
Design of a Web-based Clinical Decision Support System for Guiding
Patients with Low Back Pain to the Best Next Step
in Primary Healthcare
Wendy Oude Nijeweme – d’Hollosy
1
, Lex van Velsen
1,2
, Remko Soer
3,4
and Hermie Hermens
1,2
1
University of Twente, MIRA, EWI/BSS Telemedicine, Enschede, The Netherlands
2
Roessingh Research and Development, Telemedicine cluster, Enschede, The Netherlands
3
University of Groningen, University Medical Center Groningen, Groningen Spine Center, Groningen, The Netherlands
4
Saxion University of Applied Science, Enschede, The Netherlands
Keywords: Classification of Patients, Clinical Decision Support Systems (CDSS), Decision Tree, Low Back Pain (LBP),
Ontology, Primary Care, Self-referral, Triage.
Abstract: Low back pain (LBP) is the most common cause for activity limitation and has a tremendous socioeconomic
impact in Western society. In primary care, LBP is commonly treated by general practitioners (GPs) and
physiotherapists. In the Netherlands, patients can opt to see a physiotherapist without referral from their GP
(so called ‘self-referral’). Although self-referral has improved the choice of care for patients, it also requires
that a patient knows exactly how to select the best next step in care for his or her situation, which is not always
evident. This paper describes the design of a web-based clinical decision support system (CDSS) that guides
patients with LBP in making suitable choices on self-referral. We studied literature and guidelines on LBP
and conducted semi-structured interviews with 3 general practitioners and 5 physiotherapists on the
classification of LBP with respect to the best next step in care: visit a GP, visit a physiotherapist or perform
self-care. The interview results were validated by means of an online survey, which resulted in a select group
of key classification factors. Based on the results, we developed an ontology and a decision tree that models
the decision making process of the CDSS.
1 INTRODUCTION
Low back pain (LBP) is the most common cause for
activity limitation in people, and has a tremendous
socioeconomic impact (Hill, 2011; Ung, 2012). More
than 80% of all persons experience low back pain in
their lifetime (Balagué, 1999). A distinction is made
between specific low back pain and non-specific low
back pain. Most cases of low back pain are non-
specific (Ehrlich, 2003). Non-specific low back pain
is defined as “pain symptoms anywhere in the lower
back between the twelfth rib and the top of the legs,
with no recognizable, specific pathology such as
infection, tumour, osteoporosis, fracture, radicular
syndrome, or cauda equina syndrome that is
attributable to the pain sensations” (Rolli Salathé,
2013).
Most people who suffer from non-specific low
back pain recover within six weeks, but about 10-15%
develop chronic symptoms (Balagué, 1999). It is not
always clear why some people with non-specific low
back pain develop chronic low back pain. In
literature, multiple risk factors have been identified,
including abnormal course of the low back pain,
patients’ belief and expectations about recovery,
anxiety, distress and depression (Weiner, 2010).
Patients with increased risk to develop chronic low
back pain should be identified and supported by the
most relevant healthcare professional at the earliest
possible stage of non-specific low back pain, thereby
reducing the development of a chronic condition
(Childs, 2015), while patients who do not have
increased risk profiles, may do well with self-
management.
In the Netherlands, patients with musculoskeletal
disorders can make use of so-called ‘self-referral’.
Patients’ self-referral, or direct access, means that
patients can be examined, evaluated and/or treated by
a physiotherapist without the requirement of a
physician referral (APTA, 2012; Swinkels, 2014).
Although self-referral has improved the freedom of
Nijeweme-d’Hollosy, W., Velsen, L., Soer, R. and Hermens, H.
Design of a Web-based Clinical Decision Support System for Guiding Patients with Low Back Pain to the Best Next Step in Primary Healthcare.
DOI: 10.5220/0005662102290239
In Proceedings of the 9th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2016) - Volume 5: HEALTHINF, pages 229-239
ISBN: 978-989-758-170-0
Copyright
c
2016 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
229

choice of care for patients with musculoskeletal
problems, it also requires that a patient knows exactly
what is the best care for his or her situation. This,
however, is not always evident, especially for those
patients that are new to musculoskeletal complaints.
Swinkels et al (2014) showed that people who
directly access the physiotherapist receive less
treatment than patients who are referred by their GP.
Next to this, Bornhöft, Larsson and Thorn (2014)
concluded that patients referred to physiotherapists
required fewer GP visits or received fewer
musculoskeletal disorders-related referrals to
specialists/external examinations, sick-leave
recommendations or prescriptions during the
following year, compared to patients that were
referred to GPs.
Although it may seem that a patient with a
musculoskeletal complaint is served best with referral
to a physiotherapist, there are also situations in which
a patient should go to the GP. Alternatively, it might
also be sufficient to perform self-care. For example,
in case of the presence of so-called ‘Red Flags’,
indicating a serious condition, the patient should
contact his or her GP (Staal, 2013). Therefore, a
correct referral for patients with low back pain is
essential for effective treatment of patients, leading to
fewer instances of chronic low back pain. Moreover,
efficient treatment alleviates the burden on
healthcare. In this paper, we describe a study that
identifies key classification factors to be used as the
basis for the development of a web-based clinical
decision support system (CDSS) that guides patients
with low back pain to the best next step in healthcare
by advising the patient to 1) see a GP, 2) see a
physiotherapist, or 3) perform self-care.
2 RELATED WORK
2.1 Classification of Patients with Low
Back Pain
In order to enable an appropriate decision for the next
step in the care of low back pain complaints, the
nature of the pain should first be classified correctly
(Hill, 2011) (Koes, 2010). Classifying patients is,
however, a difficult task, due to the high degree of
diversity of patients and risk factors.
Literature on the classification of low back pain is
extensive. This has, for example, resulted in
guidelines for GPs as well as physiotherapists for the
classification and treatment of patients with low back
pain (Chavannes, 2009) (Staal, 2013). In all
guidelines patients are classified and stratified into
groups for further treatment. A recent study showed
that stratified care for back pain implemented in
family practice leads to significant improvements in
patient disability outcomes and a halving in time off
work, without increasing health care costs (Hill,
2011; Foster, 2014).
Basically, literature shows that the classification
of patients with low back pain is mainly based on
looking for the presence of so-called “Red Flags” and
“Yellow Flags”. “Red Flags” are considered to be
serious conditions, such as trauma, cancer, and
herniated discs. “Yellow Flags” are psychosocial
factors complicating the condition as anxiety, distress
and depression. Some papers categorize “Yellow
Flags” into further detail, calling these “Blue Flags”
(factors about work that may lead to prolonged
disability) (Weiner, 2010), “Orange Flags”
(psychiatric factors), and “Black Flags” (contextual
factors as a compensation system under which
workplace injuries are managed) (Nicholas, 2011).
Flags can be used as decisive factors in the
decision process for further referral, also called
‘triage’, to determine whether the patient has to go to
the GP or to the physiotherapist, or can perform self-
care. Furthermore, flags can also be used as decisive
factors at a later stage in the healthcare process, for
example after anamnesis and physical examination of
the patient with low back pain to determine the
treatment path.
2.2 Clinical Decision Support Systems
for Healthcare Professionals as
Well as Patients
Over almost half a century, clinical decision support
system (CDSSs) have been developed to support
healthcare professionals during the clinical decision
process. The term CDSS is defined as “any computer
program designed to help healthcare professionals to
make clinical decisions” (Musen, 2014). One of the
key decision support functions is to provide patient-
specific recommendations that cover assistance in
making a diagnosis, providing advice on therapy, or
both diagnostic assistance and therapy advice
(Perreault, 1999).
CDSSs on the management of low back pain have
also been developed. These CDSSs were mainly
developed to improve uptake of guideline
recommendations on low back pain by healthcare
professionals (Peiris, 2014). Next to this, CDSSs
were developed to assist healthcare professionals in
making a diagnosis on low back pain, like detecting
chronic low back pain by the evaluation of MRI
images of the brain (Ung, 2012), classifying low back
HEALTHINF 2016 - 9th International Conference on Health Informatics
230

pain when dealing with uncertainty (Lin, 2006), and
stratifying patients in risk groups on the development
of a chronic condition based on questionnaires
(StarTBack and Örebro) (Hill, 2008)(Linton, 2003).
Besides for supporting healthcare professionals,
systems have also been developed to aid patients in
decision support. These computerized patient
decision aids range from general home healthcare
reference information to symptom management and
diagnostic decision support (Jimison, 2007). For low
back pain, computerized patients decision aids have
been developed for patients facing a surgical
treatment decision (Deyo, 2000)(Knops, 2013). No
systems have been identified in literature that support
patients in the classification of their own low back
pain prior to contacting a primary healthcare
professional. However, such a system will be very
helpful to support patients in the determination of a
correct self-referral, an essential prerequisite for an
effective treatment of patients with low back pain.
3 METHODS
The first steps in the development of a web-based
clinical decision support system that guides low back
pain patients to the most relevant healthcare
professional is finding those factors that can classify
these patients for further referral. To find these
factors, the following steps were taken:
1. Studying physiotherapist and general
practitioner guidelines on the classification and
treatment of patients with low back pain;
2. Performing in-depth, semi-structured interviews
with a group of 3 general practitioners and 5
physiotherapists;
3. Performing a thematic analyses on the interview
transcriptions;
4. Validation of the results gathered thus far by
means of an online survey among the
interviewees.
3.1 Studying Guidelines on Low Back
Pain
During this step, the Dutch physiotherapist guideline
on low back pain (Staal, 2013) and the Dutch GP
guideline on low back pain (Chavannes, 2009) have
been studied. The main goal of this step was to gain a
good understanding of the low back pain domain, the
terminology used in this domain by GPs as well as by
treatment.
3.2 Setting up and Analysis of the
Interviews
Knowledge gained from the previous step was used
to set-up the interviews. These were semi-structured
interviews, based on the following themes:
• Demographics of the interviewee (e.g., age,
specialisation);
• Expertise of the interviewee on classifying and
treating low back pain (e.g., how often the
healthcare professional sees a patient with low
back pain, how knowledge on low back pain is
kept up-to-date);
• Steps in the clinical evaluation and
classification, and management of low back
pain by questioning the healthcare professional
about specific patient cases on self-referral (see
Appendix);
• Definitions on low back pain concepts (e.g., the
differences between specific and nonspecific
low back pain);
• Future expectations of a CDSS that supports
healthcare professionals and patients in the
classification, treatment and management of low
back pain.
The interviews were held among 3 GPs and 5
physiotherapists. Afterwards, the interviews were
transcribed verbatim and analysed by means of
thematic analysis (Braun, 2006).
3.3 Validation of the Identified
Decision Factors for Classifying
Low Back Pain by Means of an
Online Survey
The previous steps resulted into a large number of
decision factors for classifying low back pain related
to further referral in care (GP, physiotherapist, or self-
care). These factors were resubmitted to the
interviewees to be validated by means of an online
survey, and by assessing:
1. The importance of being questioned during
initial triage;
2. The importance to be included into the decision
for further treatment interventions.
4 RESULTS
Studying literature and guidelines resulted in a clear
global overview of possible classes of patients with
Design of a Web-based Clinical Decision Support System for Guiding Patients with Low Back Pain to the Best Next Step in Primary
Healthcare
231
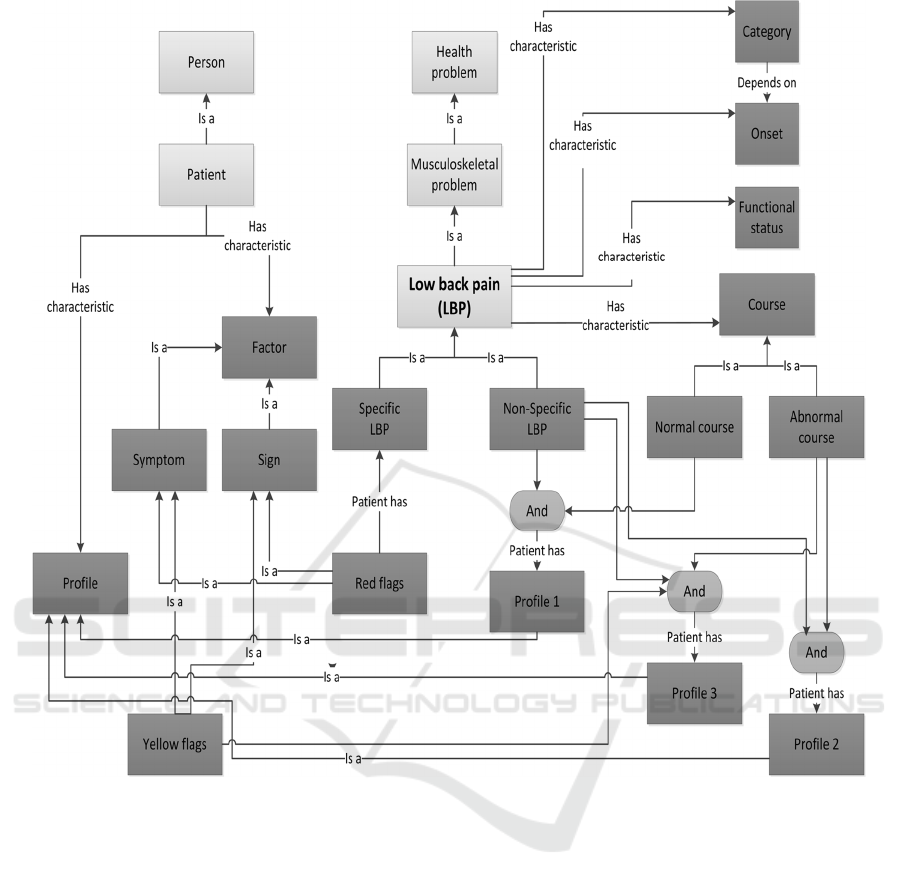
Figure 1: The knowledge model (ontology) on the classification of patients with low back pain, as deduced from guidelines
on low back pain (Chavannes, 2009) (Staal, 2013).
low back pain, and the possible prognosis and
potential risks these patients face according to these
classes. The focus of the guidelines was mainly
placed on nonspecific low back pain, but factors
related to specific low back pain were also found. We
made a visual overview of the knowledge, gained
during this step. This overview is shown as an
ontology in Figure 1. In Figure 1, the light blocks
refer to knowledge classes that are general to
knowledge concepts in the health care domain, the
dark grey blocks refer to knowledge classes that are
needed to describe the knowledge classes needed to
classify patients with low back pain. This figure also
shows three patient profiles to stratify patients with
non-specific low back pain. Profile 1 is a patient with
non-specific low back pain (no “Red Flags”) with a
normal course. Profile 2 is a patient with non-specific
low back pain with an abnormal course, but no
psychosocial factors (“Yellow Flags”). Profile 3 is a
patient with non-specific low back pain with an
abnormal course and psychosocial factors.
Figure 1 shows that the main determining factors
in classifying patients are the course of the low back
pain (normal, abnormal), the presence or absence of
serious factors (“Red Flags”) as specific underlying
serious conditions, and the presence or absence of
psychosocial factors (“Yellow Flags”). These
observations were also supported by the results of the
interviews. The analysis of the interviews resulted in
43 identified factors for classifying low back pain.
These factors are shown in Table 1.
HEALTHINF 2016 - 9th International Conference on Health Informatics
232
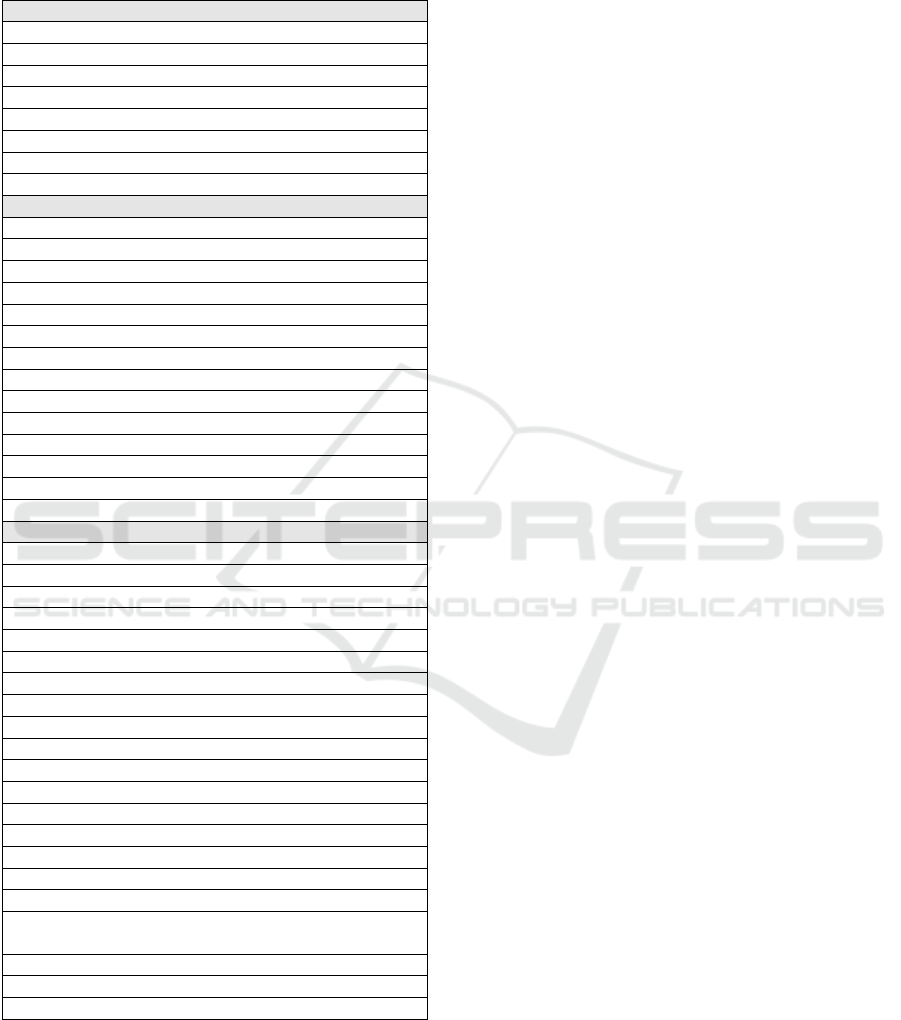
Table 1: Classification factors for patients with low back
pain, based on literature, guidelines and the interviews.
Divided in the groups ‘general’, ‘psychosomatic’, and
‘serious’.
General factors
Patients’ preference for help
Well-being as experienced by patient
Course of the LBP
Sick leave
Earlier hospitalisation on LBP
Working environment
Family history of LBP
Working ergonomics
Psychosomatic factors (“Yellow Flags”)
Depression
Extremely nervous
Extremely worried
Stress (e.g., caused by family or relational problems)
Relationship with colleagues
Irrational thoughts about LBP
Problems with employers occupational insurance
Dysfunctional cognition
Anxiety disorder
Patients’ coping strategy
An ongoing investigation on personal injury
Kinesiophobia
Personality disorder
Borderline disorder
Serious factors (“Red Flags”)
Start LBP before age of 20
Start LBP after age of 50
Response on analgesics
Prolonged use of corticosteroids
Serious diseases, such as cancer, in patient history
Neurogenic signals
Specific pathologies
Problems with moving, shortly after waking up
Continuous pain, regardless of posture and movement
Decreased mobility
Radiation in the leg below the knee
Nocturnal pain
Rapid weight loss, more than 5 kg per month
Loss of muscle strength
No biomechanical pattern
Trauma
Underlying diseases
Failure symptoms during increased pressure (e.g.,
coughing, straining, lifting gives extra pain)
Possible to walk on the toes and heels?
Incoordination
Stooped posture
The interviewees indicated that in case of the
presence of a serious factor (“Red Flag”), patients
should be sent to a GP. Next, the interviewees
indicated that in case of the presence of a
psychosocial factor (“Yellow Flag”), the patient has a
risk on the development of an abnormal course on low
back pain, possibly resulting in chronic low back
pain. In order to avoid the development of a chronic
condition, these patients should see the right
healthcare professional as early as possible, who can
then guide the patient during his or her rehabilitation
process. In most cases, this will be a physiotherapist,
sometimes working in a multi-disciplinary setting
with other healthcare professionals as, for example, a
psychologist, with the physiotherapist as head
therapist.
For the CDSS, we want to use the lowest number
of classification factors for providing the best self-
referral advice. This in order to minimize the
workload for the patient in answering questions,
posed by the CDSS. Therefore, we resubmitted the 43
identified classification factors (Table 1) to the
interviewees so that these factors could be validated
on two aspects: 1) their importance during initial
triage to determine a self-referral advice for the
patient, and 2) their importance for the decision
process to determine further treatment interventions,
also after the first anamnesis and physical
examination of the patient with low back pain by the
healthcare professional. Six of the 8 interviewees (3
physiotherapists and 3 GPs) responded on the Internet
survey. This resulted in an overview of the most
important classification factors to determine the
advice for self-referral (Figure 2) and the most
important classification factors for determining a
treatment plan (Figure 3).
Both figures show the results in radar charts. The
identified factors are labelled around the circle. The
number of times an interviewee marked the factor as
important for triage, and for determining a treatment
plan (Figure 2 and Figure 3 respectively), is plotted
for each factor as a point along a separate axis that
starts in the centre of the chart (no interviewee
marked the factor as important) and ends on the outer
ring (all 6 interviewees marked the factor as
important). Connecting these different points results
in a quick overview of the most important factors for
triage and treatment assessment. For better visibility,
we also divided the circle into three pie slices: white
represents the “general factors”, grey checked
represents the “psychosocial factors (Yellow Flags)”,
and dark grey represents the “serious factors (Red
Flags)”.
Figure 2 shows that only general and serious factors
(“Red Flags”) are pointed at the 5th and 6th rings,
fifteen factors in total. Subsequently, we used these
fifteen factors to model the inference process of the
CDSS, presented as a decision tree in Figure 4. This
Design of a Web-based Clinical Decision Support System for Guiding Patients with Low Back Pain to the Best Next Step in Primary
Healthcare
233
decision tree models the process to determine the
referral advice (see a GP, see a physiotherapist, or
perform self-care). Figure 2 shows twelve serious
factors on the 5th and 6th rings: Start of low back pain
after age of 50, prolonged use of corticosteroids,
serious diseases (e.g., cancer) in patient’s history,
neurogenic signals, continuous pain, regardless of
posture and movement, radiation in the leg below the
knee, nocturnal pain, rapid weight loss (more than 5
kg per month), loss of muscle strength, trauma, and
failure symptoms during increased pressure (e.g.,
coughing, straining, lifting gives extra pain). In
Figure 4, these serious factors are taken together in
one block to keep it as simple as possible: “# Red
flags >= 1” means the presence of one or more serious
factors.
Next, we decided that the factor “Asking patients’
preference” cannot be used in the decision process
itself, because it is no indication of patients’
condition. Therefore, the block “Asking patients’
preference” is not a part of the decision tree.
However, the healthcare professional certainly wants
to know the patient’s preference for help. Therefore
“Asking patients’ preference” is at least part of the
triage process, and will be sent to the healthcare
professional to be used during the first anamnesis,
when the patient is referred to a healthcare
professional.
5 DISCUSSION
By means of studying literature, and interviews and
an online survey among 3 GPs and 5 physiotherapists,
we identified 43 decision factors to classify low back
pain for determining the best next step in primary
healthcare. Fifteen of these identified factors have
been used to model the triage process as the basis in
the design of a web-based clinical decision support
system (CDSS) that supports patients with low back
pain in making a decision on self-referral. That is
advising the patient 1) to see a GP, 2) to see a
physiotherapist, or 3) to perform self-care. A correct
self-referral is an essential prerequisite for an
effective treatment of patients with low back pain.
The identified classification factors correspond to
classifications factors also found in literature
Figure 2: An overview of the identified factors to classify patients with low back pain, and their importance related to initial
triage of patients with low back pain.
HEALTHINF 2016 - 9th International Conference on Health Informatics
234
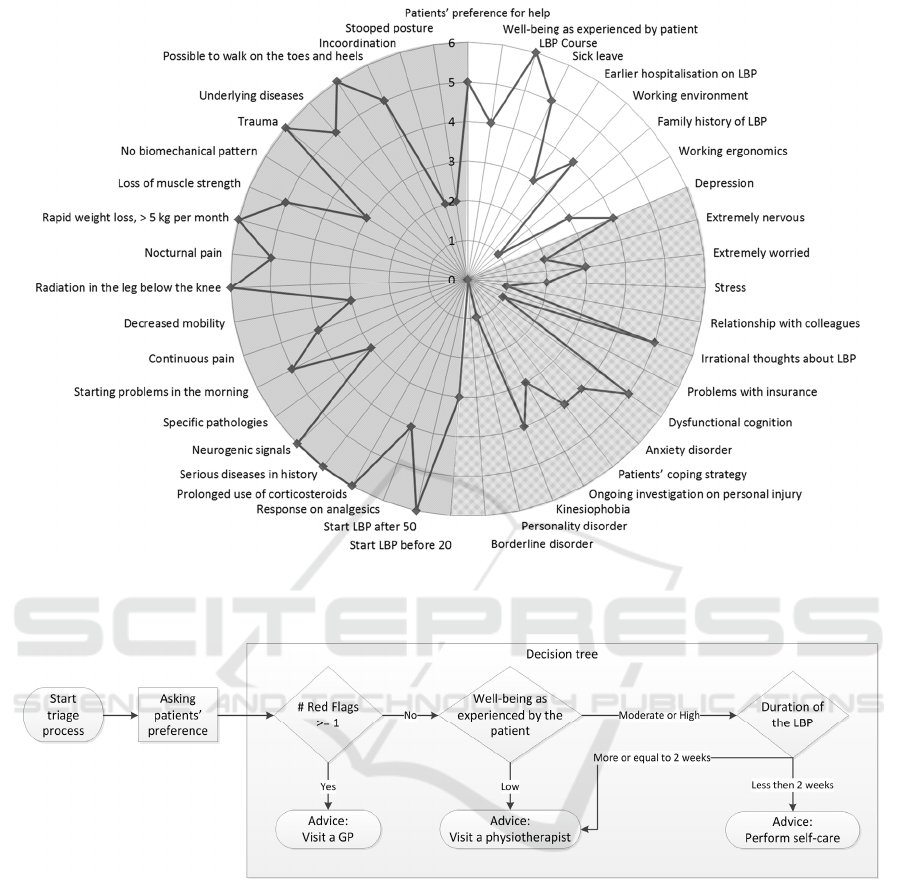
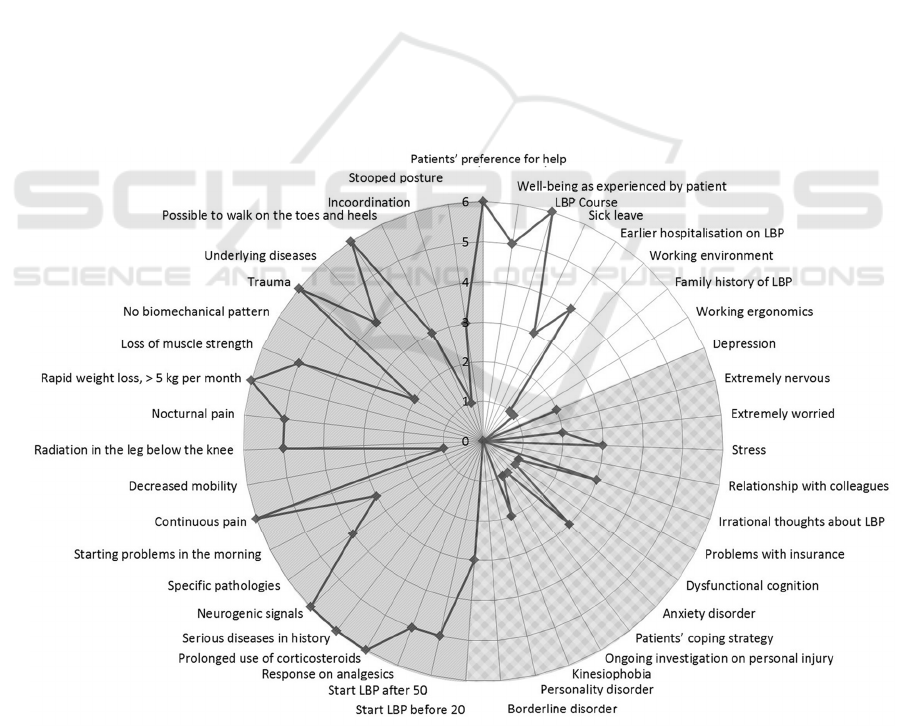
Figure 3: An overview of the identified factors to classify patients with low back pain, and their importance to determine
further treatment plans.
Figure 4: The triage process for providing advice on further referral of patients with low back pain.
(Ehrlich, 2003; Koes, 2010; Weiner, 2010; Hill,
2011). In our study, one new identified factor
emerged compared to factors found in literature,
namely the general factor “Patients’ preference for
help” (Table 1). Almost all study participants
indicated the importance of this factor in triage,
because healthcare professionals want to know the
preferences of the patient with respect to the
management of his or her low back pain complaints.
Therefore, although the factor “Patients’ preference
for help” is not an indication of patients’ condition
needed for determining the advice for further referral,
we included this factor into model of the triage
process (Figure 4).
The identified classification factors appear to be
evidence-based, which is supported by the great
overlap between our study results and the factors
found in literature. This means that the identified
factors can be used in the decision process to
determine a self-referral advice for patients suffering
from low back pain. As no other systems have been
found in literature to support patients in the
classification of their own low back pain before
contacting a primary healthcare professional, we
cannot compare our found identified factors to other
similar studies.
Looking at the classification process itself, there
are CDSSs that stratify patients in risk groups on the
Design of a Web-based Clinical Decision Support System for Guiding Patients with Low Back Pain to the Best Next Step in Primary
Healthcare
235

development of a chronic condition based on
questionnaires as the StarTBack screening tool (Hill,
2008) and the Örebro tool (Linton, 2003). These
CDSSs, however, are intended for use by healthcare
professionals and are not used to triage a patient for
further referral, but for further treatment.
This difference in usage compared to our CDSS
probably also explains the difference in classification
factors used. For example, the StarTBack screening
uses 8 prognostic factors for low back pain: two items
for functioning, and items on radiating leg pain, pain
elsewhere, depression, anxiety, fear avoidance,
catastrophizing, and bothersomeness (Foster, 2014).
These are mainly psychosocial factors, so called
“Yellow Flags”, while the identified factors in our
study for usage during initial triage are only general
and serious factors (“Red Flags”). However, the
results in our study also show the importance of
psychosocial factors (“Yellow Flags”) in the
classification process of patients with low back pain
for assessing further treatment, thus after initial triage
(Figure 3). Here, our study identifies the psychosocial
factors “Irrational thoughts about LBP” and
“Dysfunctional cognition” as most important.
5.1 Study Limitations
In our study, we used the Dutch physiotherapist
guideline on low back pain (Staal, 2013) and the
Dutch GP guideline on low back pain (Chavannes,
2009). This may be considered a limitation of our
study, especially because of the unique situation of
self-referral in the Netherlands. However, Koes et al.
(2010) compared international clinical guidelines for
the management of low back pain. This study showed
that there are some differences between international
guidelines, which may be due to a lack of strong
evidence regarding these topics or due to differences
in local health care systems. But, in general,
diagnostic as well as therapeutic recommendations
are similar among these guidelines. This indicates
that using only Dutch guidelines will not substantially
affect the results as presented in this paper.
Next to this, the interviews and the online survey
were held among a small group of GPs and
physiotherapists. Each interview was transcribed
verbatim and analysed by means of thematic analysis.
After a couple of interviews, no new themes had to be
added meaning data saturation was achieved. A low
variance in the answers on the interview questions
could be expected, because the participants all work
according to the same guidelines. Next to this, all
interviewees were experienced healthcare
professionals on low back pain. That is four of the
five interviewed physiotherapists had also a
background as manual therapist, and all GPs had
more than 10 year experience in primary care.
Because of the achieved data saturation after a few
interviews, but also because interviews are labour-
intensive, the number of interviews was kept low.
5.2 Future Work
In future research we aim to evaluate the process
model, as shown in Figure 4, in more detail. By means
of a vignette survey, also called factorial survey
(Taylor, 2006), we will present cases (vignettes) to a
group of more than 500 GPs and physiotherapists.
This vignette survey will evaluate the importance of
the presence or absence of the 15 classification
factors as identified most relevant for initial triage as
described in this paper. The outcome of the vignette
survey should lead to a smaller set of classification
factors that is an optimum between the factors
necessary to determine a correct referral advice, while
minimizing the workload for patients in answering
questions.
We will relate the remaining factors to questions
to be posed to the patients by the CDSS. For most of
the identified classification factors in our study,
validated questionnaires exist that also can be used in
the CDSS. Commonly used questionnaires in low
back pain research are, for example, the Visual
Analog Scale (VAS) for Pain (Crichton, 2001), and
the Oswestry Low Back Pain Disability
Questionnaire (Intensity, 1980).
Based on the results of the vignette survey, and
the usage of validated questionnaires that determine
the presence or absence of a factor, the CDSS will be
developed. Subsequently the CDSS will be evaluated
with patients in primary healthcare.
Figure 5 shows an overview of the intended future
utilization of the CDSS in the further referral of a
patient. The patient answers triage questions posed by
the CDSS. The entered information is used by the
CDSS to advice the patient on the best next step in
healthcare 1. visit a GP, 2. visit a physiotherapist, or
3. perform self-care. The idea is that in all cases the
primary healthcare centre will be notified about the
CDSS advice provided to a patient. When desired by
the primary healthcare centre, an extra check on the
self-care advice is possible, for example, by the
medical assistant. Next to this, the CDSS will check
the self-care process outcome after two weeks. This
is different from the current healthcare process in
which a patient can notify the primary healthcare
centre on his or her self-care progress, but which is
not usually the case when the patient becomes free
HEALTHINF 2016 - 9th International Conference on Health Informatics
236
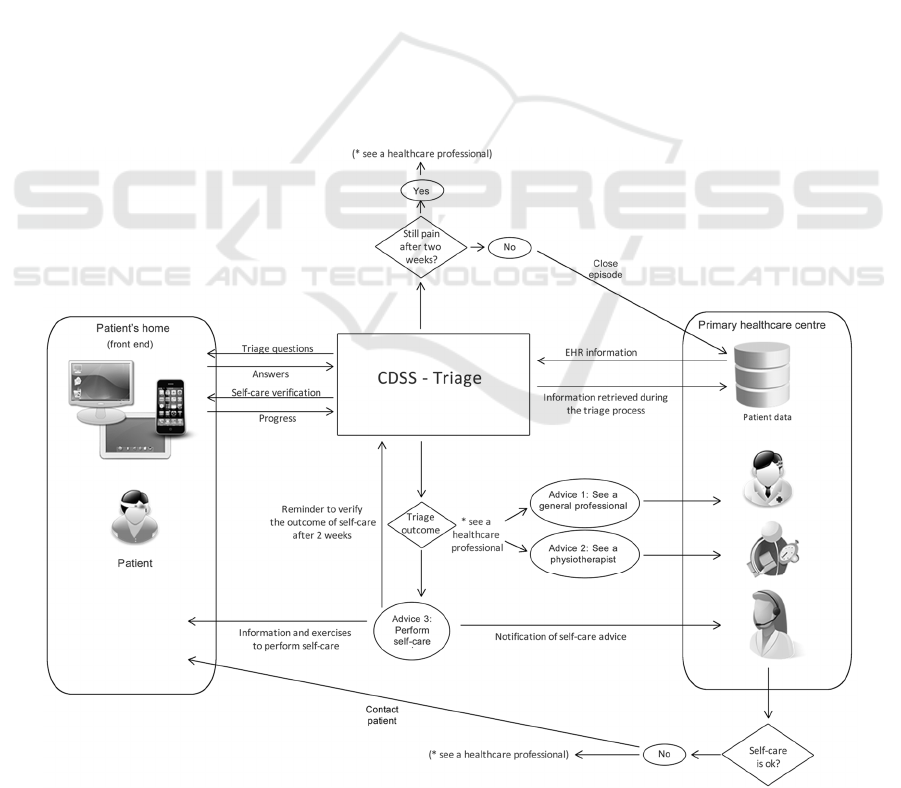
of low back pain.
The CDSS retrieves healthcare information from
the patient. This information can also already be
available within the electronic health record (EHR) of
the patient. Therefore, interoperability between the
CDSS and the healthcare information system is
desired. Advantages of interoperable systems are that
already known information does not need to be
requested from the patient by the CDSS. Next to this,
information retrieved by the CDSS can be stored in
the EHR so that it becomes available to the healthcare
professional, to be used during a consultation with the
patient.
The ontology we developed in our study is the
first step in the realization of interoperable systems,
and this ontology will be further developed during our
CDSS project based on further research findings
during the design process of the CDSS. Knowing the
used knowledge concepts by the CDSS, these can be
related to a terminology system, as SNOMED CT
(SNOMED CT, 2015), that can on its turn serve as an
intermediate terminology system to exchange
information among different healthcare IT systems.
Next to this, we now focussed on low back pain,
because the musculoskeletal disorder domain is a
large domain (Oude Nijeweme - d’Hollosy, 2015). By
using general approaches to design the CDSS, as
building an ontology and a decision tree we expect
these same approaches are also applicable to extend
the CDSS for self-referral advice on other
musculoskeletal disorders.
ACKNOWLEDGEMENTS
This work has been conducted within the context of
the eLabEL project. eLabEL is a project of the Centre
for Care Technology Research. eLabEL aims to
contribute to the sustainability of primary care by
developing, implementing and evaluating innovative,
integrated Telemedicine technology by means of a
Living Lab approach.
More information can be found at:
http://www.caretechnologyresearch.nl/elabel.
This work is partly funded by a grant from the
Netherlands Organization for Health Research and
Development (ZonMw); grant number: 10-10400-98-
009.
Figure 5: Overview of the future utilization of the CDSS in the further referral of a patient.
Design of a Web-based Clinical Decision Support System for Guiding Patients with Low Back Pain to the Best Next Step in Primary
Healthcare
237

We thank the participating healthcare professionals
for their cooperation in our research.
REFERENCES
American Physical Therapy Association (APTA), 2015, A
summary of direct access language in state physical
therapy practice acts, http://www.apta.org/uploadedFi
les/APTAorg/Advocacy/State/Issues/Direct_Access/D
irectAccessbyState.pdf, Sep 9, 2015.
Balagué, F., Troussier, B. and Salminen, J. J., 1999. Non-
specific low back pain in children and adolescents: risk
factors. European spine journal, 8(6), 429-438.
Bornhöft, L., Larsson, M. E., and Thorn, J., 2014.
Physiotherapy in Primary Care Triage-the effects on
utilization of medical services at primary health care
clinics by patients and sub-groups of patients with
musculoskeletal disorders: a case-control study.
Physiotherapy theory and practice, 31(1), 45-52.
Braun, V. and Clarke, V., 2006. Using thematic analysis in
psychology. Qualitative research in psychology, 3(2),
77-101.
Chavannes, A. W., Mens, J. M. A., Koes, B. W., Lubbers,
W. J., Ostelo, R. W. J. G., Spinnewijn, W. E. M., and
Kolnaar, B. G. M., 2009. NHG-standaard aspecifieke
lagerugpijn. NHG-Standaarden 2009, Bohn Stafleu van
Loghum, 1128-1144.
Childs, J. D., Fritz, J. M., Wu, S. S., Flynn, T. W., Wainner,
R. S., Robertson, E. K., Kim, F. S. and George, S. Z.,
2015. Implications of early and guideline adherent
physical therapy for low back pain on utilization and
costs. BMC health services research, 15(1), 150.
Crichton, N., 2001. Visual analogue scale (VAS). Journal
of Clinical Nursing, 10(5), 706.
Deyo, R. A., Cherkin, D. C., Weinstein, J., Howe, J., Ciol,
M., and Mulley, A. G., 2000. Involving patients in
clinical decisions: impact of an interactive video
program on use of back surgery. Medical care, 38(9),
959-969.
Ehrlich, G. E., 2003. Low back pain. Bulletin of the World
Health Organization, 81(9), 671.
Foster, N. E., Mullis, R., Hill, J. C., Lewis, M., Whitehurst,
D. G. T., Doyle, C., Konstantinou, K., Main, C.,
Somerville, E., Sowden, G., Wathall, S., Young, J., and
Hay, E. M., 2014. Effect of stratified care for low back
pain in family practice (IMPaCT Back): a prospective
population-based sequential comparison. The Annals of
Family Medicine, 12(2), 102-111.
Hill, J. C., Whitehurst, D. G. T., Lewis, M., Bryan, S.,
Dunn, K. M., Foster, N. E., Konstantinou, K., Main, C.
J., Mason, E., Somerville, S., Sowden, G., Vohora, K.
and Hay, E. M., 2011. Comparison of stratified primary
care management for low back pain with current best
practice (STarT Back): a randomised controlled trial.
The Lancet, 378(9802), 1560-1571.
Intensity, P., 1980. Modified Oswestry Low Back Pain
Disability Questionnaire. Physiotherapy, 66, 271-273.
Jimison, H. B., Sher, P. P., and Jimison, J. J., 2007.
Decision Support for Patients, in Berner, E. S. (ed.)
Clinical Decision Support Systems: Theory and
Practice, Springer Science & Business Media, 249-261.
Knops, A. M., Legemate, D. A., Goossens, A., Bossuyt, P.
M. and Ubbink, D. T., 2013. Decision aids for patients
facing a surgical treatment decision: a systematic
review and meta-analysis. Annals of surgery, 257(5),
860-866.
Koes, B. W., van Tulder, M., Lin, C. W. C., Macedo, L. G.,
McAuley, J., and Maher, C., 2010. An updated
overview of clinical guidelines for the management of
non-specific low back pain in primary care. European
Spine Journal, 19(12), 2075-2094.
Lin, L., Hu, P. J. H., and Sheng, O. R. L., 2006. A decision
support system for lower back pain diagnosis:
uncertainty management and clinical evaluations.
Decision Support Systems, 42(2), 1152-1169.
Linton, S. J. and Boersma, K., 2003. Early identification of
patients at risk of developing a persistent back problem:
the predictive validity of the Örebro Musculoskeletal
Pain Questionnaire. The Clinical journal of pain, 19(2),
80-86.
Musen, M. A., Middleton, B., and Greenes, R. A. , 2014.
Clinical decision-support systems. In Biomedical
informatics, Springer London, Chapter 20, 643-674.
Nicholas, M. K., Linton, S. J., Watson, P. J. and Main, C.
J., 2011. Early identification and management of
psychological risk factors (“yellow flags”) in patients
with low back pain: a reappraisal. Physical therapy,
91(5).
Oude Nijeweme – d’Hollosy, W., van Velsen, L., Swinkels,
I. C. S., and Hermens H., 2015. Clinical Decision
Support Systems for Primary Care: The Identification
of Promising Application areas and an Initial Design of
a CDSS for lower back pain. In Proceedings 17th
International Symposium on Health Information
Management Research (ISHIMR 2015), York, England,
49-59.
Peiris, D., Williams, C., Holbrook, R., Lindner, R., Reeve,
J., Das, A. and Maher, C., 2014. A Web-Based Clinical
Decision Support Tool for Primary Health Care
Management of Back Pain: Development and Mixed
Methods Evaluation, In JMIR research protocols, 3(2).
Perreault, L. E., and Metzger, J. B., 1999. A pragmatic
framework for understanding clinical decision support.
Journal of Healthcare Information Management, 13, 5-
22.
Rolli Salathé, C., and Elfering, A., 2013. A health-and
resource-oriented perspective on NSLBP. ISRN Pain,
vol. 2013, Article ID 640690, 19 pages,
doi:10.1155/2013/640690.
SNOMED CT, The Global Language of Healthcare,
IHTSDO, http://www.ihtsdo.org/snomed-ct, Nov 8
2015.
Staal, J. B., Hendriks, E. J. M. , Heijmans, M., Kiers, H.,
Lutgers-Boomsma, A. M. , Rutten, G., van Tulder, M.
W., Den Boer, J., Ostelo, R. and Custers, J. W. H., 2013.
KNGF-richtlijn lage rugpijn, Koninklijk Nederlands
HEALTHINF 2016 - 9th International Conference on Health Informatics
238

Genootschap voor Fysiotherapie, De Gans. Amersfoort,
The Netherlands (Dutch).
Swinkels, I. C. S., Kooijman, M. K., Spreeuwenberg, P. M.,
Bossen, D., Leemrijse, C. J., van Dijk, C. E., Verheij,
R., de Bakker, D. H., and Veenhof, C., 2014. An
overview of 5 years of patient self-referral for physical
therapy in the Netherlands. Physical Therapy, 94(12),
1985-1995.
Taylor, B. J., 2006. Factorial surveys: Using vignettes to
study professional judgement. British Journal of Social
Work, 36(7), 1187-1207.
Ung, H., Brown, J. E., Johnson, K. A., Younger, J., Hush,
J. and Mackey, S., 2012. Multivariate classification of
structural MRI data detects chronic low back pain,
Cerebral cortex, bhs378.
Weiner, S. S., and Nordin, M., 2010. Prevention and
management of chronic back pain. Best Practice &
Research Clinical Rheumatology, 24(2), 267-279.
APPENDIX
During the semi-structured interviews, the following
patient cases were presented to the interviewees. For
each case, the interviewee was asked about the
clinical evaluation and classification, management of
low back pain, and the ultimate advice on self-
referral: see a GP, see a physiotherapist, or perform
self-care.
Case 1
• Male, 53 years, bus driver, married;
• Tennis: 2 times a week;
• Since three weeks, he has a burden of the
spine with radiation just above right knee;
• Also low back pain problems in the past;
• Six years ago, some X-rays were made not
showing any causes to explain symptoms;
• On sick leave at the moment;
• Worried that something has been broken in his
back;
• He avoids pain;
• No pain during lying and sitting down.
Case 2
• Female, 69 years old, divorced;
• Low body weight;
• Sleeps poorly;
• Worrying a lot and feeling nervous;
• Has low back pain complaints since several
weeks;
• Continuous pain, independent of posture and
movement;
• Walks crooked.
Case 3
• Male, 39 years, bricklayer;
• Wants to visit primary healthcare for the 2
nd
time in 3 months, because of no improvement
in low back pain complaints despite
medication and advice;
• Otherwise a healthy person;
• No symptoms below the knee;
• Moves slowly, because of pain presence;
• Only walks short distances;
• Believes that low back pain will never end;
• 100% sick leave.
Case 4
• Female, 15 years old, follows 4th grade high
school education;
• Suffers from low back pain since 6 months;
• Unclear start and cause of the low back pain;
• Plays handball;
• Otherwise a healthy person;
• Little pain when lying and sitting;
• Stiffness in the morning.
Design of a Web-based Clinical Decision Support System for Guiding Patients with Low Back Pain to the Best Next Step in Primary
Healthcare
239
