
Optimal Treatment Selection for Hip Fracture Patients using a Hybrid
Decision Making System
Aleksandar Jeremic
1
, Natasa Radosavljevic
2
, Dejan Nikolic
3
and Milica Lazovic
4
1
Department of Electrical and Computer Engineering McMaster University, Hamilton, ON, Canada
2
Institute for Rehabilitation Belgrade, Belgrade, Serbia
3
Physical Medicine and Rehabilitation, University Childrens Hospital, Belgrade, Serbia
4
Faculty of Medicine, University of Belgrade, Belgrade, Serbia
Keywords:
Macular Oedema, Prediction, Estimation, Least-squares Estimation.
Abstract:
Hip fractures are most frequent cause of hospitalization after the fall in older population and consequently
have been subject of great interest in medicine and biomedical engineering. It has been observed that the
incidence of hip fractures is rising at the approximate rate of 1-3% per year, with subsequent mortality rates at
approximately 33% in first year after the fracture. Although in some cases the hydrotherapy may be improve
recovery of patients it may not be easily accessible due to limited resources. To this purpose we propose a
hybrid decision making system consisting of computer-aided decision combined with an expert opinion. We
then evaluate and compare the performance of the proposed algorithms using a data sample consisting of 413
patients that have been admitted to the Institute for Rehabilitation, Belgrade, Serbia.
1 INTRODUCTION
Hip fractures are most frequent cause of hospitaliza-
tion after the fall in geriatric population (Roudsari
et al., 2005) worldwide and consequently have been
subject of great research interest in both medicine
and biomedical engineering due to the incident fre-
quency, corresponding mortality as well as treatment
expenses. It has been reported that the incidence of
hip fractures is rising at the approximate rate of 1-3%
per year, with subsequent mortality rates at approx-
imately 33% in first year after the fracture (Johnell
and Kanis, 2004; Roche et al., 2005). Consequently
because of the increasingly large number of elderly
patients with these fractures significant advances have
been made with respect to surgical procedures, post-
surgical rehabilitation procedures as well as social
support services. It is often emphasized that man-
agement and allocation of resources is of utmost im-
portance in patient care. In practical situations the
amount of resources is limited and thus proper assign-
ment of priorities may play crucial role in recovery.
As an example certain patients experiencing hip frac-
ture may show significant progress if surgeries and
rehabilitation programs are allocated in timely man-
ner thus leading to more efficient health care.
To this purpose there are different rehabilitation
protocols that are used for the treatment of these pa-
tients as well as variety of efforts to identify parame-
ters that could serve as useful predictors of the treat-
ment outcome. Two of the commonly used parame-
ters, often correlated, which are used for this evalua-
tion is functional independence measure (FIM) which
evaluates patients’ ability to perform particular tasks
and Berg Balance Scale (BBS) which evaluates pa-
tients ability to maintain the balance. There is still
a lack of consensus among physicians regarding the
factors that are of greatest significance for the recov-
ery (of the long-term disability associated with hip
fractures., 2011)-(Adunsky et al., 2012).
In our previous work we proposed a clustering al-
gorithm for selecting patients with largest recovery
capacity with respect to Berg Balance Scale (BBS)
(Jeremic et al., 2012) as well as linear and nonlin-
ear prediction algorithms of the FIM using multi-
variate regression with respect to age, comorbidity
and type of treatment (we consider two different con-
trol groups: with and without hydrotherapy) (Jeremic
et al., 2013). It is often argued that in order to per-
form proper clinical care and management the pa-
tients should be triaged upon admission according to
their ability for recovery and/or predicted efficiency
of the treatment using hydrotherapy. To this purpose
in this paper we propose multichannel fusion algo-
301
Jeremic A., Radosavljevic N., Nikolic D. and Lazovic M..
Optimal Treatment Selection for Hip Fracture Patients using a Hybrid Decision Making System.
DOI: 10.5220/0004914703010305
In Proceedings of the International Conference on Bio-inspired Systems and Signal Processing (BIOSIGNALS-2014), pages 301-305
ISBN: 978-989-758-011-6
Copyright
c
2014 SCITEPRESS (Science and Technology Publications, Lda.)

rithm for decision making in which the two decisions
are modelled as uncorrelated binary decisions. At
the present time there is no consensus whether or not
these are correlated decisions so in order to obtain
preliminary results we propose to model them as un-
correlated decisions. We then evaluate the proposed
prediction algorithms on a data sample consisting of
413 patients that have been admitted to the Institute
for Rehabilitation, Belgrade, Serbia. For comparison
purposes we compare the performance of our com-
puter based system with expert opinion of the physia-
trist performing patient evaluation.
The paper is organizedas follows. In Section II we
describe the data set and the proposed decision mak-
ing/binary hypothesis decision algorithms. In Section
III we evaluate the applicability of the proposed algo-
rithm using a real data set. Finally, in Section IV we
discuss the results and future work.
2 SIGNAL PROCESSING
MODELS
2.1 Data Set
We have evaluated 413 eligible participants that were
referred to the rehabilitation facility from January
2011 until April 2013 after hip fracture for inclusion
into rehabilitation program and follow-up. To assess
eligibility for the inclusion in the study the patients
were evaluated by board certified physiatrist and spe-
cialist of internal medicine. Prior to the inclusion, all
the participants were informed about the study pro-
tocol and informed consent was obtained. The study
was approved by the Institutional Review Board and
was carried out according to the principles of good
clinical practice. The eventual onset of early compli-
cations was indication for the termination of the reha-
bilitation program for defined period of time. The ex-
clusion criteria for the study were recurrent hip frac-
tures and inability to completely finish the rehabili-
tation program or follow-up that was defined by the
study. Therefore, the initial group on admission con-
sisted of 467 patients, where 24 did not complete re-
habilitation program due to the worsening of health
condition and thus transferred to specialized referring
hospitals, while 30 subjects dropped out from dis-
charge period to the planned follow-up after 3 months
post-discharge. Beside Board certified Physiatrist, re-
habilitation team consisted of: licensed physical ther-
apists, licensed occupational therapists and nurses.
Once a week, the aforementioned rehabilitation team
gathered on meeting to evaluatepatients improvement
and further implementation of rehabilitation program.
Prescription of rehabilitation program was indi-
vidually addressed with particular attention to the pa-
tients functionalstatus. Patients were included twice a
day for the duration of two hours (60/60 minutes) into
physical therapy. First part of physical therapy was
composed of different exercises including those for
strength and balance improvement, conditioning and
coordination improvement. These exercises aimed to
improve walking and mobility. The second part of the
program was conducted by occupational therapist and
consisted of improving activities of daily living. The
maintenance of proper hygiene during the rehabilita-
tion program was conducted by experienced nurses.
Functional Independence Measure (FIM) and
Berg Balance Scale were used to evaluate patients
functional status on 3 occasions: at admission (Ad-
mission), on discharge from the rehabilitation facil-
ity (Discharge) and 3 months after discharge (Follow-
up). After discharge, patients were not included into
any kind of rehabilitation program and were referred
to home of residence. Both of these measures presents
valid and reliable test in the estimation of aggregated
changes in functional status that appears in the de-
fined period of the study evaluation (Young et al.,
2009)-(Dodds et al., 1993). It is composed of 18 cat-
egories that are scaled from 1-7 each (Young et al.,
2009) For the estimation of comorbidity of partic-
ipants we used Cumulative Illness rating Scale for
Geriatrics (CIRSG), and findings were presented as
severity index (SI), where SI was calculated as total
CIRS-G score divided by the number of endorsed cat-
egories (Firat et al., 2002).
We organize the data set in a database consist-
ing of 413 rows corresponding to the patients and
40 columns of different features (age, height, weight,
respiratory conditions, heart conditions, FIM at the
admission, FIM at the discharge, BBS three months
after discharge, etc.) In our previous work we ana-
lyzed cross-correlation between all the features and
extract statistically significant ones using Pearson co-
efficient. In order to study dynamics of rehabilitation
we use log-values of BBS score ratios. The rationale
behind this approach is that we expect exponential
change in balance improvement and thus log (semi-
log) models may represent better fit.
2.2 Parameter Estimation and Decision
Making
We first partition patients into two groups, those that
participated in hydrotherapy and those who did not.
Then, let y
i
denote our measurement vector consist-
ing of the FIM and BBS values 6 months after the
BIOSIGNALS2014-InternationalConferenceonBio-inspiredSystemsandSignalProcessing
302
discharge from the rehabilitation program for the ith
patient. The corresponding MANOVA model for the
first group of patients can be written as
y
i
= Xa
i
+ e
where X is the matrix of unknown parameters and a
i
is the ”source” vector for the I-th patient consisting of
a
i,i
=
1 j = 1
age of the i− th patient j = 2
comorbidity of the i− th patient j = 3
BBSatadmission j = 4
FIMatadmission j = 5
The unknown matrix X can then be estimated using a
technique similar to one proposed in (Jeremic et al.,
2013). Similarly we formulate equivalent model for
patients that were not subject to hydrotherapy and de-
note corresponding MANOVA coefficients as Y.
We then proceed to define a computer based deci-
sion for therapy selection in the following way. Ac-
cording to expert input the hydrotherapy is consid-
ered sufficiently efficient if the average sum of FIM
and BBS after dismissal from the program is more
than 25% larger compared to the value that would
be achieved without therapy. Therefore we formulate
following decision problem
H
1
=
n
choosehydrotherapy
ˆ
Xa
ˆ
Ya
≥ 1.25
In our previous work (Jeremic et al., 2013) we also
derived the nonlinear estimator for predicting values
of BBS and FIM. Similarly to the above approach
we estimate the corresponding coefficients X
n
and Y
n
where we use subscript n to denote that the coeffi-
cients are estimated using a nonlinear model in which
the predicted value is modelled as a polynomial func-
tion of age, weight and BBS and FIM admittance val-
ues. Similarly the second local detector is formulated
as
H
2
=
n
choosehydrotherapy
ˆ
X
n
a
ˆ
Y
n
a
≥ 1.25
We then propose to fuse the above two decisions
using blind adaptive algorithm proposed in our previ-
ous work (Mirjalily et al., 2003). The authors demon-
strated that by formulating empirical probabilities of
decisions one can solve in a closed form for prior
probabilities as well as probabilities of false alarm
and miss under the assumption that the performance
of local detectors does not vary significantly. We ap-
ply the following approach using similar technique
we demonstrated in (Li and Jeremic, 2011) to fuse
the above decisions of linear and non-linear predictor.
We recall it here for the case of N = 3.
u
0
=
(
1, if w
0
+
∑
2
n=1
w
n
> 0
0, otherwise
where, w
0
= log
P
1
P
0
(1)
and w
n
=
(
log((1− P
m
n
)/P
f
n
), if u
n
= 1
log(P
m
n
/(1− P
f
n
)), if u
n
= 0
The probabilities of false alarm and missed detection
of the nth local detector are denoted as P
f
n
and P
m
n
,
respectively. The optimal fusion rule tells us that the
global decision u
0
is determined by the a priori prob-
ability and the detector performances, i.e., P
1
, P
f
n
and
P
m
n
which can be solved for by solving algebraic set of
equations as demonstrated in (Mirjalily et al., 2003)
3 RESULTS
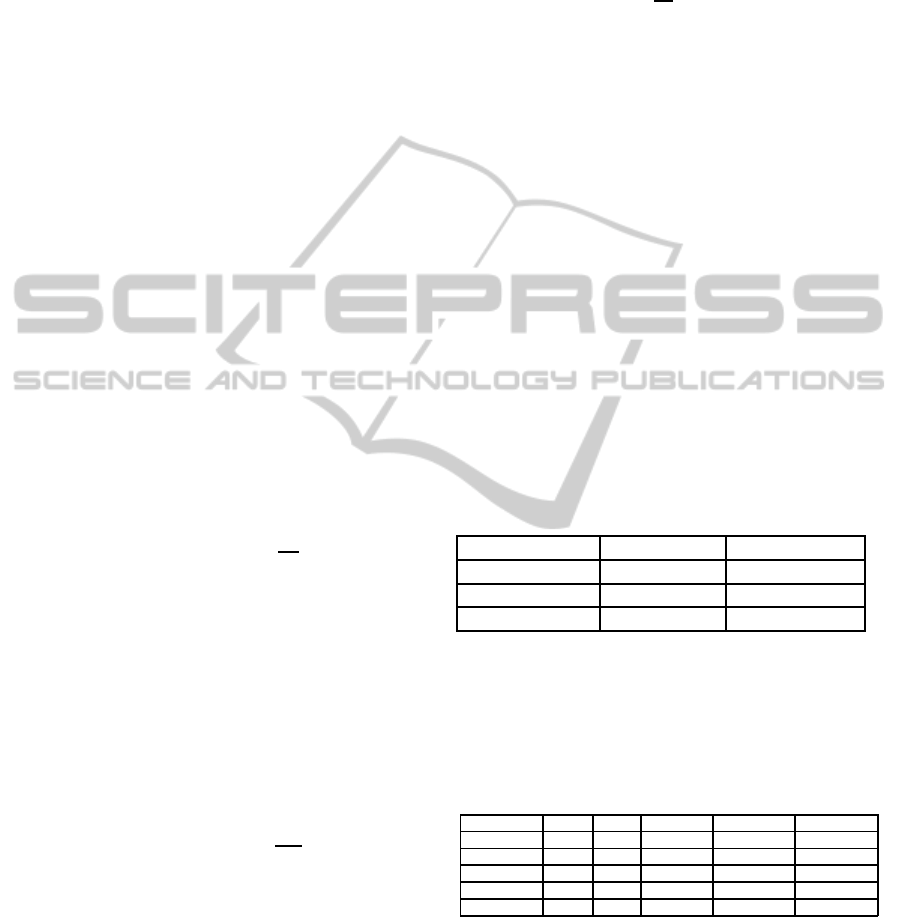
The total number of patients admitted was 413 (260
with hydrotherapy and 153 without hydrotherapy)
with general characteristics being described in Table
1.
Table 1: General characteristics of patient population with
respect to the age and severity index of fracture
Age Severity Index
Total N=413 77.63± 6.21 1.84± 0.59
Female N=271 78.28 ± 5.86 1.74± 0.43
Male N =142 76.39± 6.56 1.79± 0.62
Additionally in Table 2 we show the correlation
coefficient of the 6-month FIM with respect to the
model parameters. Based on these results we select
age and comorbidity as two most significant parame-
ters in the remainder of the paper.
Table 2.
Age Com. Wait time FIM - adm. FIM - 6mo.
Age 1.00 0.37 -0.15 -0.29 -0.57
Com. 0.37 1.00 0.20 0.48 -0.52
Wait time -0.15 0.20 1.00 0.71 0.24
FIM - adm. - 0.29 0.48 0.71 1.00 0.51
FIM - 6mo. -0.57 -0.52 0.24 0.51 1.00
To illustrate the statistical properties of the data
sample we present two scatter plots. In Figure 1 we
illustrate two-dimensional scatter plots of age and co-
morbidity (as a preliminary approach we arbitrarily
selected the two parameters with largest coefficients)
using therapy indicator as grouping parameter. In Fig-
ure 2 we present a similar three-dimensional scatter
plot with 6-months FIM as an indicator. Obviously
the decision whether or not the therapy should be used
OptimalTreatmentSelectionforHipFracturePatientsusingaHybridDecisionMakingSystem
303
65 70 75 80 85 90 95
0
5
10
15
20
25
30
Age
Comorbidity
With therapy
Without therapy
Figure 1: Two-dimensional scatter of age and comorbidity
65
70
75
80
85
90
95
0
5
10
15
20
25
30
10
20
30
40
50
60
70
80
90
Age
Comorbidity
FIM
With therapy
Without therapy
Figure 2: Three-dimensional scatter of age, comorbidity
and FIM.
2 2.5 3 3.5 4 4.5 5 5.5 6
0.01
0.015
0.02
0.025
0.03
0.035
0.04
0.045
0.05
0.055
0.06
Number of parameters
MSE
Nonlinear
Linear
Figure 3: MSE comparison nonlinear vs. linear model for
patients with hydrotherapy.
was not randomized in this study and hence we expect
to have different performance. Obviously in making
clinical decision not all the decisions can be random-
ized as it may contradict clinical protocols.
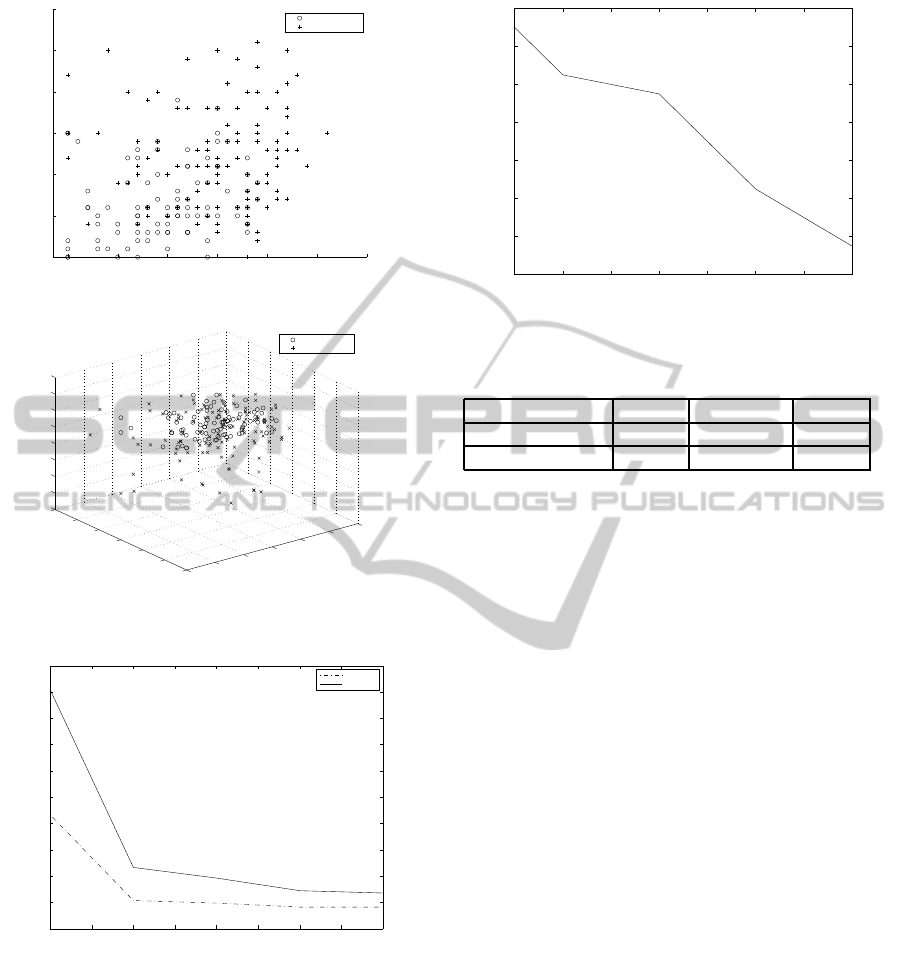
In order to evaluate the performance of the pro-
posed hybrid system we run the fusion center consist-
ing of three local detectors: linear detector, nonlin-
ear detector and human expert system. As expected
the overall probability of error decreases with the in-
crease in the number of the patients. It demonstrates
50 100 150 200 250 300 350 400
0.08
0.1
0.12
0.14
0.16
0.18
0.2
0.22
Overall Error Proabibility
Patient Number
Figure 4: Overall Probability of Error for Hybrid System.
Table 3: General characteristics of patient population with
respect to the age and severity index of fracture.
Linear Nonlinear Expert
False Positives 12% 10% 11%
False Negatives 10% 9% 8%
significant dip after number of patients reaches 300
which is consistent with our findings in (Liu et al.,
2011) where we developed optimal M-ary distributed
detection system.
In Table 3 we list the estimated performance mea-
sures of our local detectors. Note that by false
positives we determine selection of hydrotherapy
when it is not expected to provide significant advan-
tage. As expected the human system outperforms the
computer-aided systems except with the case of false
positives when compared to the non-linear system.
Note that the results in Table 3 are overall results and
it may be potentially useful to decompose these error
with respect to patients’ age and gender which may
affect human decision making.
4 CONCLUSIONS
The importance of early inclusion in rehabilitation
program and exercise of older people after the hip
fracture could be explained by the fact that physical
activity influences the muscle strength, balance and
eventually degree of hip pain (Sipila et al., 2011).
Such determinants are very important particularly for
individuals quality of life and could prevent further
risks of comorbidities and falls later in life. It has
been often hypothesized that the success of recov-
ery is extremely dependent on the timeliness and ad-
equacy of the treatment. While it is desirable to pro-
vide the best possible care as soon as possible the ac-
tual limitations that may exist in health-care systems
due to a limited number of medical staff as well as
BIOSIGNALS2014-InternationalConferenceonBio-inspiredSystemsandSignalProcessing
304

limited capacity in rehabilitation programs may cre-
ate need for appropriate planning and/or scheduling.
To this purpose in this paper we proposed an al-
gorithm which can potentially be used to determine
whether or not hydrotherapy is required. This ques-
tion may be of significant resources in scenarios in
which the number of geriatric physiatrists as well as
access to resources and/or their cost may be a limiting
factor. Furthermore we proposed a framework that
can potentially be useful for evaluating performance
of fellows and/or residents and assist them in their
training and educations as well as professional de-
velopment as it can point to potential mistakes. This
could be further used in order to evaluate the cause of
such mistakes and potential was to remedy them.
As a preliminary approach we proposed
computer-aided decision making using linear
and nonlinear models in which parameters were
chosen based on the correlation coefficient. An effort
should be made to compare the performance of these
models to non-parametric, multilevel histograms
in which FIM and BBS can be modelled using the
joint probability density function and consequently
determining a histogram based maximum likelihood
estimate. In addition the residual vector may not
be Gaussian distributed especially in which case
an effort should be made to investigate different
estimation techniques that may be more suitable for
non-Gaussian models.
Finally, a clinical study with a larger number of
patients and different waiting times should be per-
formed in order to evaluate the correlation between
waiting time (time from operation to admission to re-
habilitation program). In this particular data set, due
the similarity between waiting times, this parameter
was not a significant factor. However that may not
be the case if the waiting times are larger than certain
threshold value which should be investigated in future
work.
REFERENCES
Adunsky, A., Arad, M., Koren-Morag, N., Fleissig, Y., and
Mizrahi, E. (2012). Atrial fibrillation is not associ-
ated with rehabilitation outcomes of elderly hip frac-
ture patients. Geriatr Gerontol Int., 10:1320–1325.
Dodds, T., Martin, D., Stolov, W., and R, D. (1993). A val-
idation of the functional independence measurement
and its performance among rehabilitation inpatients.
Arch Phys Med Rehabil, 74:531–536.
Firat, S., Bousamra, M., Gore, E., and RW, B. (2002). Co-
morbidity and kps are independent prognostic factors
in stage i non-small-cell lung cancer. Int J Radiat On-
col Biol Phys, 52:1047–1054.
Jeremic, A., Radosavljevic, N., Nikolic, D., and Lazovic,
M. (2012). Analysis of berg balance scale in hip frac-
ture patients using fuzzy clustering. Proc BIOSIG-
NALS 2012, pages 466–470.
Jeremic, A., Radosavljevic, N., Nikolic, D., and Lazovic,
M. (2013). Blind adaptive decision fusion for dis-
tributed detection. Proc IEEE EMBC, pages 6421–
6424.
Johnell, O. and Kanis, J. (2004). An estimate of the world-
wide prevalence, mortality and disability associated
with hip fracture. Osteoporosis, 15(5):897–902.
Li, H. and Jeremic, A. (2011). Neonatal seizure detection
using blind multichannel information fusion. Proc
IEEE ICASSP, pages 649–652.
Liu, B., Jeremic, A., and Wong, K. (2011). Optimal dis-
tributed detection of multiple hypothesis using blind
algorithm. IEEE Transactions on Aerospace and Elec-
tronic Systems, pages 317–331.
Mirjalily, P., Luo, T., and Davidson, T. (2003). Blind adap-
tive decision fusion for distributed detection. IEEE
Transactions on Aerospace and Electronic Systems,
39:34–52.
of the long-term disability associated with hip fractures., R.
(2011). Bertram, m and norman, r and kemp, l and
vos, t. Inj Prev, 7:365–370.
Roche, J., Wenn, R., Sahota, O., and Moran, C. (2005).
Effect of comorbidities and postoperative complica-
tions on mortality after hip fracture in elderly peo-
ple: prospective observational cohort study. BMJ,
331:1374.
Roudsari, B., Ebel, B., Corso, P., Molinari, N., and
Koepsell, T. (2005). The acute medical care costs of
fall-related injuries among u.s. older adults. Injury,
36(1):1316–132.
Sipila, S., Salpakoski, A., Edgren, J., Heinonen, A., Kaup-
pinen, M., and M, A.-K. (2011). Promoting mobility
after hip fracture (promo): study protocol and selected
baseline results of a year-long randomized controlled
trial among community-dwelling older people. BMC
Musculoskelet Disord, 27:277.
Young, Y., Fan, M., Hebel, J., and Boult, C. (2009). Con-
current validity of administering the functional inde-
pendence measure (fim) instrument by interview. Am
J Phys Med Rehabil, 88:766–770.
OptimalTreatmentSelectionforHipFracturePatientsusingaHybridDecisionMakingSystem
305
