networks for Development, ICeND, 2014 Third
International Conference on , pp. 151-155 . IEEE.
Sibai AM, Rizk A, Kronfol NM. , 2014. Ageing in the Arab
region: Trends, implications and policy options.
UNFPA, ESCWA, and CSA 2014.
Sibai, A. M., Yount, K. M., Tohme, R., Yamout, R.,
Kronfol, 2011: The older persons: from veneration to
Vulnerability? In S. Jabbour et al., eds Public health in
the Arab Word, Cambridge, Cambridge University
Press.
Silbermann, M., Fink, R. M., Min, S. J., Mancuso, M. P.,
Brant, J., Hajjar, R., Strode, D., 2015. Evaluating
palliative care needs in Middle Eastern countries.
Journal of palliative medicine, 18, 1, 18-25.
Chaudhry, B., Wang, J., Wu, S., Maglione, M., Mojica, W.,
Roth, E., Shekelle, P. G. (2006). Systematic review:
impact of health information technology on quality,
efficiency, and costs of medical care. Annals of internal
medicine, 144(10), 742-752.
Smith, D. H., Perrin, N., Feldstein, A., Yang, X., Kuang,
D., Simon, S. R., Soumerai, S. B., 2006. The impact of
prescribing safety alerts for elderly persons in an
electronic medical record: an interrupted time series
evaluation. Archives of Internal Medicine, 166, 10,
1098-1104.
Teece D, Pisano G, Shuen A., 1997 Dynamic Capabilities
and Strategic Management. Strategic Management
Journal. 1997; 18:509–33.
Waked, M., Khayat, G., Salameh, P., 2011. Chronic
obstructive pulmonary disease prevalence in Lebanon:
a cross-sectional descriptive study. Clinical
Epidemiology, 3, 1315–323.
Wernerfelt, B., 1984, A resource-based view of the firm.
Strategic Managements Journal, 5: 171–180.
Wildevuur, S. E., and Simonse, L. W., 2015. Information
and Communication Technology–Enabled Person-
Centered Care for the “Big Five” Chronic Conditions:
Scoping Review. Journal of medical Internet research,
17(3).
HEALTHINF 2017 - 10th International Conference on Health Informatics
212
