
Towards Providing Full Spectrum Antenatal Health Care in Low and
Middle Income Countries
Muhammad Abubakar
1
, Amina Bibi
1
, Rashad Hussain
1
, Zohra Bibi
1
, Asma Gul
2
, Zahid Bashir
3
,
Salman Noshear Arshad
4
, Momin Ayub Uppal
5
and Safee Ullah Chaudhary
1
1
Department of Biology, Lahore University of Management Sciences, DHA (Phase 5), Lahore, Pakistan
2
Gynaecology and Obstetrics Department, Shalamar Institute of Health Sciences, Lahore, Pakistan
3
Department of Forensic Medicine and Toxicology, Shalamar Institute of Health Sciences, Lahore, Pakistan
4
Department of Chemistry, Lahore University of Management Sciences, DHA (Phase 5), Lahore, Pakistan
5
Department of Electrical Engineering, Lahore University of Management Sciences, DHA (Phase 5), Lahore, Pakistan
Keywords: Antenatal Care, Mobile Health, Smartphone Health Monitoring, Decision Support Systems.
Abstract: The provision of Antenatal Care (ANC) for pregnant women plays a vital role in ensuring infant and maternal
health. Limited access to antenatal care in Low and Middle Income Countries (LMIC) results in high Infant
and Maternal Mortality Rate (IMR and MMR, respectively). In this work, we propose a cloud-based clinical
Decision Support System (DSS) integrated with a wearable health-sensor network for patient self-diagnosis
and real time health monitoring. Patient assessment is performed by evaluating the human-input coupled with
sensor-generated symptomatic information using a Bayesian network driven DSS. High risk pregnancies can
be identified and monitored along with dispensing of consultant advice directly to the patient. Patient and
disease incidence data is stored on the cloud for tuning probabilities of the Bayesian network towards
improving accuracy of predicting anomalies within the epidemiological context. The system therefore, aims
to control IMR and MMR by providing ubiquitous access to ANC in LMICs. A scaled-up implementation of
the proposed system can help reduce patient influx at the limited tertiary care centers by referring low-risk
cases to primary or secondary care establishments.
1 INTRODUCTION
Every year over 210 million pregnancy cases are
reported worldwide (Shah and Åhman, 2004). About
2.6 million of these pregnancies conclude in
stillbirths with 98% of these deaths occurring in Low
and Middle-Income Countries (LMIC) (Hogan et al.,
2010, WHO and UNICEF, 2012, UNICEF, 2012,
May 2014). Nearly 800 women lose their lives every
day as a result of pregnancy related complications
with 99% of all maternal deaths occurring in
developing countries. The high fertility rates amongst
LMIC women (Sathar et al., 1988) predisposes them
to an enhanced risk of pregnancy related
complications. The resource-limited health-care
infrastructures in the LMICs further aggravates the
situation, with women from remote poverty-stricken
areas being the most disadvantaged.
Antenatal care (ANC) has been proven to be a key
determinant of infant and maternal health (Inam and
Khan, 2002). Provision of the most basic ANC has
been shown to significantly reduce the astronomical
IMR and MMR in LMIC countries (Inam and Khan,
2002). A simple but timely measurement of high
blood pressure can help pre-empt several
complications including but not limited to
preeclampsia, ectopic or molar pregnancy, placenta
previa, placental abruption, miscarriage, hyperemesis
gravidarum, preterm labour as well as problems with
the foetus itself (Burrow et al., 2004, Norbeck and
Tilden, 1983, Sattar and Greer, 2002, U.S.
Department of Health and Human Services,
September 2010.). In Pakistan, like other LMICs, the
leading causes of maternal mortality include
haemorrhage, followed by eclampsia and sepsis
(Jafarey, 2002). Regularity in ANC can pre-empt
such obstetric and postnatal complications thereby
averting major emotional and financial stress for the
patients and their families.
The major impediments in provision of ANC in
478
Abubakar, M., Bibi, A., Hussain, R., Bibi, Z., Gul, A., Bashir, Z., Arshad, S., Uppal, M. and Chaudhary, S.
Towards Providing Full Spectrum Antenatal Health Care in Low and Middle Income Countries.
DOI: 10.5220/0005823104780483
In Proceedings of the 9th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2016) - Volume 5: HEALTHINF, pages 478-483
ISBN: 978-989-758-170-0
Copyright
c
2016 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

LMICs include poverty, illiteracy, inadequate
governmental healthcare support, obstacles in timely
access to available services and cultural barriers.
Moreover, with the absence of health insurance safety
nets in LMICs accessibility to ANC becomes directly
proportional to the economic status of the patient and
her family. Besides the non-availability of essential
health information, ill-equipped primary care centres
and under-trained primary health care workers also
contribute to the high IMRs and MMRs. (Penfold et
al., 2013, Bloom et al., 1999, Ransom et al., 2002,
Titaley et al., 2010). As a result, a large number of
patients in developing countries fail to access, obtain
and implement ANC, essential for the welfare of both
the foetus and the mother.
In this work, we propose a cloud-based ANC DSS
for an assistive medical diagnosis and monitoring of
pregnant women. The salient features of the system
include: (i) patient self-diagnostics; (ii) automated
monitoring; (iii) patient prioritization; (iv) real-time
case tracking and intervention by patient-opted
tertiary care consultants; and (v) on request consultant
advice dispensation. The structural components of
our clinical Decision Support System (DSS) include
a multilingual tablet and smart phone front-end
application that is usable by both patients and
consultants; a wearable health sensor suite interfaced
with front-ends via Bluetooth (Miller and Bisdikian,
2001); a web application for dealing with PC-based
patient requests; a desktop application for hospital
administration and a backend database server for
storing patient and doctor incidents data.
At the heart of the system is a DSS which is
compliant with the ANC guidelines devised by the
Merck® Manual Professional Version (Merck, 2015)
and is designed to emulate the decision making
capabilities of a professional medical advisor. A total
of 16 pregnancy-related abnormalities (Table 1) are
included and elaborated by Merck along with their
risk factors and symptoms. Pre-eclampsia has been
selected and a probabilistic Bayesian network
(Friedman et al., 1997) is constructed involving its
symptoms (Figure 1). Clinical data from Shalamar
Institute of Health Sciences (SIHS, Pakistan) is used
to calculate the probabilities in the network. Patients
may answer a series of systematically-posed
questions, developed in accordance with the Merck®
guidelines for self-diagnosis, in tandem with inputs
from patient-worn sensors. Sensor-based monitoring
can be performed in a continuous or periodic manner
depending on the type of health marker to be
measured. The probability of an abnormality is then
progressively calculated by employing the Bayesian
network and the patient provided symptomatic
information.
The system can thereby keep track of and assess
the health state of the respondent in real time
irrespective of her physical distance from a hospital.
Users can also choose to subscribe to certified
consultants who are registered in the system, based on
the tertiary hospital that they’re working in. These
consultants may then choose to participate and
receive the patient’s data followed by intercession in
the recommendations dispensation process. On the
basis of the diagnostic information, a health support
or emergency response may be orchestrated at the
primary, secondary or tertiary care centres. The
system is currently being deployed at SIHS, where it
is undergoing functional testing.
Taken together, the proposed system ensures a
timely provision of optimal quality ANC to LMIC
populace; thus, providing significant assistance in
reducing the IMR and MMR.
Table 1: List of pregnancy disorders enlisted in the Merck®
ANC guidelines.
1 Oligohydramnios 9 Abruptio Placentae
2 Preeclampsia and
Eclampsia
10 Cervical
Insufficiency
3 Spontaneous
Abortion
11 Intra-Amniotic
Infection
4 Pruritic Urticarial
Papules & Plaques of
Pregnancy
12 Hyperemesis
Gravidarum
5 Pemphigoid
Gestationis
13 Erythroblastosis
Fetalis
6 Septic Abortion 14 Placenta Previa
7 Stillbirth 15 Ectopic Pregnancy
8 Vasa Previa 16 Polyhydramnios
2 RESULTS
2.1 Elicitation of Risk Factors,
Symptoms and Diseases from
Merck® ANC Guidelines
The comprehensive ANC guidelines provided in the
Merck® Manual Professional Version were used to
elicit pregnancy-related abnormalities, the risk factor
to which a patient may be predisposed and the
presented disease symptoms. A total of 16
abnormalities (Table 1) were extracted along with
respective risk factors and symptoms. These included
pre-eclampsia (MacKay et al., 2001) which is
amongst the leading contributors to IMR (Basso et al.,
2006) and MMR (Ghulmiyyah and Sibai, 2012). A
Towards Providing Full Spectrum Antenatal Health Care in Low and Middle Income Countries
479

Table 2: Symptoms and Risk Factors Associated with
Preeclampsia and Eclampsia.
S
y
mptoms and si
g
ns Risk factors
Proteinuria Nulliparity
High blood pressure
and hypertension
Pre-existing
chronic hypertension
Severe headache Vascular disorders
Visual disturbances
(blurred vision, scotomata)
Pre-existing or
gestational diabetes
Coagulopathy (Petechiae) Age>35 or Age<17
Non-dependent oedema
(facial & hand swelling)
Family history of
preeclampsia
Hepatic ischemia
(right upper quadrant
abdominal, epigastric pain)
Preeclampsia or poor
outcome in previous
pregnancies
Enhanced reflex reactivity Multifetal pregnancy
Nausea Obesity
Confusion Thrombotic disorders
Vomiting
Dyspnea
Cyanosis
Stroke
Serum > two times normal
(AST, ALT)
Thrombocytopenia
Reduced urine output
detailed tabulation of 10 risk factors and 17
symptomatic presentations associated with pre-
eclampsia are provided in Table 2.
2.2 DSS for Pre-eclampsia using a
Bayesian Network
All symptoms of pre-eclampsia are orchestrated into
a Bayesian Network (Figure 1). Bayesian
probabilities for each disease outcome are
progressively calculated upon input of symptomatic
information by the user and wearable health sensors.
The probabilities in the Bayesian Network are
populated in line with the diagnosis pathways in the
Merck® Manual and will later be further tuned in
light of regionally localized patient data (both manual
and sensor inputs). The DSS encapsulates the
Bayesian probability calculation engine and
transforms user inputs into probable outcomes,
thereby also prioritizing high risk pregnancies for
evaluation by a remote clinical consultant. The output
to the user includes primary care advice and
recommendations while detailed user profile and
assessment information is uploaded to the cloud for
ready reference and intervention of the consultant.
2.3 System Architecture for
Cloud-based ANC
A three-tier architecture is employed to construct the
foundation of the proposed system (Figure 2). The
first tier comprises of Graphical User Interfaces
(GUI) for the targeted client audience. These GUIs
include a smart phone/tablet app and a web
application for patients, primary health professionals
and, consultants. A desktop application is also
provided for user administration by the hospital
administrators. Middle tier is a subscription-driven
Web API (Microsoft, 2014) which embodies the
functional logic including the DSS and Bayesian
network. The third tier includes a MySQL (MySQL,
2001) relational database server with a normalized
schema of all system entities. User triggered
operations and requests are transported in JSON
(Peng et al., 2011) between the wearable sensors, GUI
applications, the Web API and the database.
Microsoft® MVC (Masound and Halabi, 2006)
has been employed to develop the Web API. Agile
Development (Martin, 2003) methodology is used to
incrementally develop the system’s overall software
manifestation. The system has been tested and
verified using white-box testing at the component
level. Integration testing has been performed to
validate the functional coupling of the overall system.
2.4 Security and Privacy
Confidentiality of patient data is ensured by
controlled access and its on-demand availability from
isolated logical data storages at hospital level. It can
be further enhanced by continuous risk assessment
and updates to the security policies. Furthermore, we
are considering to deploy Health Level-7 (HL-7)
Healthcare Privacy and Security Classification
System (HCS), and Role-Based Access Control
Healthcare Permission Catalogue (RBAC). Towards
implementing data segmentation for access across
distributed systems, we are also considering to use
HL-7 Data Segmentation for Privacy (DS4P) as a
standard.
2.5 ANC System Software Prototype
2.5.1 Smartphone and Tablet Application
for Patients and Consultants
A smartphone application is developed for users
including patients, primary care operatives, doctors
HEALTHINF 2016 - 9th International Conference on Health Informatics
480
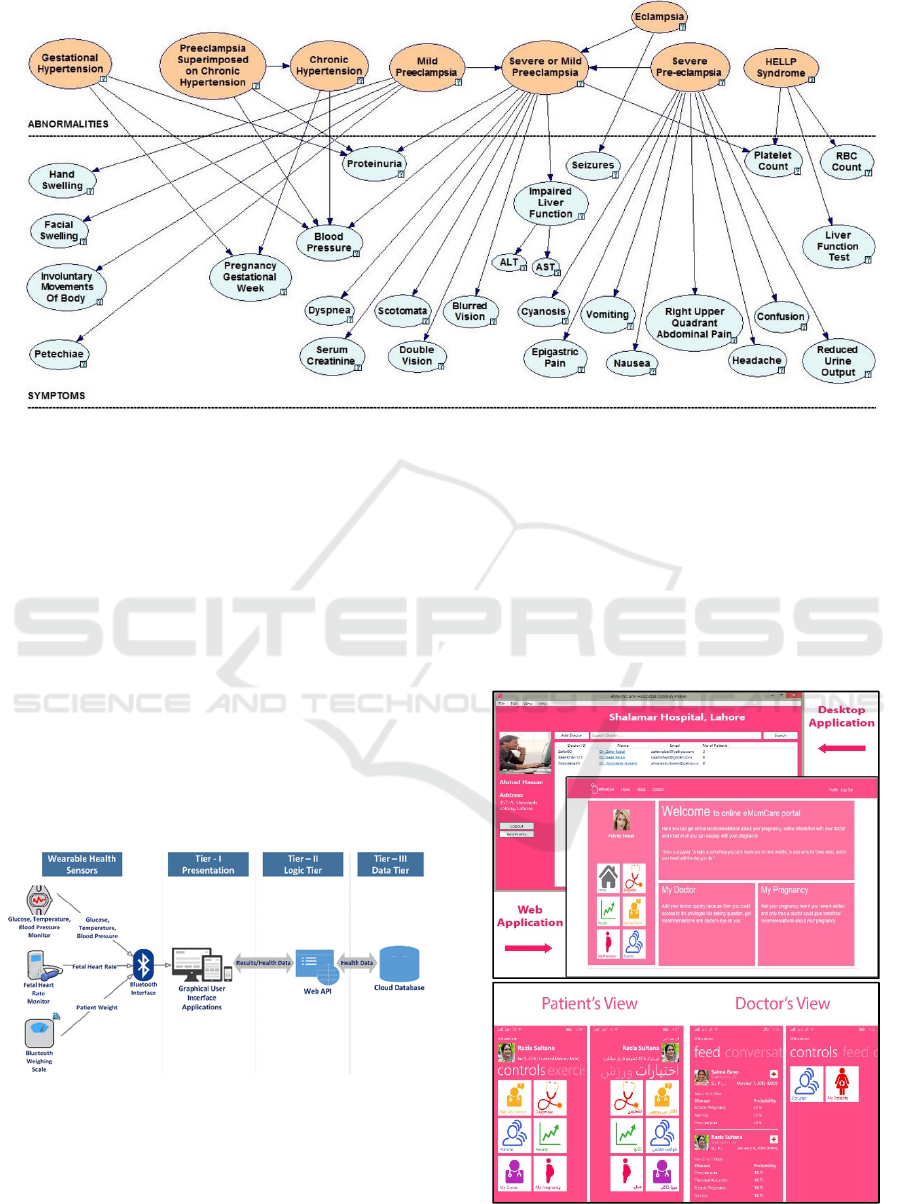
Figure 1: Bayesian Network of Symptoms Leading to Pre-eclampsia and Eclampsia.
and consultants (Figure 3B). Heuristic evaluation for
user interfaces has been undertaken and the smart
phone app has been localized to rural locales along
with a text-to-speech feature in the DSS.
Furthermore, elicitation of potential users’
characteristics such as reasoning ability, gender, age,
spatial memory and learning style is underway
towards creating an enabled user experience.
Windows Phone Development Kit (Microsoft, 2013)
is used to develop the application and XAML
(Schmidt, 2010) is used to construct the user
interfaces. The application encompasses features
such as user registration, profile creation, patient self-
diagnosis using a multi-lingual GUI, consultant
subscription based on patient choice, and public
forums for discussions and sharing ANC experiences.
Figure 2: Overall System Architecture.
2.5.2 Web Application for PC-based Patient
Assessment and Diagnostics
Since smartphone penetration is still low in rural and
sub-urban localities of LMICs, the proposed system
also includes a web application with the complete set
of system features (Figure 3A). An extensive exercise
for user interface design and development has been
undertaken on the lines of the smart phone application
interface (mentioned above). Microsoft® ASP.NET
Web Forms (Sheriff, 2001) has been employed for the
software. This application can be leveraged by using
a personal computer with an installation of standard
web browsers.
Figure 3: (A) Web Application and Desktop Administration
Console, (B) Smart Phone App View.
B
A
Towards Providing Full Spectrum Antenatal Health Care in Low and Middle Income Countries
481

2.5.3 Desktop Application for System and
Data Administration
A stand-alone desktop application has been
developed to act as the administration console (Figure
3A). Windows Presentation Foundation (WPF)
(Chappell, 2006) has been employed to develop this
component. Using this console, authenticated doctors
and consultants are enlisted with the system by a
hospital designated administrator.
2.6 Deployment of Prototype at
Shalamar Institute of Health
Sciences (SIHS)
The system has being test-deployed at clinical site in
SIHS. Patient and consultant views are being
acquired to fine tune the GUIs as well as the
probabilities for pre-eclampsia’s Bayesian network.
A data warehouse has been established to act as
patient and self-diagnostics registry.
3 DISCUSSION & CONCLUSIONS
The work outlines the design and development of a
cloud-based ANC health support system which can be
employed by patients for self-diagnosis and by
clinical consultants to provide timely support to high
risk cases. The salient objective of this project is to
provide optimal clinical advice and support to
pregnant women in LMICs. Towards its popular
acceptance, limited financial resources of LMIC
women limits affordability of prevalent smartphone
devices and tablets. However, with a foreseeable drop
in the device costs (Hamblen, 2014), a significantly
improved affordability may be less than a decade
away. Additionally, limited availability of 3G and 4G
spectra for fast communication between the users and
the cloud may be another impediment in scaling the
system in rural and sub-urban areas of LMICs. The
relevance of the system is however anticipated to
improve with rapid penetration of communication
technologies in LMICs (PTA, 2013).
Another significant challenge in wide-spread
application of the proposed system may come from
the inability of the potential LMIC users to read non-
native languages. This has been catered for in this
work by a multilingual support (English and Urdu) in
the GUIs. For world-wide acceptance, an adequate
design allocation has been made for supporting other
native languages. Furthermore, the limited
experience of LMIC women to execute software is
also pertinent and may require tailored human-
computer interaction techniques for ensuring an
enabling user experience. Furthermore, hesitation on
part of the patients can be circumvented by providing
hands-on training to primary health care workers on
the proposed system. Since primary healthcare
networks are established in most LMICs, they can act
as vehicles of delivery and execute the diagnostics in-
tandem with the patient.
At the clinical end, a rapid increase in patient turn-
over may lead to hesitation on part of the consultants
to enrol in the system. However, an encouraging
response has been received after the system’s test-
deployment at SIHS. It is envisaged that with due
enhancements in GUIs, a streamlined patient-
consultant communication, the proposed ANC
system can gain wider subscription in Pakistan and
worldwide.
In conclusion, the proposed system aims to use
pre-existing clinical knowledge and employ
communication technologies to deliver much needed
ANC in LMICs towards reducing high IMR and
MMR.
REFERENCES
May 2014. Maternal mortality.
[Online]. Who-Media Centre Fact sheet. Available:
http://www.who.int/mediacentre/factsheets/fs348/en/.
Basso, O., Rasmussen, S., Weinberg, C. R., Wilcox, A. J.,
Irgens, L. M. & Skjaerven, R. 2006. Trends in fetal and
infant survival following preeclampsia. JAMA, 296,
1357-1362.
Bloom, S. S., Lippeveld, T. & Wypij, D. 1999. Does
antenatal care make a difference to safe delivery? A
study in urban Uttar Pradesh, India. Health policy and
planning, 14, 38-48.
Burrow, G. N., Duffy, T. P. & Copel, J. A. 2004. Medical
complications during pregnancy, Saunders.
Chappell, D. 2006. Introducing Windows Presentation
Foundation. Microsoft Developer Network. Chappell &
Associates.
Friedman, N., Geiger, D. & Goldszmidt, M. 1997. Bayesian
Network Classifiers. Mach. Learn., 29, 131-163.
Ghulmiyyah, L. & Sibai, B. Maternal mortality from
preeclampsia/eclampsia. Seminars in perinatology,
2012. Elsevier, 56-59.
Hamblen, M. 2014. Smartphone prices are dropping, and
will continue to dip through '18. Computerworld.
Hogan, M. C., Foreman, K. J., Naghavi, M., Ahn, S. Y.,
Wang, M., Makela, S. M., Lopez, A. D., Lozano, R. &
Murray, C. J. 2010. Maternal mortality for 181
countries, 1980–2008: a systematic analysis of progress
towards Millennium Development Goal 5. The lancet,
375, 1609-1623.
HEALTHINF 2016 - 9th International Conference on Health Informatics
482

Inam, S. & Khan, S. 2002. Importance of antenatal care in
reduction of maternal morbidity and mortality. Journal-
Pakistan Medical Association, 52, 137-137.
Jafarey, S. 2002. Maternal mortality in Pakistan–
compilation of available data. J Pak Med Assoc, 52,
539-44.
Mackay, A. P., Berg, C. J. & Atrash, H. K. 2001.
Pregnancy-related mortality from preeclampsia and
eclampsia. Obstetrics & Gynecology, 97, 533-538.
Martin, R. C. 2003. Agile software development: principles,
patterns, and practices, Prentice Hall PTR.
Masound, F. & Halabi, D. H. Asp. NET and JSP
Frameworks in Model View Controller
Implementation. Information and Communication
Technologies, 2006. ICTTA'06. 2nd, 2006. IEEE,
3593-3598.
Merck 2015. Merck Manuals Professional Edition.
Gynecology and Obstetrics.
Microsoft 2013. Windows Phone SDK. Microsoft
Developer Technologies. Microsoft.
Microsoft. 2014. ASP.NET Web API Framework [Online].
Available: http://www.asp.net/web-api.
Miller, B. A. & Bisdikian, C. 2001. Bluetooth revealed: the
insider's guide to an open specification for global
wireless communication, Prentice Hall PTR.
MySQL, A. 2001. MySQL.
Norbeck, J. S. & Tilden, V. P. 1983. Life stress, social
support, and emotional disequilibrium in complications
of pregnancy: a prospective, multivariate study.
Journal of Health and Social Behavior, 30-46.
Penfold, S., Shamba, D., Hanson, C., Jaribu, J., Manzi, F.,
Marchant, T., Tanner, M., Ramsey, K., Schellenberg,
D. & Schellenberg, J. A. 2013. Staff experiences of
providing maternity services in rural southern
Tanzania–a focus on equipment, drug and supply
issues. BMC health services research, 13, 61.
Peng, D.-L., Cao, L.-D. & Xu, W.-J. 2011. Using JSON for
data exchanging in web service applications. Journal of
Computational Information Systems, 7, 5883-5890.
PTA 2013. Annual Report. Pakistan Telecommunication
Authority.
Ransom, E. I., Yinger, N. V. & SASS, J. 2002. Making
motherhood safer: overcoming obstacles on the
pathway to care.
Sathar, Z., Crook, N., Callum, C. & Kazi, S. 1988. Women's
status and fertility change in Pakistan. The Population
and Development Review, 415-432.
Sattar, N. & Greer, I. A. 2002. Pregnancy complications
and maternal cardiovascular risk: opportunities for
intervention and screening? BMJ: British Medical
Journal, 325, 157.
Schmidt, W. 2010. XAML Overview. Microsoft Developer
Network. Microsoft.
Shah, I. & Åhman, E. 2004. Age patterns of unsafe abortion
in developing country regions. Reproductive Health
Matters, 12, 9-17.
Sheriff, P. D. 2001. Introduction to ASP.NET and Web
Forms. Microsoft Developer Network. Microsoft.
Titaley, C. R., Dibley, M. J. & Roberts, C. L. 2010. Factors
associated with underutilization of antenatal care
services in Indonesia: results of Indonesia
Demographic and Health Survey 2002/2003 and 2007.
BMC Public Health, 10, 485.
U.S. Department of Health and Human Services, O.
September 2010. "Pregnancy,".
UNICEF, W. 2012. UNFPA, World Bank (2012) Trends in
maternal mortality: 1990 to 2010. WHO, UNICEF.
UNFPA and The World Bank estimates. Geneva:
World Health Organization.
WHO & UNICEF 2012. Trends in maternal mortality: 1990
to 2010: WHO, UNICEF, UNFPA and The World Bank
estimates.
Towards Providing Full Spectrum Antenatal Health Care in Low and Middle Income Countries
483
