
3D-printing: A Future “Magic Wand” for Global Manufacturing
How Can We Benefit from It Today for Sports and Health Care?
Andrey Koptyug, Mikael Bäckström, Lars-Erik Rännar
Sports Tech Research Centre, Mid Sweden University, Östersund, Sweden
Keywords: Additive Manufacturing, Sports Technology, Active Lifestyle, Research and Development, Education.
Abstract: 3D-printing, or as it is also known, additive manufacturing (AM), is promising to be one of the determining
manufacturing technologies of the present century. It is not a single technology but a family of rather
different ones common in the way components are made, adding materials layer by layer. Additive
manufacturing is already quite competitive to existing and well established technologies, but it also can
provide unprecedented flexibility and complexity of shapes making components from the materials as
different as cheese, chocolate and cream, live cells, concrete, polymers and metal. Many more materials we
were not even thinking about few years ago are also becoming available in additive manufacturing, making
it really believable that “only the sky is the limit”. During the time available for the keynote lecture, we will
analyze the present position of AM in relation to other technologies, the features that make it so promising
and its influence upon the part of our life we call sports and health, using the examples relevant to the
Congress areas from computer systems to sports performance. Out of all enormities of materials available
for different representatives of this manufacturing family we will concentrate at polymers and metals. AM
technologies working with these two material families are already providing some unique solutions within
the application areas relevant to the Congress' scope. We will also talk about some limitations inherent to
the AM in polymers and metals to have the awareness that though the limit is somewhere “high in the sky”,
it still exists.
1 INTRODUCTION
Additive Manufacturing (AM) is a proper term
describing technologies that build objects by adding
layer-upon-layer of material (Christensen et al,
2007). 3D printing, the name commonly used in
everyday life, is in fact only one of the technology
types in this family, and many other AM
technologies can hardly be referred to as “printing”.
Materials used in modern additive manufacturing
can range from concrete, rubbers to polymers,
metals, cheese, cream and chocolate. In the big
family of additive manufacturing different
technologies have different levels of “maturity”.
AM in polymers and metals (alloys) represent most
mature methods that already compete with many
other, well established technologies especially in
manufacturing small series or unique products.
Competitive advantages of these methods include
the ability of building components with extremely
complex shapes in a single technological process,
fast design-to-market times, high energy and
material efficiency (Koptyug et al, 2017,
Nanotechnology). Along with materials common
with other technologies additive manufacturing in
metallic materials and polymers introduce new
materials not available for other technologies (e.g.
Koptyug et al, 2013 AM Conf., Pauly et al, 2013),
utilizing unique inherent properties of used
processes. Wide applications of modern computer
and virtual reality technology integrated into “the
design for AM” process allow for unique versatility
in functionalization, individualization and
modification of the manufactured components
almost without increasing production costs. Current
paper presents some of the experiences in integrating
additive manufacturing into the education, research
and development within healthcare, sports and active
lifestyle technology- related applications from
Sports Tech Research Centre at Mid Sweden
University.
Koptyug A., BÃd’ckstrÃ˝um M. and RÃd’nnar L.
3D-printing: A Future â
˘
AIJMagic Wandâ
˘
A
˙
I for Global Manufacturing - How Can We Benefit from It Today for Sports and Health Care?.
DOI: 10.5220/0006810300010001
In Proceedings of the 5th International Congress on Sport Sciences Research and Technology Support (icSPORTS 2017), pages 5-16
ISBN: 978-989-758-269-1
Copyright
c
2017 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
2 MATERIALS AND METHODS
A set of additive manufacturing machines is
stationed at Sports Tech Research Centre, including
one high-end device working with metals and alloys,
two high-end industrial class polymer machines, and
five table-top polymer ones. Table-top polymer
machines are mainly used in education within the
BSc and MSc engineering courses related to modern
design and manufacturing, and graduate exam
projects (Bäckström et al, 2013). High end machines
are used both for research and development, and as
the means of manufacturing of unique parts and
components. Majority of the described examples
relate to the components and parts manufactured
using these machines.
For additive manufacturing in metals and alloys
we use an ARCAM A2 Electron Beam Melting
machine by ARCAM AB (Mölndal, Sweden).
Electron Beam Melting is a powder bed fusion
additive manufacturing method, where successive
layers of metal powder are melted together with a
high power scanning electron beam (Sames et al,
2016, Koptyug et al, 2017, MSF). The process takes
place in a vacuum chamber at high temperatures.
Powder is brought to the working zone forming a
thin layer (commonly 50 to 90 micron- thick). High
intensity electron beam melts the area corresponding
to solid sections at present component height.
Working table is lowered one step (thickness of one
production layer), powder is brushed over the
working area again, and the process of next layer
processing is carried out. More details about the
process stages can be found elsewhere (Sames et al,
2016, Koptyug et al, 2017, MSF). Currently we
mainly work with the titanium alloy Ti6Al4V
(Koptyug et al, 2017, Cronskär et al, 2012, Koptyug
et al, 2013, LSMR), an alloy well known to medical,
aerospace and automotive industry and common to
many powder-bed AM methods, and at introducing
new materials earlier not used in AM (Koptyug et al,
2013, AM Conf., Zhong et al, 2017).
High-end additive manufacturing in polymers is
represented by fused deposition modelling (FDM)
machine Stratasys uPrint and PolyJet machine
EDEN260V, both by Stratasys Ltd (Stratasys Ltd,
2017). FDM machine uses a thin filament made of a
thermoplastic polymer, which is melted and
extruded in thin adjacent “wires” forming
manufactured component layer by layer. It can make
components up to 203 x 203 x 152 mm in size with
the resolution about 0.1 mm. PolyJet machine
operates in a way similar to an old bubble-let printer,
only instead of liquid ink it uses monomers
depositing them layer and curing it by a UV-lamp. It
can make components up to 255 x 252 x 200 mm,
and its precision is given in dpi, as for the true
printer: 600 dpi in the layer plan and 1200 dpi in the
build direction. It means that in the high resolution
mode its precision is about 16 micron. And when the
FDM machines are rather limited to the type of
materials (relatively stiff thermoplastic polymers)
PolyJet ones have much wider choice, from softer
rubber-like to relatively hard polymers, transparent
or having different colours. Table-top polymer
machines MakerBot Replicator (Makerbot LLC,
2017) are also of the FDM type. Though sizes of
components it can manufacture and precision are not
as impressive as for the high-end machines, these are
easy to use and interface. These machines are mainly
used for prototyping, and mainly for education. It
should be noted here, that with manufacturing of
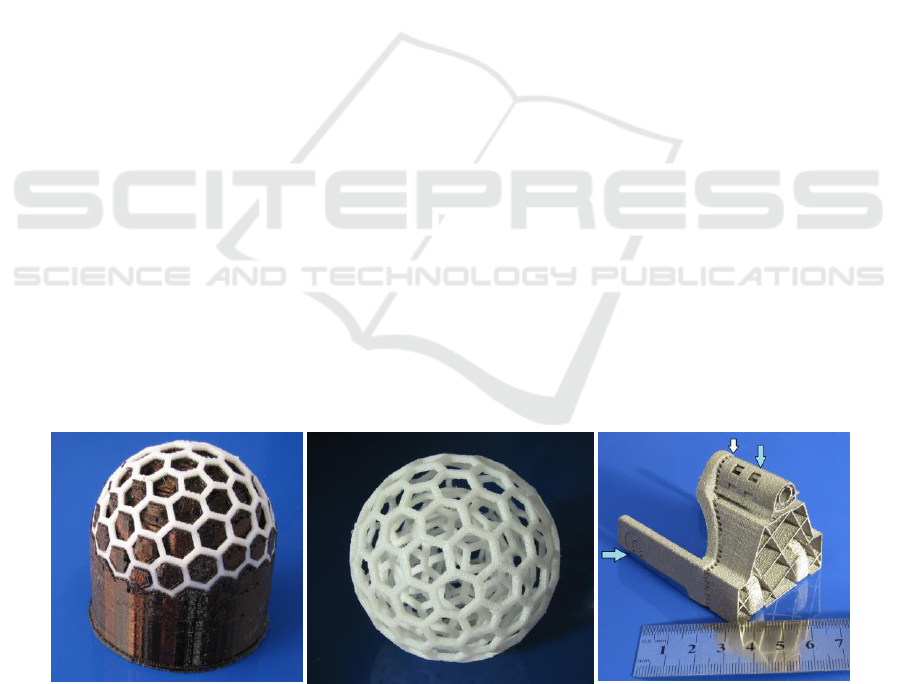
(a)
(b)
(c)
Figure 1: Complex shape components manufactured from ABS polymer in the FDM machine (a, b), and from Ti6Al4V in
the EBM machine (c). Polymer component is shown as it comes out from the machine, when support material covers
essentially all voids (a), and after support removal in the ultrasonic bath (b). Ti6Al4V component (c) is shown after removal
of the surrounding working powder. Arrows mark the position of the wafer supports, and perforated support boundary
where it will be broken off during post-processing.

complex shapes with overhanging features it is not
possible to avoid using supporting elements in the
manufactured component. In case of polymer
machines a second, “support” polymer is used,
commonly removable by water or special water
solutions. In the case of metal machines supports
take shape of wafer-thin elements, which are
mechanically removed in post-processing. Figure 1a
presents an examples of a “ball-in-ball”
manufactured from ABS polymer in the FDM
machine (a, b), and a component manufactured from
Ti6Al4V in ARCAM A2 machine (c). With the
polymer part (Fig. 1 a, b) working material is white
and support material is dark. With the metallic parts
supports are made in the same material. In Fig 1(c)
blue arrows show the positions of the support
wafers, and white arrow marks the perforated
boundary of the supports, along which they will be
broken off in post-processing. It is also clear, that
one of the restrictions in “design for AM” for these
types of machines. If we leave closed voids inside
the components, they will be filled with a support
polymer, or working powder, as it is possible to
remove support materials in post-processing only
through openings and channels.
3 AM IN HEALTHCARE
There are some application areas that already
strongly benefit from actively using additive
manufacturing. Industry is commonly the first to be
mentioned, but areas related medicine, health care,
and rehabilitation are also among clear beneficiaries
(Koptyug et al, 2013, 2017). High competitiveness
of the sport activities and certain risks inherent to
active lifestyle can unfortunately result in injuries.
Injury prevention is of course one of the best
strategies to go for and some contributions of
additive manufacturing to preventive strategies will
be discussed later in this paper. In present chapter it
will be discussed what AM can do for the medical
treatment and rehabilitation.
3.1 Biomedical Implants
Orthopaedics and reconstructive surgery is already
recognizing the advantages of additive
manufacturing. While some other medical
disciplines start discussing future possibilities of the
medical treatment individualization, orthopaedics
and reconstructive surgery already practice it with
the help of additive manufacturing. Today it is
possible to go all the way from medical image to
individualized implants placed into the human body
using design and manufacturing methods developed
for or within AM technologies (Cronskär et al, 2008,
2012, 2013, Koptyug et al, 2013, LSMR). Today the
advanced path from the results of medical scan to
individualized implant looks as follows. During the
first stage a standard image set acquired form
medical 3D imager is transformed to the format that
can be used by engineering and design software.
Next, special software is used to “filter out”
unnecessary features. In the case of designing
individualized metallic implant or fixation plate for
the broken bone one needs to “filter out” all soft
tissues and cartilage from the original image, leaving
only the bone outlines. Though it is not a trivial
operation, number of commercial software packages
capable of doing it is already available. Result of
these operations is an exact computer 3D model of
the bone, with all defects and brakes. From this point
the path splits. “In real world”, a replica of the
broken bone is additively manufactured using a
computer bone model (Fig. 2 a). “In virtual world”,
broken bone is mended using mirrored image of the
symmetrical healthy bone as a template, with all
bone fragments that are to be saved in the exact
places. Next, perfectly fit individualized implant
with screw hole positions and all other demanded
details is designed (Koptyug et al, 2013, LSMR,
Cronskär et al, 2008, 2012, 2013). It should be
noted, that today “virtual world” line does not end
with the shape optimization of the implants. Using
advanced body modelling software packages one
can calculate the values and directions of the forces
applied to the bone by attached ligaments in a
chosen scenario (Fig. 2 b, from Cronskär, 2014).
And it is possible to model and calculate
corresponding stress fields in both the broken bone
and implant attached to it. And implant design now
can be adjusted and optimized for the chosen
functionality (lowest weight with given loading
capacity, minimum thickness with excessive
strength etc., Cronskär, 2014, Cronskär et al, 2013).
Effectively, this is a process combining advanced
shape and function-optimized design and “virtual
surgery” of the broken bone mending. Now the
implant itself is ready to enter the real world, and it
is manufactured in one of the metal AM machines.
At this point a preoperative model of broken bone
“meets” matching metallic implant, both
components additively manufactured in polymer and
metal respectively (Fig. 2c). To speed up a pre-
operative process in complex cases additional model
of the implant can also manufactured in polymer,
allowing surgeons to practice even before the
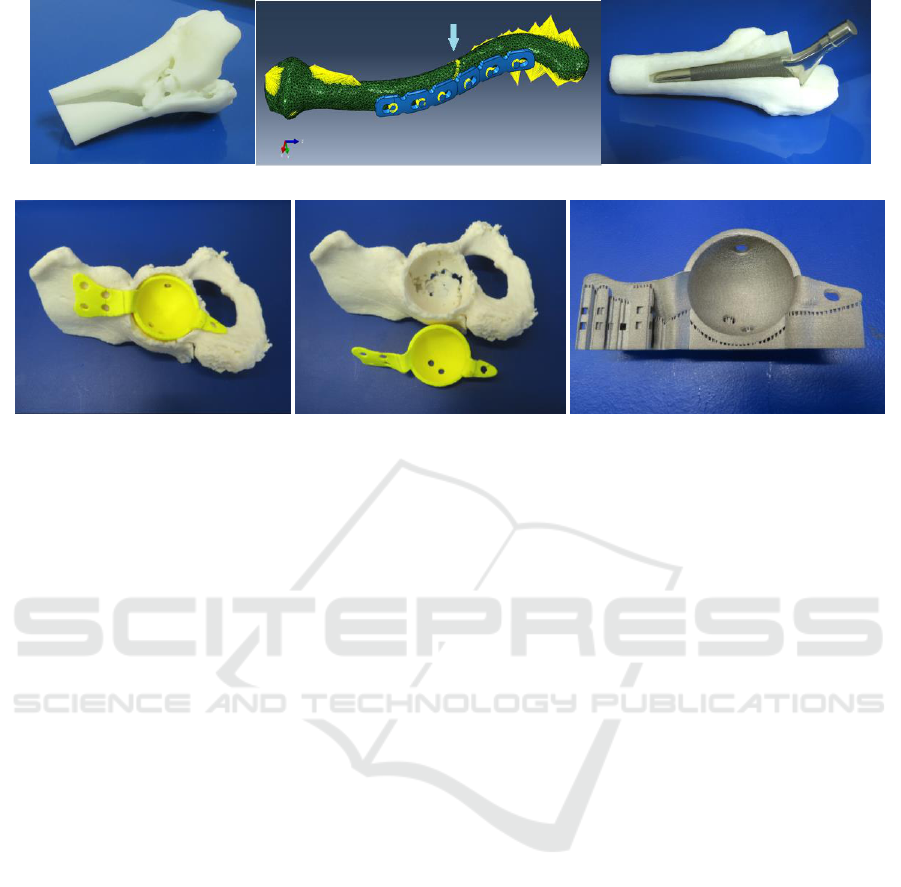
(a)
(b)
(c)
(d)
(e)
(f)
Figure 2: (a) Actual size pre-operative model of the broken bone manufactured from the ABS polymer basing on the
medical image of the patient’s bone. (b) Computer model of the broken collarbone (clavicle) with a fixation plate attached.
Arrow marks the brake position; yellow lines indicate directions and values of forces applied to the bone by attached
ligaments. (c) Actual size ABS model of the thigh bone (femur) section showing the position of the individualized
Ti6Al4V implant designed for the hip replacement surgery. (d, e) Actual size models of the human pelvis section and of a
customized implant used in pre-operative planning; (f) corresponding implant made in EBM machine from Ti6Al4V with
support structures still present. All given examples are from the medical case studies.
metallic implant is made. Figure 2 (e-f) illustrates a
case for the hip replacement operation planning with
the help of additive manufacturing in the case when
pelvic bones are osteoporotic and acetabular cups
with standard fixation cannot be applied. In such
case individualized acetabular cup integrating
fixation elements with the screw holes
corresponding to parts of the pelvis where the bone
is still strong enough is designed and manufactured.
Figure 3(f) shows such cup as it comes after working
powder is removed, but with the support structures
still attached (positioned as it would be oriented in
manufacturing).
Described path allowing “transitions” between
virtual world of computer models and real one can
be extended even further, for example towards
manufacturing individualized surgical support tools.
Using computer models of the bones one can
manufacture saw guides for fast and precise removal
of the damaged bone sections, and screw guides,
allowing putting screws in exact places with precise
orientation. As a result, modern surgeon can obtain a
package of parts including a pre-operative bone
models, optimized in shape and functionality
implants and surgery support tools. And even before
the patient goes to the operation theatre surgeons can
perform a full-scale “dummy surgery” using actual
size plastic bone models, individualized saw guides
and implants- cutting, drilling and putting screws in
place. Such preparation and availability of the
individualized implants can significantly shorten the
operation time and cost, and improve the procedure
outcomes for the patients (Koptyug et al, 2013,
Cronskär et al, 2008, 2012, 2013). Realizing market
opportunities polymer AM machine manufacturers
are now introducing the materials that can be
sterilized and taken directly into the operation
theatre.
Discussions about the benefits of additive
manufacturing for biomedicine always involve
delivery time and cost related issues. It appears that
today design of the individualized implants takes
most of the image-to-product time, and it should be
done in tight cooperation between AM-able
designers and practicing doctors. Polymer pre-
operational models and metallic implants also need
certain time to be manufactured, quality controlled
and properly prepared for transferring to the hospital
environment. Our experience shows that with the
availability of proper resources, image-to-model
times can be as short as 48-72 hours, and image-to-
implant path can take less than 5-7 days (depending
upon the complexity of the implants needed). Our
best achievement was a lead time of 48 hours from
receiving a medical image to the delivery of the
finished implant. With the complex surgical

procedures, where application of the individualized
implants is effective, surgery preparation also takes
time of at least about one-two weeks. Speaking of
the costs, one needs to think of them even in the
cases when individualized implants make a
difference for patient between permanent disability
and relatively normal life for a number of years.
Comparisons of the costs associated with the
additive manufacturing of individualized implants
indicate that they are at least 30-40% cheaper than
individualized implants manufactured using other
technologies (Cronskär et al, 2013), and with
increasing numbers of manufacturing sites capable
of AM this ratio continues to improve. As compared
to the “standardized” implants used in complex
surgical cases additively manufactured implants are
as such more costly. But when the reduction of
surgery time is counted for, overall hospital costs are
either on par or, in many cases, is significantly lower
when using AM implants. Of course it would be
hard for AM implants to compete in cost with
relatively simple, mass-produced items. Thus at
present highest value AM implants usage will bring
in special surgical cases (complex fractures,
osteoporotic bone cases, complex reconstructive
procedures etc.).
Implant manufacturing is among the most
challenging for additive manufacturing. Along with
the issues common with almost all other technology
and engineering applications of AM like: providing
good value for money and acceptable costs,
adequate design-to-market times, exact replication
of the designed shape at the output, securing
mechanical strength, fatigue and corrosion
resistance, biomedical applications impose
additional ones (Koptyug et al, 2012, 2014, 2017,
Nanotechnology). Majority of these additional
demands are related to biocompatibility of the
implant material, its biointegration and longevity in
the human body. For example, corrosion resistance
in technology mainly presumes that component
should not lose its mechanical properties. But even
relatively small amount of ions “leaking” from the
metallic implant into the body may be harmful.
Also, because molten metal in powder- bed AM
methods is surrounded by the working powder,
component outer surfaces are always coming “as
manufactured” rough to some extent and can contain
loosely attached powder grains. Some technological
applications demand much better surface finish and
thus certain post-processing is performed. In ideal
case surface topography control of biomedical
implants should cover the feature dimensions from
nanometres (determining wet ability and water
contact angle important for the earliest stages of
implant integration with cell attachment to the
surface) through micrometers (important at later
stages with cell migration and differentiation) to
millimetres (providing vascularisation and bone
ingrowths for better implant stability; Koptyug et al,
2012, 2014, 2017, Nanotechnology). Such control is
not possible within existing additive manufacturing
processes, and even needed post-processing often
becomes hardly possible. Loosely connected surface
powder grains may potentially become loose during
service life, and thus should be secured or removed.
For solving these issues research and development
work is carried out across the world. Such work is
aiming for example at improving AM processes in
cases when components have solid and lattice
sections, which can be additively manufactured in a
single additive process. Such structures are
important both for the implants (mimicking cortical
bone structures) and for industrial applications (3D
lattices in filters and catalyst carriers, in lightweight
construction elements- integrated with solid
component sections). Also significant efforts are
directed to introducing better biocompatible
materials for AM (Koptyug et al, 2014, 2017,
Nanotechnology), and better methods for metallic
implant surface coating (Surmenev et al, 2014,
Surmeneva et al 2015, Chudinova et al, 2016).
Yet more problems are coming from the fact that
solid implants used to fix and support broken or
weak bones are much stronger than bone tissue. This
often results in the situation when additional stress
appears in the bone sections adjacent to the implant?
For example, when solid titanium rod of the hip
stem implant is sitting inside the osteoporotic thigh
bone (femur) after hip replacement surgery, upper
part of the bone up to the joint is than well protected
from extra loads. But the area, where the “rod” ends
will be under considerable stress, if the patients
occasionally falls in a wrong way, and secondary
brake in this position is quite probable. Differences
in the mechanical properties of the metallic implants
and bones can also lead to the loosening of the
implant in the body after some time, either due to
damaging surrounding bone, or to so-called “stress
shielding”, when bone tissue adjacent to the implant
starts to “dissolve” (Huiskes et al, 1992, Summer,
2015, Koptyug et al, 2014). Today two possible
ways of solving this problem are dominating
research activities: development of new metallic
materials with the mechanical properties closer to
the ones of natural bone (e.g. Niinomi et al, 2011),
and application of the implant sections that are
porous or made of three-dimensional lightweight

constructions (lattices; Heinl et al, 2008, Murr et al,
2010, Koptyug et al, 2012, 2014). But one should
admit that no optimal solution is yet available for the
everyday medical practice.
Though limitations of additive manufacturing in
supporting treatment of broken bones exist, related
progress in practical surgery related to AM
implementation is quite significant allowing one to
speak about introducing “spare parts for human
body” (Bäckström et al, 2012, Zadpoor et al, 2017).
Though such spare parts are not yet ideal and cannot
completely substitute natural bones, they still help to
return to activities and save lives.
3.1 Rehabilitation and Protection
Additively manufactured components significantly
broaden the possibilities in supporting active patient
rehabilitation after illness or injury. Individually fit
protection, fixation and support devices can be
manufactured for example with the help of additive
manufacturing (e.g. Bibb et al, 2014, Palousek et al,
2014, Mills, 2015, Ganesan et al, 2016). Availability
of the inexpensive, often hand-held digital scanners,
availability of affordable and the emergence of free
digital design software, and wide availability of both
professional and table-top “3D printers” working
with polymers boost public access to the
individualized rehabilitation and protection devices.
Because the extreme precision of digital scanning
and manufacturing in many protection devices is
often not needed, it allows keeping their cost
relatively low
It should be noted, that as with many other
additively manufactured components, production of
such devices is not the most expensive stage, and
dominating costs commonly lay with the design
process. This difference is quite pronounced with the
applications of additive manufacturing in prosthetics
(e.g. Jina et al, 2015, Skoglund, 2015). In many
cases individualized prosthetic device is the only
option for having active lifestyle and participation in
sports. As compared to many temporary protection
devices prostheses should be designed for individual
fit baring in mind their functionality, comfort,
possible excessive loads and fatigue during service.
And because in additive manufacturing cost is
mainly associated with amount of used material and
processing time rather than component complexity
(“complexity comes for free”, Fera, 2016),
prosthetic devices now can afford elements of the
artistic design. Figure 3 (a-c) illustrates the process
of an individualized prosthetic socket design and
manufacturing (Skoglund, 2015). Digital model is
designed basing on the individual scan (Fig 3 a) and
is “virtually tested” in realistic loading conditions
(Fig. 3b presents the deformation field in the
Ti6Al4V socket during loading with clamped
fixation element- small pyramid in the bottom of the
socket). Sports Tech Research Centre logotype
(stylized letter S) is incorporated into the socket to
illustrate possibilities of artistic touch to the
individualized prosthetic devices.
Today functional prosthetic devices and
individualized equipment are becoming available
and are actively used by many Para-athletes (e.g.
Pallis, 2003, Technology for Disability Sport, 2016).
For many of them only such devices allow them to
compete. Figure 3(d) presents the low leg prosthetic
device successfully used in training and
competitions by Swedish Nordic skier Helene Ripa
(Helene Ripa, 2017). It has relatively simple
(a)
(b)
(c)
(d)
Figure 3: 3D design model for the manufacturing of the individualized prosthetic socket for a knee amputee (a), computed
deformation field during its loading (b) and final component manufactured using EBM technology in Ti6Al4V (c); lower
leg functional prosthesis for the Nordic skier (e).

mechanical construction and incorporates bicycle air
type adjustable shock absorber with some parts in
this first prototype made in Ti6Al4V using EBM
additive manufacturing. According to Helen, this
device allows for the leg movements much closer to
what she has had before the injury. So the engineers
have done a good technical job, but at the time were
lacking the knowledge on the rules and regulations
for competitions by the International Paralympics
Committee (IPC). According to these rules (see IPC
rules for Nordic Skiing) devices like the one shown
in Fig. 3(d) that are directly connected to the ski
bindings are not allowed in the IPC competitions,
the ski shoe must be always present. So the device
was re-designed and manufactured using simpler
and off-shelf components.
4 INJURY PREVENTION
Additive manufacturing is not only actively helping
with medical treatment and rehabilitation, but
becomes an important tool in injury-prevention
research. It is quite important to understand how
injuries happen in order to prevent them. We realize
that the most important part of the scientific method
is the experiment. But experiments leading to
injuries are belonging to a nightmare scenario. Thus
in many cases the only experimental evidence
available for scientists would be the unfortunate
results of an injury or trauma. Modern science has
certain tools that can be used for reconstructing the
events. Mainly this is done using computer-based
modelling. In modern days such modelling often
involves what we call “virtual reality”, allowing to
“perform experiments” that could be dangerous in
real world (or expensive, or lengthy in time, or under
conditions which never exist in real world). Typical
examples of this approach are related to designing
safety devices protecting human body parts from
injuries resulting from the falls or collisions. Modern
medical equipment is capable of producing detailed
scans (high spatial resolution and specificity to the
type of the tissues) of the body parts. Basing on such
scans computer models of corresponding bones, or
of the whole body parts, are made. In case of
damaged body parts it is possible to make virtual
reconstruction of their “intact” state, and model the
conditions that will cause damage we registered
experimentally. One can also generate models of the
body parts together with safety devices and perform
multiple “virtual experiments” assessing the
efficiency of the protection.
Among various devices protecting us in sports
and other activities with the help of mathematical
modelling and additive manufacturing one can find
the ones designed to protect our legs (e.g. Emerson
et al, 2011, 2013), wrists (e.g. Pain et al, 2013, 2015,
Adams, 2016) and heads (Kleiven, 2002, 2006,
Petrone et al, 2010, Samaka et al, 2013, Taha et al,
2013, Smith et al, 2015, Awad et al, 2015, Hassan et
al, 2015, Antona-Makoshi, 2016, Koptyug et al,
2017). But although significant advances are reached
in mathematical modelling there are certain issues
related to it. First of all, any model is to some extent
simplifying the reality. It is both strength of the
modelling process, but in some cases it may be a
weakness: too many details can mask certain key
features; too little details- and we can miss or
misinterpret significant ones. Another problem is
that modelling demands exact input parameters,
which we often either do not know exactly or they
are changing depending on some conditions. For
example, in typical cases of discussed modelling
mechanical properties of human tissues are needed.
Unfortunately, some of these are not known at all,
some are hard to measure, some are nonlinear and
their values depend on multiple parameters. On the
top of that, mathematical models for such objects as
body parts are extremely complex, and in many
cases there is no guarantee that they are actually
correct. Depending on the models one cannot
experimentally test in designing safety equipment is
at least questionable, and here physical modelling is
coming into play. For example, one can model
animal bones mathematically, and perform
laboratory experiments breaking them. By
comparing the results one can adjust the models
making them better (Taha et al, 2013, Awad et al,
2015, Hassan et al, 2015, Koptyug et al, 2017). But
the problem of not exactly known (or dynamically
changing) input parameters still to some extent will
remain with such tests. Situation changes if we can
make “surrogate” body parts made of the synthetic
materials with known properties (with the
parameters “close to the ones of originals”) basing
on the exact geometry retrieved from the real scans
(Payne et al, 2013, Awad et al, 2015, Adams et al,
2016, Koptyug et al, 2017). Additive manufacturing
today easily produces the real size “surrogates” of
the bones replicating them in high precision. It can
also produce various moulds used for casting and
exact replication of the softer tissue shapes. Thus
quite complex realistic physical models of the body
parts are becoming available today. We can use such
surrogates in experiments, comparing the results to
the ones from mathematical modelling. Obviously, it
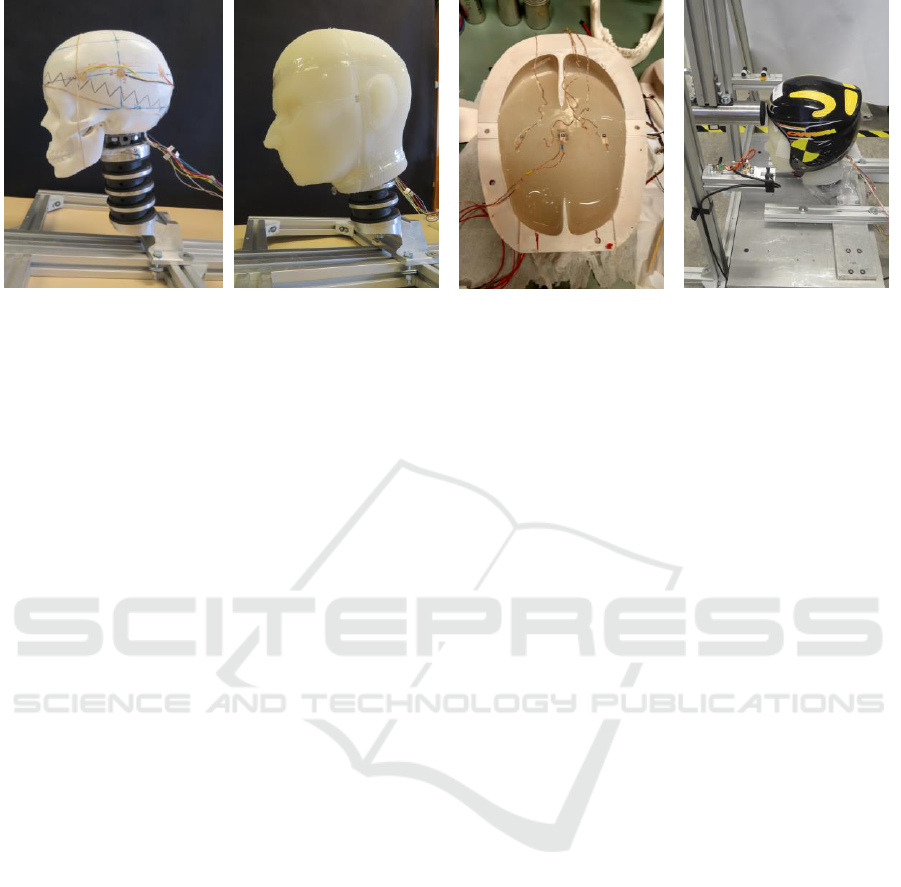
(a)
(b)
(c)
(d)
Figure 4: Surrogate human head with embedded sensors for studying dynamics of the collisions: assembled head on the
hybrid III neck without (a) and with (b) the “soft tissue” in place; mould with partly cast surrogate brain showing sensors
placed in the plane coming through CG point (c); head-neck assembly in the helmet mounted on the impact rig.
is safe to “abuse” surrogate body parts without any
risk to humans. Also, the input parameters for
mathematical modelling will be now exactly known
(or directly measured); geometry will follow actual
body parts and will be exactly transferred into the
model, allowing validating and adjusting our models
and modelling approaches.
Modelling in head injury prevention is used in
similar way (Awad et al, 2015, Koptyug et al, 2017).
Significant improvements in the protection helmet
design are already in place as a direct result of better
understanding how certain impacts can affect the
brain. For example, patented MIPS technology
(MIPS AB, 2017) already implemented in many
helmets, allows to additionally protecting from the
non-central impacts leading to the rotational motions
of the brain and its parts in the cranium and
consequent damage to the axons. But physical
modelling in this research helps to go one step
further. Subjecting the surrogate body parts to
excessive loading and monitoring at the results of
the “injuries” does not bring the full understanding
on how the damage have happened. Embedding
multiple sensors into such surrogates and
reconstructing the dynamics of the events during
surrogate head impacts brings more precise
information (Taha et al, 2013, Awad et al, 2015,
Hassan et al, 2015, Koptyug et al, 2017). Now it also
becomes possible to correlate the values measured
by wearable sensors placed outside the “head” to
what is happening inside it, adding more validity
tothe empirical criteria used by multiple monitoring
devices used in modern sports and training.
An advanced head surrogate with multiple
embed sensors is developed at Mid Sweden
University for studying concussion mechanisms and
ways of better head protection (Fig. 4). It consists of
the anatomically correct scull additively
manufactured from the ABS polymer (Fig. 4a)
surrounded by the surrogate tissue, made from
silicone rubber in additively manufactured mould
(Fig. 4b). Scull hosts a surrogate brain, made from
soft silicone rubber cast in additively manufactured
mould. Scull with the brain inside is filled with
silicone oil, a surrogate of cerebral fluid. Scull,
tissue and brain surrogates were designed basing on
medical 3D scans. Surrogate brain was made in
sequential steps, allowing sensor embedding at
specific positions (Fig. 3c). Two three-axial
accelerometer chips are embedded in the top part of
the brain lobes, three- in the plane coming through
the centre of gravity (CG) plane of the brain (Fig.
4c), and three- in the medial plane of the cerebellum
(“small brain”). Additional three-axis gyroscope
chip is positioned at the CG point, to monitor the
motion of the brain surrogate together with
acceleration sensors. Seven pressure sensors are
placed across the scull at different positions to
monitor changes in the surrogate cerebral fluid
during the impact. Materials were selected to have
properties as close as possible to the “natural” parts
of human anatomy.
Preliminary impact tests carried out using home-
made pendulum type rig (Fig. 3c) indicate that
chosen sensors allow monitoring relative brain
motion in the cranium under impact with a
millisecond time resolution, and pressure sensors
can simultaneously monitor the dynamics of the
cerebral fluid pressure at different locations. Large
amount of data acquired in these experiments is still
analyzed, but qualitative analysis already confirms
that significant rotational motion of the brain as a
whole caused by non-central impacts to the head can
cause significant strain in the axons of the brain

stem. Non-central impacts to the head or head
protection can also cause different movements of the
brain lobes, and rotation of the cerebellum, which
also can present certain danger for brain tissue
damage. At the moment new improved version of
the surrogate head model is under development.
5 TECHNOLOGY
Within the diversity of additive manufacturing
applications for sports and active lifestyle we will
only discuss two examples related to the prototyping
and manufacturing of experimental equipment. It is
clear, that such advantages of the AM and design for
AM as ease of construction alterations, “virtual
tests” of mechanical properties and functionality,
possibility of cost-effective manufacturing polymer
and metallic components of extremely complex
shapes not available with other manufacturing
methods, brings significant benefits for research and
development work in multiple application areas.
Extra dimension is added here by the possibilities of
designing construction elements with embedded
sensors (strain gauges, force and pressure sensors,
accelerometers, gyros etc.) purpose-designed or
substituting original elements of the existing
construction.
Prototyping is a major part of experimental
development of the devices and components based
on new ideas. It is also a critical stage of product
development process in industry. Flexibility, fast
manufacturing of test components implementing
design changes with relatively low cost processes
makes additive manufacturing an ideal support tool
for innovative development. One of the examples
demonstrating such process in action is the
development of novel ski pole handles done initially
as a project within the Mid Sweden University
research environment and later turned into
successful commercial product (Kuzmin Ski
Technology AB, 2017). Measurements performed
during the World Cup biathlon event held in
Östersund indicated that one of the factors slowing
the athlete’s progress through the race is excessive
time spent for taking off ski poles at the shooting
station and putting them back on again. So ideas for
the new ski pole handles for better grip and faster
mounting-dismounting were put forward. Tens of
prototypes in ABS polymer were designed,
additively manufactured and tested in the lab and in
the field. Final design (Fig. 5a-c) incorporates few
innovations, including the pen-like clip on the ski
pole handle and added loop on the inner side of the
glove for fast “connection”, and better positioning of
the thumb over the ski pole top providing better grip
and power transfer in active poling.
Another typical example is development of the
new roller ski design, initially done as a part of the
research project and later turned into a patented
(a)
(b)
(c)
(d)
(e)
Figure 5: Novel design of a ski pole handle: (a) additional loop added to the glove, (b) pencil-like clip is inserted into the
glove loop, (c) thump positioning on the pole handle support element; novel roller ski design: (d) test version with
embedded load cells (d, top) and final version (d, bottom), friction mechanism with slip adjustment (e).

product (Tinnsten et al, 2010, Ainegren et al, 2012,
2013). Many of active skiers complained that
training in summer using roller skis presumes very
different patterns of motion and leg muscle activity
as compared to training in winter (Ainegren et al,
2012, 2013). Cross country skis used in winter have
a camber: free gliding happens with only front and
rear of the ski running surface having the contact
with the snow, and these parts of the ski are covered
with so-called “gliding wax”. To push back in
classic style skiing athlete needs to load the skis
forcing the central part covered with the “grip wax”
getting in contact with the snow. To push back with
traditional roller ski having a ratchet mechanism on
the rollers one only needs backward sliding motion.
Also, with the “winter skis” pushback action
happens with partial slipping depending on the
loading pressure, particular wax type, snow
conditions, ambient temperature and humidity etc.
With the ratcheted roller skis there is almost no
pushback slipping, as the friction between the rubber
roller and road surface is quite high. Two types of
prototype roller skis were manufactured using AM
technology: research ones with embedded load cells
for measurement forces involved, and the ones with
pushback slip action (Fig 5 d-f). New roller skis also
need to be loaded like the “winter” for pushing back,
and the pushback friction (extent of slipping) can
also be adjusted. Extensive tests performed in the
laboratory conditions and in the field indicate that
roller skis of new design much better represent
winter skiing, and feedback given by athletes using
them is very positive.
6 SOME CONCLUSIONS
Some conclusions can already be drawn from our
experiences of using additive manufacturing in
education and research related to sports technology
and active lifestyle. Additive manufacturing can be
successfully used as one of the powerful support
tools enabling the applications not available before,
speeding up development processes in many
different application areas, and even saving lives.
Possibility to utilize significant competitive
advantages of modern AM strongly depend on the
knowledge of corresponding technologies, their
strong points and limitations, and on practice of
designing for AM. Thus incorporating additive
manufacturing into the study programs for all
engineering specialists, including the ones
specializing in sports and active lifestyle related
subjects is quite important. Involvement with
additive manufacturing also helps specialists to be
more innovative, to rethink old design paradigms in
a novel way, to develop new research setups and
methodologies and to design new products. We
believe that the penetration of additive
manufacturing into applications related to sports
technology and active lifestyle will dramatically
increase in the years to come.
ACKNOWLEDGEMENTS
Authors acknowledge the efforts of all people from
Sports Tech Research Centre: without their active
contribution many of the results described in the
paper would not be possible. We also acknowledge
the financial support from Mid Sweden University,
Östersund Municipality, Region Jamtland-
Herjedalen, Swedish Innovation Agency (Vinnova),
Swedish Agency for Economic and Regional
Growth (Tillväxtverket) and Rolf and Gunilla
Enström Foundation for Research and Development
for their contributions to many projects related to
additive manufacturing applications referred to in
present paper.
REFERENCES
Adams, C., James, D., Seniora, T., Allen, T. and
Hamilton, N. (2016). Development of a method for
measuring quasi-static stiffness of snowboard wrist
protectors. Procedia Engineering, 147, pp. 378 – 383.
Ainegren, M., Carlsson, P., Laaksonen, M. and Tinnsten
M. (2012). The influence of grip on oxygen
consumption and leg forces when using classical style
roller skis. Scand J Med Sci Sports, 24(2), pp. 301-
310.
Ainegren, M., Carlsson, P. and Tinnsten, M. (2013).An
experimental study to compare the grip of classical
style roller skis with on-snow skiing. Sports
Engineering, 16(2), pp. 115-122.
Antona-Makoshi, J. (2016). Traumatic Brain Injuries:
Animal Experiments and Numerical Simulations to
Support the Development of a Brain Injury Criterion.
Doctoral Thesis, Chalmers University of Technology,
Gothenburg, Sweden. Download available at:
http://publications.lib.chalmers.se/records/fulltext/235
126/235126.pdf
Awad, N., El-Dakhakhni, W. and Gilani, A. (2015). A
Physical Head and Neck Surrogate Model to
Investigate Blast-Induced Mild Traumatic Brain
Injury. Arab J Sci Eng., 40, pp. 945-958.
doi:10.1007/s13369-015-1583-3
Bibb, R. Eggbeer, D. and Paterson, A. (2014). Medical
Modelling: The Application of Advanced Design and

Rapid Prototyping Techniques in Medicine.
Woodhead Publishing, 516 pages.
Bäckström, M., Tinnsten, M., Koptyug, A., Rännar, L.-E.,
Carlsson, P., Danvind, J. and Wiklund, H. (2013).
Sports technology education at Mid Sweden
University. Procedia Engineering; 60, pp. 214-219
.
Bäckström, M., Rännar, L.-E. and Koptyug, A. (2012).
Spare Parts for Human Body. Science First Hand;
2(44) pp. 44-57. File download available at:
https://www.researchgate.net/publication/313367815_Spar
e_Parts_for_Human_Body
Christensen, A., Lippincott, A. and Kircher, R. (2007). An
Introduction to Electron Beam Melting with Ti6Al4V-
ELI for the Orthopaedic Device Industry. BONEZone;
6, pp 14-17.
Chudinova, E., Surmeneva, M., Koptioug, A., Skoglund,
P. and Surmenev, R. (2016). Additive manufactured
Ti6Al4V scaffolds with the RF-magnetron sputter
deposited hydroxyapatite coating. Journal of Physics:
Conference Series; 669, 012004.
Cronskär, M., Rännar, L.-E., Bäckström, M. and Koptyug,
A. (2008). Application of electron beam melting to
titanium hip stem implants. In: Proc Intl Conference
on Additive Technologies, Vienna, DAAAM
International; p. 1559.
Cronskär, M., Rännar, L.-E. and Bäckström, M. (2012).
Implementation of Digital Design and Solid Free-
Form Fabrication for Customization of Implants in
Trauma Orthopaedics. Journal of Medical and
Biological Engineering; 32(2), pp. 91-96.
Cronskär, M., Bäckström, M. and Rännar, L.-E. (2013).
Production of customized hip stem prostheses – a
comparison between conventional machining and
electron beam melting (EBM). Rapid Prototyping
Journal; 19(5), pp.365-372.
Cronskär, M. and Bäckström M. (2013). Modeling of
fractured clavicles and reconstruction plates using
CAD, finite element analysis and real musculoskeletal
forces input. WIT Transactions on Biomedicine and
Health; 17, pp. 235 - 243.
Cronskär, M. (2014). Mid Sweden University Doctoral
Thesis 191: On customization of orthopedic implants -
from design and additive manufacturing to
implementation. Mid Sweden University, Sweden
http://miun.diva-
portal.org/smash/get/diva2:745912/FULLTEXT01.pdf
Emerson, N., Carré, M., Reilly, G. and Offiah, A. (2011).
Geometrically accurate 3D FE models from medical
scans created to analyse the causes of sports injuries.
Procedia Engineering; 13, pp. 422-427.
Emerson, N., Carré, M., Reilly, G. and Offiah, A. (2013).
Simulation based upon medical data offers a fast and
robust method for the prediction of fracture risk.
Procedia Engineering; 60, pp.459 – 466.
Emerson, .N., Offiah, A., Reilly, G. and Carré, M. (2013).
Patient-specific finite element modelling and
validation of porcine femora in torsion. Strain; 49 (3),
pp. 212-220.
Fera, M., Fruggiero, F., Lambiase, A. and Macchiaroli, R.
(2916). State of the art of additive manufacturing:
Review for tolerances, mechanical resistance and
production costs. Cogent Engineering; 3: 1261503, 16
pages.
Ganesan, B., Al-Jumaily, A. and Luximon, A. (2016). 3D
Printing Technology Applications in Occupational
Therapy. Phys Med Rehabil Int.; 3(3), pp. 1085-1088.
Hassan, M.H.A. and Taha, Z. (2015). Finite Element
Analysis of Soccer Heading. Procedia Engineering,
112, pp. 46–51.
Heinl, P., Müller, L., Körnera, C., Singera, R. and Müller,
F. (2008). Cellular Ti–6Al–4V structures with
interconnected macro porosity for bone implants
fabricated by selective electron beam melting. Acta
Biomaterialia; 4(5), pp. 1536–1544.
Helene Ripa (2017),
https://en.wikipedia.org/wiki/Helene_Ripa
Huiskes, R., Weinans, H. and van Rietbergen B. (1992).
The relationship between stress shielding and bone
resorption around total hip stems and the effects of
flexible materials. Clin Orthop Relat Res.; 274,
pp.124-34.
IPC regulations on Nordik Skiing,
https://www.paralympic.org/nordic-skiing/rules-and-
regulations
Jina, Y., Plotta, J., Chena, R., Wensmanc, J. and Shih, A.
(2015). Additive Manufacturing of Custom Orthoses
and Prostheses – A Review. Procedia CIRP; 3,6 pp.
199 – 204. Available online at
http://www.sciencedirect.com
Kleiven, S. and Hardy, W. (2002). Correlation of an FE
Model of the Human Head with Local Brain Motion –
Consequences for Injury Prediction. Stapp Car Crash
Journal, 46, pp. 123-144.
Kleiven, S. (2006). Evaluation of head injury criteria using
a finite element model validated gainst experiments on
localized brain motion, intracerebral acceleration, and
intracranial ressure
International Journal of Crashworthiness, 11(1), pp 65-79.
Koptyug, A., Rännar, L.-E., Bäckström, M. and Klingvall,
R. (2012). Electron Beam Melting: Moving from
Macro- to Micro- and Nanoscale. Materials Science
Forum; 706-709, pp. 532-537.
Koptyug, A., Rännar, L.-E., Bäckström, M., Franzén, S.
and Dérand, P. (2013). Additive Manufacturing
Technology Applications Targeting Practical Surgery.
Int. J. Life Science and Medical Research; 3(1), pp.15-
24.
Koptyug, A., Rännar, L.-E., Bäckström, M. and Langlet,
A. (2013). Bulk Metallic Glass Manufacturing Using
Electron Beam Melting. In: Proc. International
Conference on Additive Manufacturing & 3D Printing,
Nottingham; July 9-10
Koptyug, A., Bergemann, K., Lange, R., Jaggi, V.-E.,
Rännar, L.-E. and Nebe B. (2014). Osteoblast
Ingrowth into Titanium Scaffolds made by Electron
Beam Melting. Materials Science Forum; 783-786, pp.
1292-1297.

Koptyug, A., Rännar, L.-E., Bäckström, M. and Cronskär,
M. (2014). Additive Manufacturing for Medical and
Biomedical Applications: Advances and Challenges.
Materials Science Forum; 783-786, pp.1286-1291.
Koptyug, A., Rännar, L.-E., Bäckström, M. and
Surmenev, R. (2017). Additive manufacturing in
metal: advances generate new research challenges.
Nanotehnology: development and applications in XXI
century; 8(4), pp. 12-36.
Koptyug, A., Rännar, L.-E., Bäckström, M. and Shen, Z.
(2017). New metallurgy of Additive Manufacturing in
Metal: Experiences from the Material and Process
Development with Electron Beam Melting
Technology (EBM). Materials Science Forum; 879,
pp. 996-1001.
Koptyug, A., Bäckström, M. and Petrone, N. (2017).
Developing an Instrumented Physical Model of the
Human Head for Studying Concussion Mechanisms.
Proc. 22nd Congress of the International Society for
Skiing Safety, Innsbruck, April, 17 – 22 2017, p. 81.
Kuzmin Ski Technology AB (2017)
http://www.kuzmin.se/pgs/skiing_en.html
MakerBot Industries, LLC (2017)
https://www.makerbot.com/products/3d-printers/
Mills, D. (2015). Future Medicine: The Impact of 3D
Printing. J Nanomater Mol Nanotechnol 4:3.
MIPS AB, http://www.mipsprotection.com/
Murr, L,. Gaytan, S., Medina, F., Lopez, H., Martinez, E.,
Machado, B., Hernandez, H., Martinez, L., Lopez, M.,
Wiker, B. and Bracke, J. (2010). Next-generation
biomedical implants using additive manufacturing of
complex, cellular and functional mesh arrays”, Phil.
Trans. Roy. Soc. A; 368, pp. 1999-2032.
Niinomi, M. and Nakai, M. (2011). Titanium-Based
Biomaterials for Preventing Stress Shielding between
Implant Devices and Bone. Intl. J. Biomater.; 2011,
Article ID 836587.
Pallis, J. Materials in Paralympic Sports. Chapter 14, in:
Materials in Sports Equipment, Volume 1. Ed. Mike
Jenkins, Elsevier, 2003 - Technology & Engineering -
424 pages
Palousek, D., Rosicky, J., Koutny, D., Stoklasek, P. and
Navrat, T. (2014). Pilot study of the wrist orthosis
design process. Rapid Prototyping Journal; 20(1), pp.
27-32.
Pauly, S., Löber, L., Petters, R., Stoica, M., Scudino, S.,
Kühn, U., and Eckert J. (2013). Processing metallic
glasses by selective laser melting. Materials Today;
1(1-2), pp. 37-41.
Payne, T., Mitchell, S. and Bibb, R. (2013). Design of
human surrogates for the study of biomechanical
injury: a review. Critical Reviews in Biomedical
Engineering; 41 (1), pp. 51-89.
Payne, T., Mitchell, S., Halkon, B.; Bibb, R. and Waters,
M. (2015). Development of novel synthetic muscle
tissues for sports impact surrogates. J. Mechanical
Behavior of Biomedical Materials; 41, pp. 357-374.
Petrone, N., Tamburlin, L., Panizzolo, F. and Atzori, B.
(2010). Development of an instrumented
anthropomorphic dummy for the study of impacts and
falls in skiing. Procedia Engineering, 2(2), pp.2587-
2592.
Samaka, H. and Tarlochan, F. (2013). Finite Element (FE)
Human Head Models / Literature Review. Intern. J. of
Sci. Tech. Research, 2(7), pp. 17-21.
Sames, W., List, F., Pannala, S., Dehoff, R and Babu, S.
(2016). The metallurgy and processing science of
metal additive manufacturing. International Materials
Reviews; 6 (5), pp. 315-360.
Skoglund, P. (2915). Prosthetic socket in Titanium, Mid
Sweden University Master Thesis. Download
available at: https://www.diva-
portal.org/smash/get/diva2:901421/FULLTEXT01.pdf
Smith, T., Halstead, P., McCalley, E., Kebschull, S.,
Halstead, S. and Killeffer, J. (2015) Angular head
motion with and without head contact: implications for
brain injury. Sports Engineering, 18(3), pp. 165-175.
Special issue: Technology for Disability Sport. (2016).
Sports Engineering; 9(3); Eds. Koptyug, A., Burkett,
D. pp 139.
Stratasys Ltd. (2017) http://www.stratasys.com/3d-
printers
Sumner, D. (2015). Long-term implant fixation and stress-
shielding in total hip replacement. J Biomech.; 48(5),
pp. 797-800.
Surmenev, R., Surmeneva, M. and Ivanova, A. (2014).
Significance of calcium phosphate coatings for the
enhancement of new bone osteogenesis–A review.
Acta biomaterialia; 10 (2), pp. 557-579.
Surmeneva, M., Chudinova, E., Syrtanov, M., Koptyug, A.
and Surmenev, M. (2015). Investigation of the HA
film Deposited on the Porous Ti6Al4V Alloy Prepared
via Additive Manufacturing. IOP Conference Series:
Material Science and Engineering; 98, 012025.
Taha, Z., Hassan, M., Aris, M. and Anuar, Z. (2013).
Predicting brain acceleration during heading of soccer
ball. IOP Conf. Series: Materials Science and
Engineering, 50(1), 012023.
Tinnsten, M., Peter Carlsson, P., Ainegren, M., and
Sandberg, S. (2010). Arrangement for a roller ski and
a roller ski. European patent EP 2418006.
Zadpoor, A. and Malda, J. (2917). Additive Manufacturing
of Biomaterials, Tissues, and Organs. Annals of
Biomedical Engineering; 45(1), pp. 1–1.
Zhong, Y., Rännar, L.-E., Liu, L., Koptyug, A., Wikman,
S., Olsén, J., Cui, D. and Shen, Z. (2017) Additive
manufacturing of 316L stainless steel by electron
beam melting for nuclear fusion applications. Journal
of Nuclear Materials; 486, pp. 234-245.
Zhong, Y., Rännar, L.-E., Wikman, S., Koptyug, A., Liua,
L., Cui, D. and Shen, Z. (2017). Additive
manufacturing of ITER first wall panel parts by two
approaches: Selective laser melting and electron beam
melting. Fusion Engineering and Design; 116, pp. 24–
33.
