
Impact of Population Ageing on Hospital Demand
Bożena Mielczarek and Jacek Zabawa
Faculty of Computer Science and Management, Wrocław University of Science and Technology,
Wyb. Wyspiańskiego 27, 50-370 Wrocław, Poland
Keywords: Hybrid Simulation, Healthcare Demand, Population Ageing.
Abstract: This paper explores the consequences of demographic changes on future access to hospital beds. It is based
on the situation in a Polish administrative region called the Wrocław Region (WR). The aim of the paper is
to quantify the impact of population ageing on hospital demand with particular emphasis on neurological
patients. A computer simulation model was used to project the population evolution during the period 2016-
2030 and forecast the number of neurological patients to be admitted to the WR hospitals. We found that the
growth of the WR population will have a large impact on the number of elderly patients, including persons
with diagnosed neurological disorders. The simulation experiments predict a continuous rise in the demand,
and the ageing alone will increase the number of neurological patients in WR, on average, by 8.5 % between
2016 and 2030.
1 INTRODUCTION
Forecasting hospital demand is essential when
developing long-term healthcare policies on the
national or regional level. The available resources are
usually limited and choices have to be made between
different interventions, treatments, diagnostic
procedures, and care processes. Effective planning
also requires adjustments in the number of beds
assigned to different medical specialties to cover the
future needs of the population inhabiting the region.
The common practice is to perform an analysis of the
previous utilization of hospital beds, develop
forecasts describing the predicted demand, and plan
the allocation of the available resources in accordance
with the forecasted needs of the population.
The demand for healthcare services is driven by a
range of different factors, from which the
epidemiological and demographic trends have the
most significant influence on the number and type of
medical needs expressed by the population. The
demographic ageing in the developed countries is
described by a shift in the age structure towards the
older cohorts. As the population of elderly grows, the
demand for healthcare services is expected to increase
considerably (Strunk et al., 2006; Burkett et al,. 2017;
Aboagye−Sarfo et al., 2016). The effect of ageing
varies across the major groups of healthcare services
and is strongly connected to a type of medical
condition and disease group (Vrhovec and Tajnikar,
2016). The observed morbidity trends force
adjustments to be made in the capacity of hospital
wards to better map the distribution of inpatient
utilization rates.
With the growing complexity of policy issues,
there is a pressing need for computer-aided modelling
tools that can enable rational resource-related
decisions for hospital bed planning in the short- and
long-term. Such a possibility is offered by simulation
modelling. Simulation techniques have been
extensively employed to analyse and design
healthcare systems for a long time, but an extensive
increase in use of simulation in healthcare studies has
been observed since 2000 (Chahal et al., 2013).
According to Mielczarek (2016), the main fields of
applying simulation approaches in healthcare
management may be categorised as health policy,
healthcare system operations and improvements,
forecasting and healthcare system design, medical
decision-making, and healthcare planning involving
extreme events. Hospital bed optimization, a
subgroup of system operations and improvements
group, has also been addressed by simulation
modelling methods (Cochran and Bharti, 2006;
Harper and Shahani, 2002; Harrison et al., 2005). The
object under study is usually a single unit or a
complex of mutually related clinics. The models are
used to study the influence of the changes in demand
Mielczarek, B. and Zabawa, J.
Impact of Population Ageing on Hospital Demand.
DOI: 10.5220/0006904404590466
In Proceedings of 8th International Conference on Simulation and Modeling Methodologies, Technologies and Applications (SIMULTECH 2018), pages 459-466
ISBN: 978-989-758-323-0
Copyright © 2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
459

on the healthcare units’ standards of service and try
to suggest improvements to the internal organisation
of the unit, assuming a certain level and structure of
demand.
The overall aim of this paper is to describe the
construction of a hybrid simulation model to
investigate the impact of population ageing on the
growing demand for inpatient hospital services in
neurological wards in south-western part of Poland.
Hybrid simulation refers to the combination of
continuous and discrete modelling methods
(Mustafee et al., 2015). The term hybrid describes an
approach that integrates methods and techniques
hitherto occurring independently. The reason for
using a hybrid model is an expectation to gain some
additional benefits that are unobtainable when using
the particular methods independently. Arisha and
Rashwan (2016) confirm that hybrid simulations are
becoming more popular because of their ability to
overcome the limitations of a single-approach
paradigm. Moreover, a hybrid simulation in
healthcare decision making could assure the balance
between strategic and operational management
(Chahal and Eldabi, 2008), particularly at the regional
level.
2 DATA AND METHODS
2.1 Study Design and Setting
The Wrocław Region (WR) is in the south-western
part of Poland and constitutes the core area of the 4
th
biggest Polish administrative region – Lower Silesia.
The population of WR was approximately 1.22
million in 2016, about 3.2% of the nation’s
population and 42.1% of Lower Silesia’s population.
It is projected to increase to 1.25 million in 2030.
The inpatient healthcare system of WR is based
on 17 public hospitals that can be freely selected by
insured inhabitants of WR, as well as patients from
other Lower Silesia subregions and citizens from
other Polish provinces. There are 8 neurological
wards in WR (general, paediatric, and rehabilitation
wards) out of 19 situated in Lower Silesia area. In
2016, there were 220 neurological beds (out of 522 in
Lower Silesia) and the average length of stay (LOS)
was 6.7 days. The annual utilization, calculated as the
quotient of the product of the number of patients and
LOS by the number of beds, then rescaled for 365
days, is very high, that is 86% in 2015 and 82% in
2016. The average waiting time for admission ranges
between 70 and 300 days.
The official projection prepared by Polish
Ministry of Health (2018) forecasts that number of
neurological patients between 2016 and 2029 will
increase by 5.4%.
2.2 Data Sources
The historical data describing the WR population was
extracted from Polish Central Statistical Office (GUS
2017) for the period 2010 – 2016, separately for 36
age-gender groups (0–4, 5–9, 10–14, 15–19, 20–24,
25–29, 30–34, 35–39, 40–44, 45–49, 50–54, 55–59,
60–64, 65–69, 70–74, 75–79, 80–84, 85–105): 18
female and 18 male cohorts.
Beyond the year 2016, the trends describing the
expected changes in the WR population were
elaborated based on the official projections prepared
by the Polish Government (Waligórska et al., 2014).
There are four main variants of the possible
demographic changes of Polish population (Table 1).
These variants predict different but probable trends
according to which the WR population is expected to
evolve. The variant no. 2 is officially considered to be
the most probable one.
The data on arrivals to WR hospitals were
obtained from the National Health Fund (NHF)
database, routinely collected and managed by NHF
regional offices. It contains patient-level data
covering all hospital stays, mode of arrivals, and the
courses of the treatment processes while staying in
the hospital wards. De-identified data were requested
to preserve patient privacy. The basic data sets
include information on 183,517 admissions in 2010
to 17 hospitals located in WR.
Table 1: Four main variants of the possible demographic
changes of Polish population.
Fertility
rate
Mortality
rate
Life
expectancy
Migration
1 Low Low High Medium
2 Medium Medium Medium Medium
3 High Medium Medium Medium
4 V. High V. High Low Medium
2.3 Methods
We have constructed a hybrid simulation model using
two simulation methods to predict the influence of
population ageing on hospital demand.
The demographic changes of the WR population
were projected using the well-established
methodology (Forrester, 1968) of system dynamics
SIMULTECH 2018 - 8th International Conference on Simulation and Modeling Methodologies, Technologies and Applications
460
and the algorithm developed by Eberlein et al. (2013)
to precisely model the ageing population. We have
applied the extended version of our model described
in detail in (Mielczarek and Zabawa, 2018).. That
model generated numerically appropriate and
validated forecasts. However, it was characterized by
some drawbacks. For example, tedious calculations
had to be made each time new data were added to the
input database to recalculate the maturation times
between consecutive age-gender cohorts. The
improved version of our demographic forecasting
model divides the population under study into 210
elementary cohorts (105 cohorts per each gender).
One cohort simulates one year of ageing of males and
(separately) females.
In order to speed up the simulation experiments,
we grouped 210 elementary cohorts into 36 main
cohorts (18 per each gender). Each main cohort
encapsulates five elementary cohorts (see Figure 1).
For simplicity, it was assumed that demographic
factors are constant for each elementary cohort being
a part of the main cohort.
Figure 1: Demographic model: main cohort decomposes
into the chain of elementary cohorts.
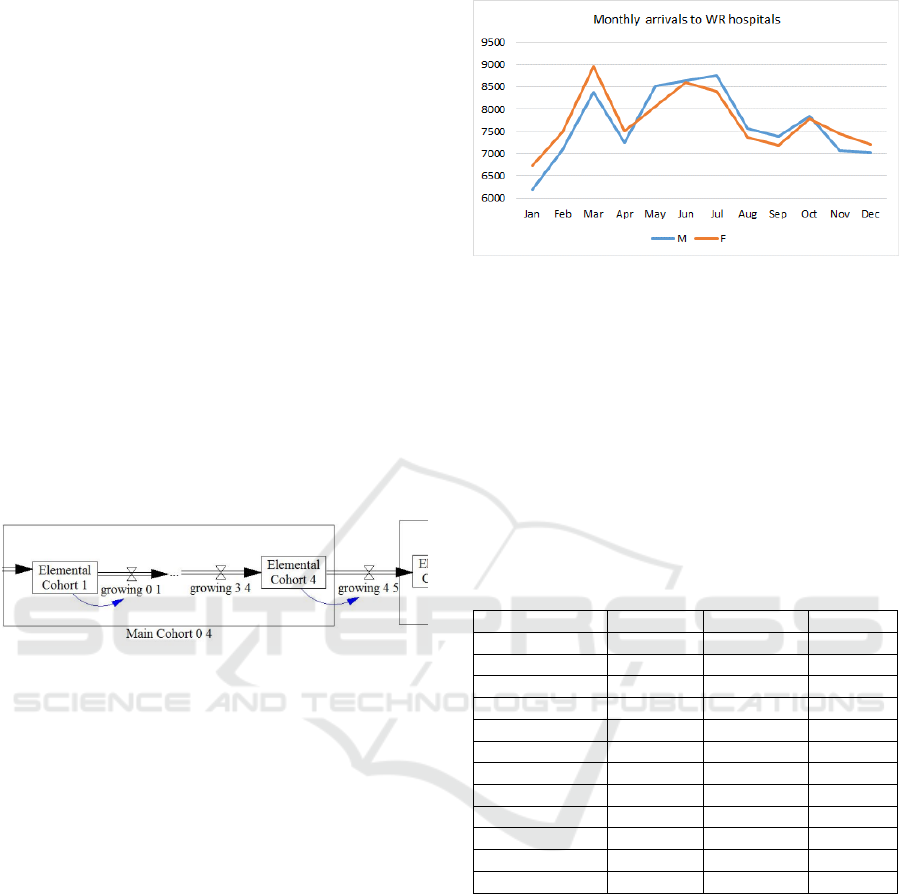
To model the demand for hospital services we
constructed discrete event simulation model (DES).
Flows of patients are generated separately for every
age-gender cohort and arrival rates change according
to calendar month (see Figure 2). Arriving patients
acquire individual attributes, like the district the
patient comes from, the diagnosis code according to
ICD-10 (International Classification of Diseases), the
hospital she selects to be treated in, the treatment she
receives when staying in a hospital ward, length of
stay, and many others. The attributes are interrelated
and mutually dependent. For example, the ICD code
of the main diagnosis determines the ward the patient
will be treated in.
Patient pathways and times between activities are
described by random values sampled from parametric
and empirical distributions. We used random variable
distributions to model the arrival processes, hospital
choices, morbidity trends, service times, likelihood of
intervention, number and type of services delivered to
patients, and others.
Figure 2: Seasonal changes in total monthly admissions to
WR hospitals.
The model was tested using a historical validation
and a comparative analysis between model output and
actual performance of the system. The results of the
simulation are consistent with the historical data and
acceptable for the estimation of WR demand
(Table 2).
Table 2: Historical validation performed for total monthly
number of patients as registered in the WR in 2010:
comparison of current system performance and results of
simulation (10 replications) – values of mean percentage
errors (MPE).
Month Historical Simulation MPE(%)
January 460 457 -0.66%
February 570 573 0.52%
March 612 609 -0.45%
April 535 533 -0.40%
May 588 586 -0.31%
June 629 631 0.36%
July 604 607 0.54%
August 526 535 1.65%
September 526 526 0.01%
October 552 549 -0.45%
November 531 528 -0.54%
December 498 500 0.32%
3 SIMULATION MODEL
3.1 Overall Algorithm
The challenge was to create the credible framework
that would enable us to link the demographic
evolutions of WR population with future hospital
demand. We have elaborated the four-phases
algorithm described below.
First, using the SD model, we performed the
demographic simulation for the years 2010-2016,
based on historical parameters that describe the WR
population. Starting from 2016, we applied the
Impact of Population Ageing on Hospital Demand
461
extrapolated fertility, mortality, and immigration
rates 15 years into the future, that is until 2030. The
most probable variant (scenario 2 as described in
par. 2.2) is considered as the base scenario.
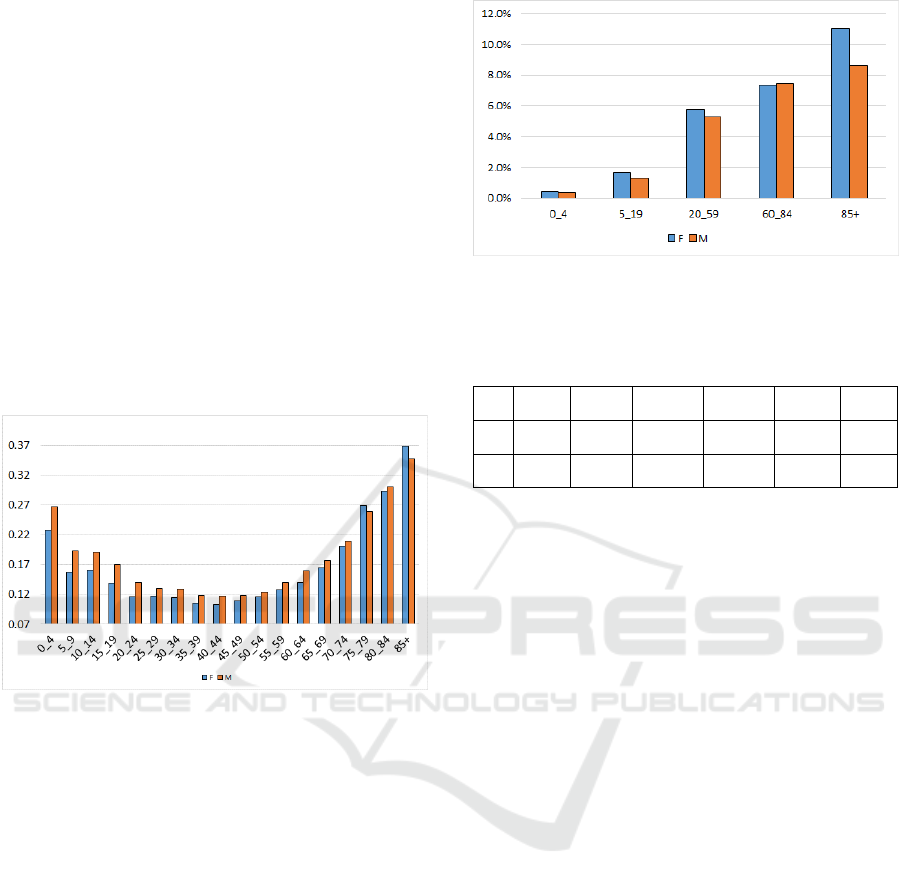
Second, following Strunk et al. (2006), we
calculated age-gender specific WR demand indexes
using 2010 demographic data and 2010 hospital
arrivals data. There are 36 values describing the
varying effect of ageing of WR population on total
inpatient hospital demand (Figure 3). The youngest
and the oldest cohorts are likely to generate higher
demand compared to middle-aged groups. We
assumed the demand indexes remain constant and
may be used to estimate the volume of demand
corresponding to the simulated changes in the
structure of WR population. We also assumed that all
other drivers of hospital demand remain stable.
Figure 3: Calculated hospital demand indexes per age-
gender cohort [patients/population].
Third, given the population projections and
hospital demand indexes describing the needs for
hospital treatment that correspond to each age-gender
cohort, we estimated the number of future inpatients.
This enabled us to calculate the values of new arrival
rates for every year beyond 2016.
Fourth, DES simulation was performed to follow
individual patients as they pass through the healthcare
system, and their progress depends on uncertainties
associated with admission and the length of delays in
internal processes. During simulation, every patient
receives the ICD code used to classify this patient to
a medical speciality and direct her to the
corresponding hospital ward. Figure 4 and Table 3
demonstrate the probabilities of being classified as a
neurological patient. The older the patient, the higher
probability of being admitted to a neurological ward.
Although the values for both genders are very similar,
a small difference may be observed between female
and male cohorts. For the oldest cohort (85+) this
difference is even more visible.
Figure 4: Probabilities of being diagnosed as a neurological
patient within given age-gender group.
Table 3: Percentage of being diagnosed as a neurological
patient within given age-gender group [%].
0_4 5_19 20_59 60_84 85+ All
F 0.47 1.65 5.76 7.35 11.06 5.39
M 0.36 1.32 5.29 7.46 8.63 4.59
3.2 Experiments
Simulation experiments were conducted according to
three officially published demographic scenarios (see
Table 1): scenario 2 (base scenario), scenario 1, and
scenario 4. According to scenarios 1 and 2, the WR
population will record the initial growth period.
However, around 2025, a stable and decreasing trend
will be observed (Figure 5). Scenario 4 predicts the
continuous increase of the WR population until 2030.
However, the speed of this growth begins to weaken
around 2025.
Although all three examined scenarios forecast
the initial demographic growth, the region is
characterized by an ageing population. It is expected
that by 2030, the percentage share of the eldest among
the WR population will increase from 22.95% in 2016
to 25.18% (Scenario 4), 25.46% (Scenario 1), or
25.64 (Scenario 2) (see Figure 6).
Population projections obtained from the
simulation demographic model were used to estimate
future healthcare demand through discrete
simulation. Two main outcome measures were
applied: the overall demand for healthcare services in
WR and the number of neurological patients arriving
to WR hospitals, stratified by age group and sex.
Every experiment was replicated 10 times and
covered the period from 2016 to 2030.
SIMULTECH 2018 - 8th International Conference on Simulation and Modeling Methodologies, Technologies and Applications
462
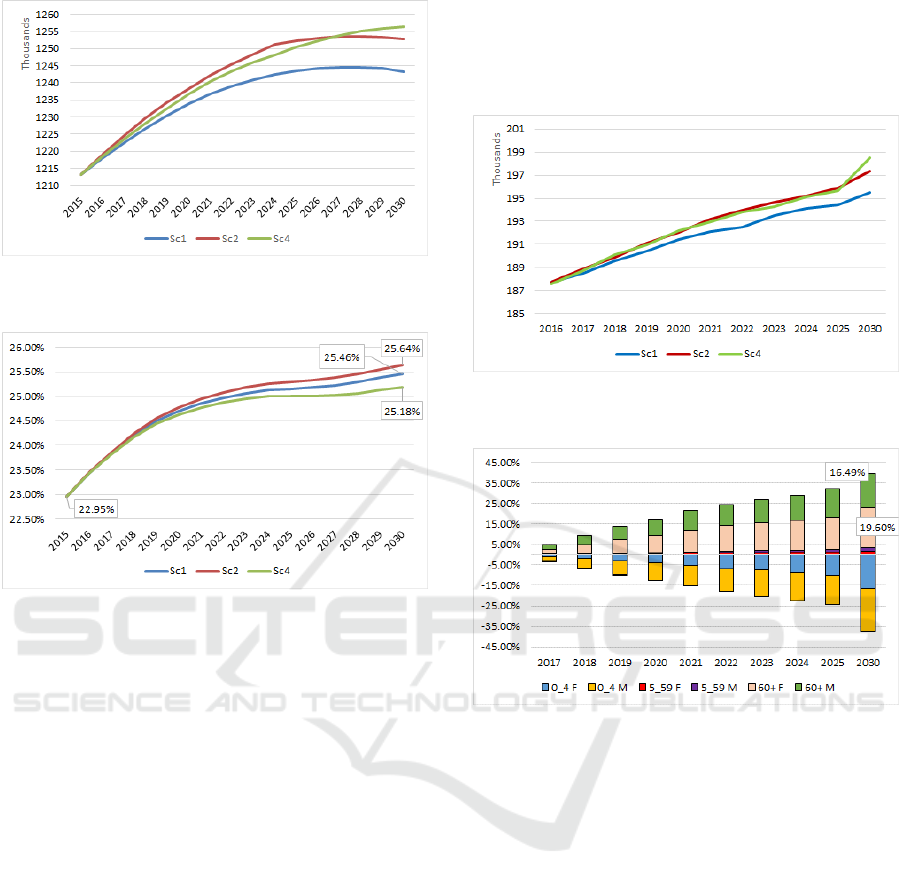
Figure 5: Predicted total WR population trends according to
three scenarios: scenario 1, scenario 2, and scenario 4.
Figure 6: Predicted percentage share of the oldest persons
(60+) among total WR population, according to three
scenarios: scenario 1, scenario 2, and scenario 4.
4 SIMULATION RESULTS
4.1 Ageing Effect on Total Hospital
Admissions
The results of the impact of three scenarios on the
estimated number of patient arrivals to WR hospitals
are presented in Figure 7. It is predicted that there will
be a 4.15% (Scenario 1), 5.17% (Scenario 2), and
5.82% (Scenario 4) increase in overall WR
admissions from 2016 to 2030 (Figure 7). Population
growth over this period will be 2.46% (Scenario 1),
3.25% (Scenario 2), and 3.56% (Scenario 4). It means
that the growth rate in overall arrivals will exceed that
of population growth.
The growth of overall demand is observed across
all age groups, except the two youngest cohorts, for
which the stable and significant decrease in the
number of arrivals is predicted, Figure 8.
According to scenario 2, the demand generated by
the oldest female population was estimated to grow
by 19.6% over the next 15 years. During the same
period, the number of the oldest male patients will
increase by 16.49%. This would translate to over
42 300 female patients and 27 800 male patients in
2030 from the current level of 35 400 and 23 900
female and male patients in 2016.
Figure 7: Projected total WR arrivals according to three
scenarios.
Figure 8: Percentage changes of healthcare arrivals by age-
gender groups - in relation to 2016 and according to
Scenario 2.
4.2 Ageing Effect on Neurological
Admissions
Neurological disorders are diseases of the brain,
spine, and the nerves that connect them. There are
more than 600 diseases of the nervous system, such
as brain tumours, epilepsy, Parkinson's disease,
stroke, and others. Neurologic diseases are the major
cause of death and disability in elderly patients
(Nentwich and Grimmnitz, 2016). They are more
common in geriatric patients because of the
physiologic changes and comorbidities that occur
when people age.
The strategic analysis published by Polish
Ministry of Health (2018) recommends immediate
increase in the availability of neurological beds.
Based on the methodology we have developed,
we ran simulation experiments to predict future
demand for neurological beds in WR hospitals. The
Impact of Population Ageing on Hospital Demand
463
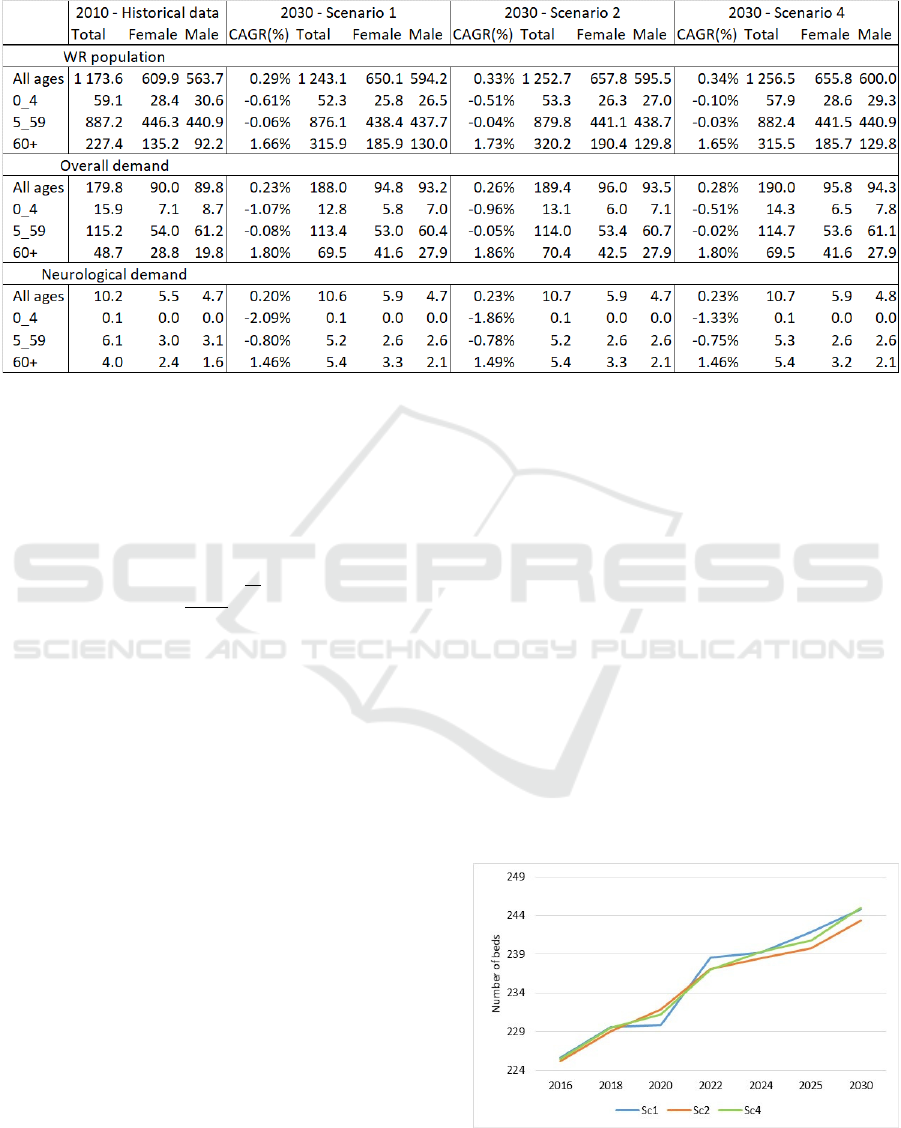
Table 4: Predicted number (in thousands) and compound annual growth rate (CAGR) of neurological patients demand in WR
by 2030, overall and by age-gender groups. Historical data and simulation output.
projections for overall demand in all the tested
scenarios were similar. However, some discrepancies
were observed, as shown in Table 3.
Following (Aboagye−Sarfo et al., 2016), we
calculated compound annual growth rate (CAGR) of
neurological demand (Formula 1),
=
−1
(1)
where
and
are the values of neurological
demand in 2010 and 2030, and 20 is the number of
years between 2010 and 2030, (see Table 4).
Between 2010 and 2030, the number of
neurological patients in WR hospitals will rise,
according to Scenario 2 (base scenario), from 10 198
to 10 670, that is by 4.6%. Looking at the period
between 2016 and 2030, this growth is even more
significant and is equal to 8.5%. Between 2010 and
2030, the increase in the number of the oldest patients
with neurological disorders will be from 4 008 (2010)
to 5 393 (2030), which gives an extremely high value
of increment, that is 34.5%.
The values of CAGR calculated for neurological
demand in the oldest cohorts are between 1.46%
(scenario 1 and 4) to 1.49% (scenario 2). When
comparing to CAGR values for overall demand
(1.86% in scenario no 2 and 1.80% in scenarios no 1
and no 4) during the same period, it is clear that the
increase in neurological demand in the oldest
population is almost as high as the increase of the
overall healthcare demand. Knowing that older
patients require more complex and more costly
treatments, these predictions show a significant
economic effect of ageing on the whole healthcare
system.
4.3 Ageing Effect on Neurological Beds
Based on the estimated level of the demand for
neurological hospital admissions, we calculated the
number of neurological beds needed to keep the
annual utilization coefficients on the desired level.
The recommended value of this coefficient for
neurological departments is 80%. Figure 9 presents
three simulations for three demographic scenarios.
The population aging will have a relatively large
effect on admissions to neurological wards. The
projected number of neurological beds in WR will
have to be increased by 8%−9%, according to all
three scenarios, to cover the desired level of annual
bed utilization. It means that at least 20 more
Figure 9: Projected number of neurological beds in WR to
cover the desired level of annual bed utilization according
to three scenarios.
SIMULTECH 2018 - 8th International Conference on Simulation and Modeling Methodologies, Technologies and Applications
464

neurological beds is required in 2030 compared to
2016. It should be noted that these forecasts do not
contain data about neurological patients older than
85+ who were treated on cardiology or geriatric
departments. The real needs are therefore even
greater than it is shown by our simulations and the
gap between predicted demand and the current supply
might be even more significant.
5 DISCUSSION AND
CONCLUSIONS
The findings of the present study indicate that
simulation approach is a powerful and effective tool
for modelling health service demand. It was proved to
be a useful predictive method when estimating an
overall demand stratified by diagnosis groups, and by
age-gender cohorts. Although, the contribution of
simulation to healthcare management is well known,
the potential for combining different simulation
techniques and using data from different sources
within one hybrid simulation model has not been
sufficiently emphasized. We have attempted to
demonstrate this by building the model to test the
impact of different demographic scenarios on overall
demand for healthcare services and on demand for
one type of hospital bed.
Our study shows a significant growth of WR
healthcare demand, especially in the oldest cohorts.
Additionally, the simulation experiments predicted
that population ageing alone increases the demand for
neurological beds during the next 15 years by about
8%−9%. This will put substantial pressure on the
Polish healthcare system.
Our approach is scalable and it could be used by
regional authorities to plan across the small
administrative unit or across the large area. Although
our estimates are based on the validated and best
available data, there are some limitations that we
would like to overcome in our future research. In
particular, the assumptions relating to the constancy
of demand indexes should be reconsidered.
ACKNOWLEDGEMENTS
This project was financed by the grant Simulation
modelling of the demand for healthcare services
from the National Science Centre, Poland,
which was awarded based on the decision
2015/17/B/HS4/00306.
REFERENCES
Aboagye−Sarfo, P., Mai, Q., Sanfilippo, F.M., and
Fatovich, D.M., 2016. "Impact of population ageing on
growing demand for emergency transportation to
emergency departments in Western Australia, 2005–
2020", Emergency Medicine Australasia, vol. 28, no. 5,
pp. 551-557.
Arisha, A. and Rashwan, W., 2016. "Modeling of
Healthcare Systems: Past, Current and Future Trends",
Proceedings of the 2016 Winter Simulation Conference,
eds. T.M.K. Roeder, P.I. Frazier, R. Szechtman, E.
Zhou, T. Huschka, and S.E. Chick. New Jersey: IEEE
Press, Piscataway, NJ, USA, pp. 1523.
Burkett, E., Martin-Khan, M. G., Scott, J., Samanta, M., and
Gray, L. C., 2017. "Trends and predicted trends in
presentations of older people to Australian emergency
departments: effects of demand growth, population
aging and climate change", Australian Health Review,
vol. 41, no. 3, pp. 246-253.
Chahal, K. and Eldabi, T., 2008. "Applicability of hybrid
simulation to different modes of governance in UK
healthcare", Proceedings of the 2008 Winter Simulation
Conference, eds. S.J. Mason, R.R. Hill, L. Mönch, O.
Rose, T. Jefferson, J. W. Fowler. New Jersey: IEEE
Press, Piscataway, NJ, USA, pp. 1469.
Chahal, K., Eldabi, T., and Young, T., 2013. "A conceptual
framework for hybrid system dynamics and discrete
event simulation for healthcare", Journal of Enterprise
Information Management, vol. 26, no. 1, pp. 50-74.
Cochran, J. K. and Bharti, A., 2006. "Stochastic bed
balancing of an obstetrics hospital", Health Care
Management Science, vol. 9, no. 1, pp. 31-45.
Eberlein, R.L. and Thompson, J.P., 2013. "Precise
modeling of aging populations", System Dynamics
Review, vol. 29, no. 2, pp. 87-101.
Forrester, J.W., 1968. "Industrial dynamics-after the first
decade", Management Science, vol. 14, no. 7, pp. 398-
415.
GUS 2017, (CSO) Główny Urząd Statystyczny. Available:
www.stat.gov.pl [2018, March].
Harper, P. R. and Shahani, A. K., 2002. "Modelling for the
planning and management of bed capacities in
hospitals", The Journal of the Operational Research
Society, vol. 53, no. 1, pp. 11-18.
Harrison, G. W., Shafer, A. and Mackay, M., 2005.
"Modelling Variability in Hospital Bed Occupancy",
Health Care Management Science, vol. 8, no. 4, pp.
325-34.
Mielczarek, B., 2016. "Review of Modelling Approaches
for Healthcare Simulation", Operations Research and
Decisions, vol. 26, no. 1, pp. 55-72.
Mielczarek, B. and Zabawa, J., 2018. "Modelling
Population Dynamics Using a Hybrid Simulation
Approach: Application to Healthcare", Simulation and
Modeling Methodologies, eds. M.S. Obaidat, T. Ören
and Y. Merkuryev. Springer International Publishing,
Cham, Technologies and Applications, pp. 241.
Ministry of Health, 2018. Mapy Potrzeb Zdrowotnych (in
Polish,
Maps of Health Needs).
Impact of Population Ageing on Hospital Demand
465

Mustafee, N., Powell, J., Brailsford, S.C., Diallo, S.,
Padilla, J., and Tolk, A., 2015. "Hybrid Simulation
Studies and Hybrid Simulation Systems: Definitions,
Challenges, and Benefits", Proceedings of the 2015
Winter Simulation Conference, eds. L. Yilmaz, W.K.V.
Chan, I. Moon, T. M. K. Roeder, C. Macal, and M. D.
Rossetti. New Jersey: IEEE Press, Piscataway, NJ,
USA, pp. 1678-1692.
Nentwich, L.M. and Grimmnitz, B., 2016. "Neurologic
Emergencies in the Elderly". Emergency Medicine
Clinics of North America, vol. 34, no. 3, pp. 575-599.
Strunk, B. C., Ginsburg, P. B., and Banker, M. I., 2006.
"The Effect of Population Aging on Future Hospital
Demand", Health affairs, vol. 25, pp. W149.
Vrhovec, J. and Tajnikar, M., 2016. "Population ageing and
healthcare demand: The case of Slovenia", Health
Policy, vol. 120, no. 11, pp. 1329-1336.
Waligórska, M., Kostrzewa, Z., Potyra, M., and
Rutkowska, L., 2014. "Population projection 2014-
2050", CSO, Demographic Surveys and Labour Market
Department.
SIMULTECH 2018 - 8th International Conference on Simulation and Modeling Methodologies, Technologies and Applications
466
