
Policy-based Emergency Bio-data Transmission Architecture for
Smart Healthcare Service
Jae-Wook Nah, Seung-Man Chun and Jong-Tae Park
College of IT Engineering, Kyungpook National University, Daegu, Korea
Keywords: Smart Healthcare, e-Healthcare, IEEE 11073, HL7, Policy-based Medical Service.
Abstract: In this paper, we propose a policy-based emergency bio-data transmission architecture for smart healthcare
service. Using the proposed service architecture, the medical staff or doctors can monitor the emergency
bio-data of remote patients in accordance with policy. The proposed system consists of three tiers:
measurement tier of bio-data of patients, policy-based transmission tier of bio-data of patients, and message
conversion tier between IEEE 11073 PHD (Personal Health Device) message and HL7 CDA (Clinical
Document Architecture). Bio-data of patients are monitored by an IEEE 11073 PHD agent such as a pulse
oximeter, glucose meter, etc., and it is transmitted to IEEE 11073 PHD manager. The manager diagnoses
the bio-data information in accordance with policy. The manager software can be installed in either a
smartphone or PC where it transmits the bio-data information to the UMS (Urgency Management Server).
The UMS converts the IEEE 11073 PHD message to a HL7 CDA standard message, after which it sends the
converted HL7 CDA message to the medical staff or medical system. Finally, the medical staff can perform
diagnoses using the patient bio-data information. Details of the proposed system architecture are discussed.
1 INTRODUCTION
Mobile, wireless, pervasive computing, and
communication environments are changing the way
medical staff interact with their patients and the
elderly. By employing self-organized wireless
physiological-monitoring hardware/software
systems, continuous patient monitoring can be used
to assure timely intervention by a healthcare
practitioner or physician. For example, cardiac
patients wearing ECG (Electrocardiogram) sensor
systems can be monitored remotely without visiting
the hospital. Healthcare sensor systems are required
to be connected directly or indirectly to the Internet
at all times (Hung, 2009).
Moreover, physiological records are collected
over a long period of time in order to allow accurate
diagnoses and correct treatment by physicians.
However, developing a pervasive sensor network for
healthcare has numerous challenges, including
conformation of wireless healthcare sensor systems
to the human body, integration of different wireless
networks with various transmission techniques, and
development of healthcare applications over these
types of networks. Hung (Hung, 2009) proposed a
healthcare monitoring architecture coupled with
wearable sensor systems and an environmental
sensor network for monitoring elderly or chronic
patients in their residences.
Patient-related bio-data such as weight, ECG,
EEG (Electroencephalography), SpO2 (oxygen
Saturation), etc. measured by sensors in, over, on,
and around the patient are delivered to the surgeon,
who checks the health status of the patient. In the
delivery of patient-related data, international
standards such as IEEE 11073 PHD, HL7 (Health
Level 7) CDA, etc. are used.
IEEE 11073 PHD (Personal Health Device)
standards are a group of standards that address the
interoperability of PHDs, such as weighing scales,
blood pressure monitors, blood glucose monitors,
and the like (IEEE 11073-20601, 2008). IEEE 11073
PHD focused on ubiquitous environments,
implementing high quality sensors, supporting
wireless technologies such as Bluetooth or Zigbee,
and providing faster and more reliable
communication network resources. Further, IEEE
11073 PHD standards are adequate for homecare
challenge and might be the best-positioned
international standards to reach this goal.
HL7 is a messaging standard for exchanging
medical information and is becoming a world
167
Nah J., Chun S. and Park J..
Policy-based Emergency Bio-data Transmission Architecture for Smart Healthcare Service.
DOI: 10.5220/0004194501670173
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2013), pages 167-173
ISBN: 978-989-8565-37-2
Copyright
c
2013 SCITEPRESS (Science and Technology Publications, Lda.)

standard (HL7, 2012). HL7 Version 2.5.1 Messaging
Standard has a defined syntax for information
representation of segments, data types, flags, and
mapped fields.
There have been numerous attempts to apply
international standards for healthcare system
development (Huang, 2009) (Kim, 2010) (Trigo,
2009) (Yao, 2005). Previously, the relationships
between the ISO/IEEE 11073 (usually referenced as
x73) PHD model for ECG devices and the fields of
the SCP-ECG standard (European Standard
EN1063) were investigated (Trigo, 2009). Yao et al.,
(Yao, 2005) employed the IEEE/ISO 11073 and
Bluetooth standards to achieve device auto-
association, interoperability, and simple
reconfigurability. Huang (Huang, 2009) proposed a
healthcare monitoring architecture that uses
wearable sensor systems and an environmental
sensor network for monitoring elderly or chronic
patients in their residences. They proposed a
hierarchical network architecture that measures
patient-related data and accesses the Internet through
GPRS/3G/WiFi.
Kim et al., (Kim, 2010) proposed the integration
of the IEEE 1451 and HL7 standards for exchanging
information obtained from patients’ sensors. In their
proposed structure of the healthcare system, medical
staff can access the mobile device of a patient by
using the IEEE 1451 and HL7 standards.
In most healthcare monitoring systems,
emergency judgement of patient bio-data is carried
out only by the medical staff. For this, the bio-data
should be transmitted continuously to medical staff
at a remote location. It is difficult for medical staff
to monitor great number of people since their
numbers are limited.
In this paper, in order to overcome the above-
mentioned problem, we propose a policy-based
emergency bio-data transmission architecture for a
smart healthcare service. Through the proposed
service architecture, medical staff can monitor the
emergency bio-data of remote patients quickly and
accurately. The proposed system consists of three
tiers: measurement tier of bio-data of patients,
policy-based transmission tier of bio-data of
patients, and message conversion tier between IEEE
11073 PHD message and HL7 CDA. More
specifically, patient bio-data are measured by an
IEEE 11073 PHD agent such as a pulse oximeter,
glucose meter, etc., after which the data are
transmitted to an IEEE 11073 PHD manager such as
a smart mobile device. The manager software
diagnoses the bio-data information in accordance
with policy, and it transmits the bio-data information
to the UMS (Urgency Management Server). The
UMS then converts the IEEE 11073 PHD message
to a HL7 CDA standard message, after which it
sends the converted HL7 CDA message to the
medical staff or medical system. Finally, the patient
bio-data information is diagnosed by the medical
staff.
The rest of the article can be described as follows.
In Section 2, we describe the general service
architecture of the patient monitoring system. In
Section 3, we propose the system structure of the
policy-based patient monitoring service with policy-
based emergency management for healthcare
service. In Section 4, we implement the proposed
system and evaluate its performance. Finally, the
conclusion follows in Section 5.
2 GENERAL SERVICE
ARCHITECTURE OF PATIENT
MOBITORING SYSTEM FOR
HEALTHCARE SERVICE
The general service architecture of the patient
monitoring system for healthcare service
(Pantelopoulos, 2010); (Li, 2010); (Huang, 2009)
consists of a mobile device, a central management
server, database, and hospital monitoring system.
Each component performs its function as follows.
The mobile node measures the patient-related data,
which are transmitted from the wireless sensors. The
central management server then collects the patient-
related data from the mobile device and relays the
data to the hospital monitoring system. The patient-
related data are then stored in the database such as
EHR/PHR (Electronic Health Record/Personal
Health Record). Next, the hospital monitoring
system receives the patient-related data from the
central management server. The surgeon in the
hospital system then judges whether or not the data
are emergency-data or patient-related as well as
checks the health condition of the patient. If it is
determined from the data that the health condition of
the patient is associated with emergency, the
surgeon calls an ambulance for timely treatment.
To reliably transmit the bio-data information in
the healthcare system, there are several technologies
and international standards, such as IEEE 11073
PHD, HL7, DICOM, etc. More specifically, a sensor
(called agent in IEEE 11073 PHD) and mobile
device (manager, IEEE 11073 PHD standards) are
used. The IEEE 11073 standard is a family of
standards intended to interconnect and interoperate
HEALTHINF2013-InternationalConferenceonHealthInformatics
168
medical devices (IEEE 11073 agent and manager)
with each other.
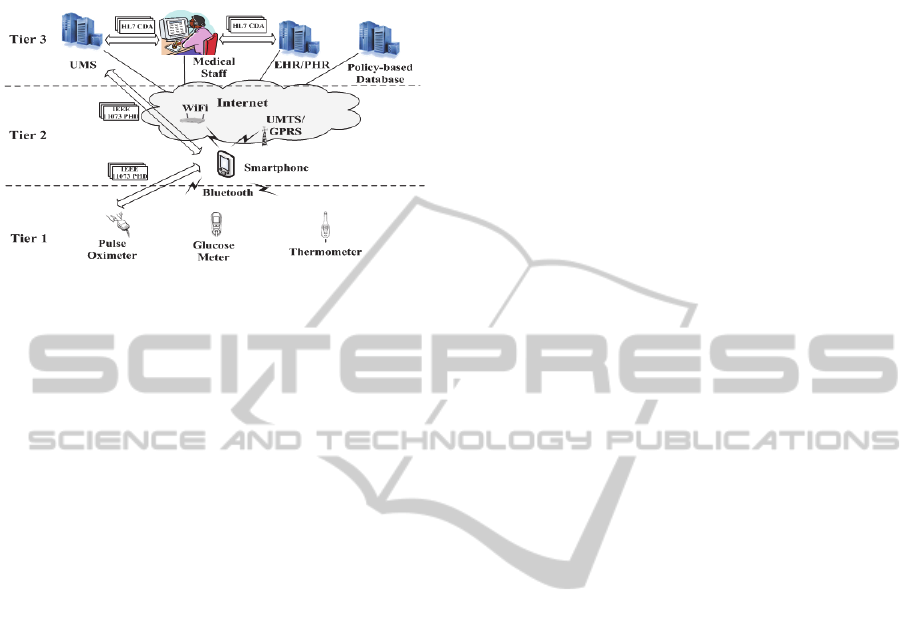
Figure 1: Architecture of policy-based urgency patient
monitoring system.
3 PROPOSED POLICY-BASED
PATIENT MONORING SYSTEM
WITH HENDLING
EMERGENCY-PATIENT
3.1 Structure of Policy-based Patient
Monitoring System
Figure 1 shows the architecture of the policy-based
patient monitoring system. The proposed system
consists of an IEEE 11073 agent such as a pulse
oximeter, glucose meter, etc., an IEEE 11073
manager such as a smartphone or tablet PC, policy-
based database, UMS (Urgency Management
Server), medical staff, and EHR/PHR database.
IEEE 11073 agent and manager are equipped
with the IEEE 11073 PHD standard protocol stack.
The policy-based database stores a variety of critical
bio-data information. The IEEE 11073 manager
judges whether or not bio-data information is urgent
or not by investigating the critical bio-data
information from the policy-based database.
EHR/PHR stores the personal bio-data information,
which is received by the UMS. The UMS performs
message conversion between the IEEE 11073 PHD
and HL7 CDA standards.
The proposed healthcare service architecture
consists of three tiers. Tier 1 measures and delivers
the bio-information in accordance with the IEEE
11073-20601 standard. IEEE 11073 agent and
manager exchange the bio-data information through
the wired/wireless network interface, such as WPAN
(Wireless Personal Area Network), LAN (Local
Area Network), WLAN (Wireless Area Network),
etc.
Tier 2 performs monitoring of bio-data from
IEEE 11073 PHD agent(s) and performs
filtration/aggregation of the bio-data. It then assesses
urgency by referring to the policy database
information. If urgency is detected, a manager sends
an urgent message to the UMS.
In tier 3, the UMS performs conversion from
IEEE 11073 PHD message format to HL7 CDA
message format to enable medical staff to check the
personal bio-data. The medical staff then makes a
decision regarding the urgent situation. If the
medical staff declare an emergency based on the
bio-data, an urgent message is created and sent to
the UMS for monitoring and gathering of the bio-
data information on a certain patient. The bio-data
transmitted from IEEE 11073 PHD agent arrives in
the medical system through the UMS.
3.2 Structure of Urgency Management
Server
Figure 2 shows the architecture of the UMS. The
UMS is located between the IEEE 11073 agent and
medical staff, and it converts IEEE 11073 PHD
message format to HL7 CDA message format or
from HL7 CDA message format to IEEE 11073
PHD message format to monitor the personal bio-
data information. The UMS also converts the
gathered bio-data to CDA document format.
The UMS is comprised of the IEEE 11073
manager, CDA Factory, HL7 v2.x Converter. The
HL7 v2.x Converter converts the received bio-
information to the HL7 message through the IEEE
11073 manager. It also analyses HL7 message
received from the remote site to the bio-information
monitoring application. HL7 is comprised of the
MSH (Message Header Segment), EVN (Trigger
Event), PID (Patient Identification Segment), OBR
(Observation Request Segment), or essential
Segment of the OBX (Observation Result Segment).
The request for the bio-information is specified in
OBR field, and the bio-information received from
the IEEE 11073 agent is transmitted to the OBX
field. The HL7v2.x Converter is comprised of
Metafile Handler and HL7 Message Converter.
The Metafile Handler analyses the meta data in
the HL7v2.x message and verifies the meta
information. The HL7 Message Converter parses the
HLT message received from bio-information
monitoring application at the remote site, after
whichi t requests the bio-information to the IEEE
11073 manager. Data mapping between the IEEE
11073 manager and HL7v2.x Converter is perfor-
Policy-basedEmergencyBio-dataTransmissionArchitectureforSmartHealthcareService
169
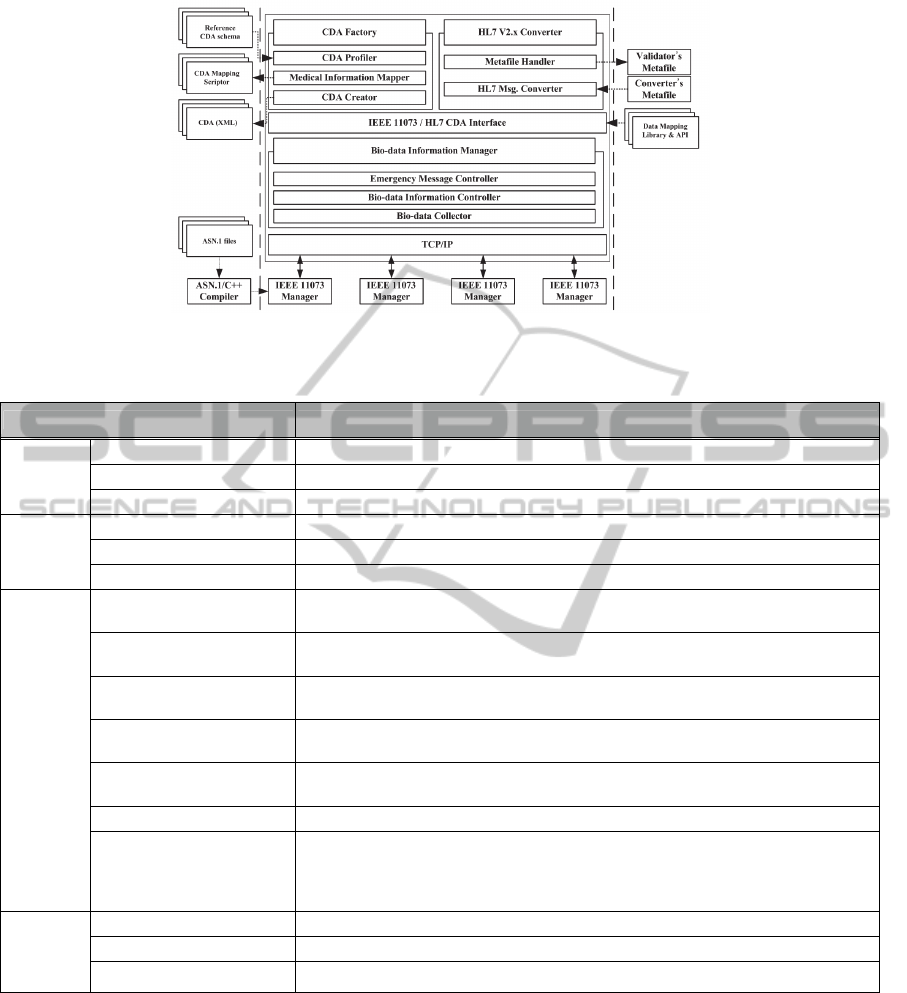
Figure 2: Structure of urgency management server.
Table 1: Service policy management for emergency healthcare monitoring service.
Policy Description
Emergency
Service
SetUp
Setting Setting of emergency bio-data types, patient’s information, emergency level
Info Information describing emergency service
Time Define starts and stop times for emergency service
Patient
Management
PatientInformation_SetUp Delivery of patient individual information for medical information generation
PatientBioData_SetUp Delivery of each patient specific bio-data for disorder judge
BioDataType_SetUp Delivery of bio-data type, detection time, and medical device ID
Disease
Management
Emergency
Management
DisordersChecker_Status
Delivery of DisordersChecker status such as currently operation status or configuration of
disorders checker
DisorderChecker_SetUp
Request ready for DisordersChecker for close examination for received
bio-data from IEEE 11073 manager
CriticalValuePreset_SetUp
Delivery preset critical value of each bio-data for preliminary examination at IEEE 11073
manager
Emergency_Creation
Declare emergency situation and request preparation for emergency communication
through hot line
EmergencyCommander_SetUp
Delivery of information for emergency communication such as medicaldevice ID and
patient individual information
EmergencyBioData_SetUp Delivery of bio-data information such as detected time, type and detected bio-data
HotLine_SetUp
Delivery emergency information and request preparation for hot line which communicate
with physician for transmission emergency data. The hot line means that only emergency
patient can transmit bio-data to physician. When the hot line is operating other medical
devices stop data transmission.
Protocol
Conversion
Mgt.
ManagerStatus_SetUp Delivery manager status such as current list of connected agents
IEEE11073Analyzer_SetUp Delivery IEEE 11073 bio-data and request ready for mapping to HL7 message
HL7Message_Creation Delivery bio-data, medical device ID, patient information for generation HL 7 message
med through the IEEE 11073/ HL7 CDA Interface.
Data mapping information conforms to standard
protocol.
CDA Factory of the IEEE 11073/HL7 protocol
conversion gateway produces a HL7 CDA document
that includes the bio-information collected in IEEE
11073. CDA documentation contains all information
related to treatment of the bio-information or patient,
and it is structured in the XML format of RIM
(Reference Information Model) of the HL7 (Dolin,
2005). The object information for comprising CDA
is comprised of Act, Participation, Entity, Role, and
ActRelationship.
CDA Factory is comprised of a CDA Profiler,
Medical Information Mapper, and CDA Creator.
CDA Profiler verifies the inputted CDA document
or outputted CDA document. The Medical
Information Mapper performs mapping of the bio-
information and meta information received from the
HL7 v2.x Converter or IEEE 11073 manager to RIM
HEALTHINF2013-InternationalConferenceonHealthInformatics
170
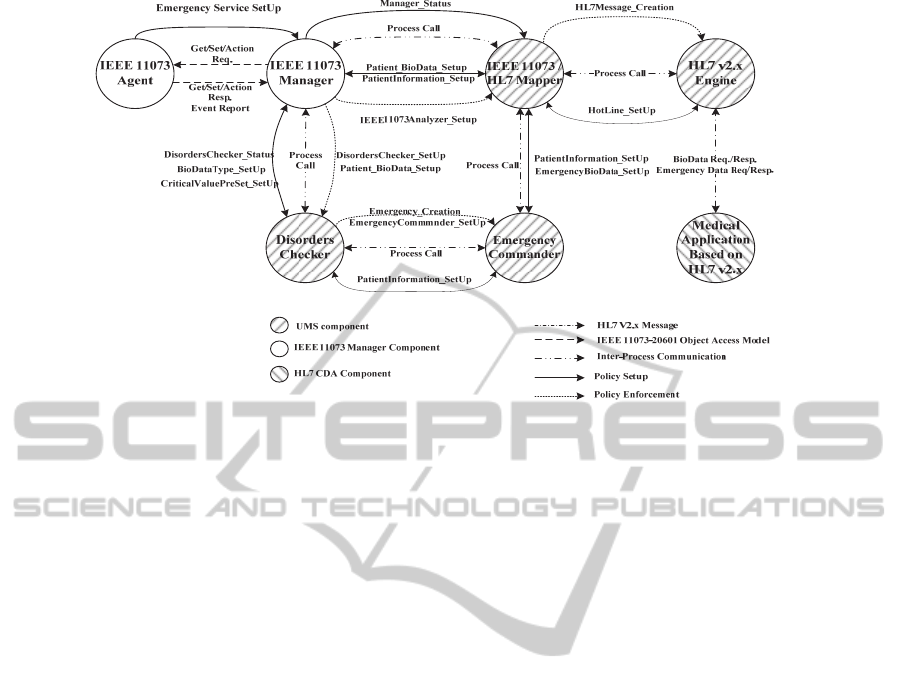
Figure 3: Message flow diagram for policy-based urgency service management.
base class of the CDA document structure. The CDA
document is produced based on the CDA template
prepared in the CDA Profiler. According to the
IEEE 11073 agent, several CDA templates are
generated that collects the bio-data information from
the IEEE 11073 agent. The generated CDA
document is verified again in the CDA Profiler.
The bio-data Information Manager consists of an
Emergency Notifier, Data Aggregation, and Data
Filtering. The Information manager makes an
emergency decision, which is received from the
sensor. If an emergency situation is detected, an
emergency notification message is created and
transmitted to the UMS. The bio-data Collector
finally transmits the bio-data information from the
UMS to the IEEE 11073 PHD manager. The
received bio-data information converts HL7 CDA
message format in accordance with the policy
information.
3.3 Message Flow Diagram for
Policy-based Emergency Service
Management
In this section, we describe the structure of policy-
based urgency service management for emergency
patients that suffer from physical trauma, etc. The
policy database is composed of patient management,
disease management, and emergency management.
The transmission of the bio-data information can be
managed through these management functions.
Table 1 indicates service policy management for
the emergency healthcare monitoring service. UMS
judges whether or not the bio-data information
warrants an emergency in accordance with the
policy information. If an emergency situation is
detected, the UMS sends an emergency notification
message to the medical staff. Upon receiving the
notification message, the medical staff sends an
emergency response message to obtain certain
personal bio-data information. Then, the UMS sends
the requested bio-data information and stops
transmission of other non-urgent bio-data
information in order to quickly and reliably transmit
the requested bio-data information.
Figure 3 shows the message flow diagram for the
policy-based emergency service management. In
Figure 3, the patient who needs emergency service,
requests the emergency service setup to the IEEE
11073 manager. The emergency service setup
request message requested from the IEEE 11073
agent to IEEE 11073 manager does not conform to
the IEEE 11073 PHD standard. Thus, we added
additional message signalling of data conversion.
In response to this request, the IEEE 11073
manager compares the bio-data of the patient, which
are received from the IEEE 11073 agent, and sets
the critical value repository. By checking the critical
value, the UMS refers to the DisordersChecker
SetUp policy for operation of the DisordersChecker.
If the critical value exceeds the preset value for
determining the emergency bio-data, the IEEE
11073 manager refers to Patient_BioData_SetUp
and BioDataType_SetUp policy.
Policy-basedEmergencyBio-dataTransmissionArchitectureforSmartHealthcareService
171
4 PERFORMANCE EVALUATION
4.1 Implementation Environment
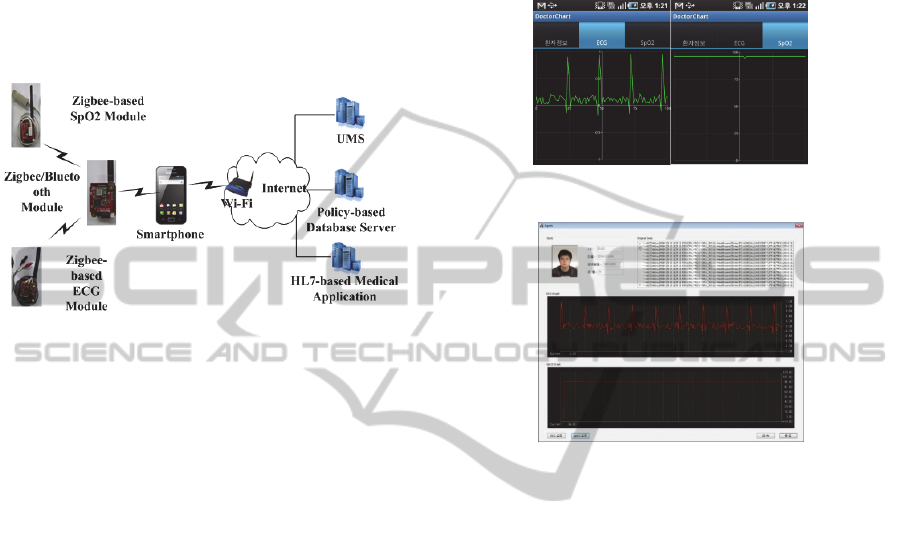
Figure 4 shows the implementation environment for
policy-based healthcare monitoring. We used two
types of sensors; ECG sensor and SpO2. We used an
HBE-ZigbeX2 device provided by the HANBACK
Company in Korea.
Figure 4: System environment for policy-based healthcare
monitoring.
Server : IBM Server
Mobile device : smartphone
Type of sensor (product standard): Bluetooth
module (HBE-ZigbeX2-Bluetooth), SpO2 (HBE-
ZigbeX2-Spo2), ECG sensor module
Development language : visual C, MFC
The bio-data information (SpO2 and ECG) is
measured and transmitted according to IEEE 11073-
10404 (11073-10404, 2008) and 11073 to 10406
(11073, 2008) standards.
4.2 Policy-based Healthcare
Monitoring System Scenario
The system operation scenario is as follows: two
types of bio-data information, i.e., SpO2 and ECG
are measured by the ZigBee-based SpO2
measurement module and ZigBee-based ECG
measurement module, respectively. Measured bio-
data are transmitted to a smartphone through ZigBee
communication and Bluetooth communication. A
smartphone requests the critical policy information
with regard to SpO2 and ECG to a policy-based
database server. Then, the smartphone monitors the
bio-data information.
If the measured bio-data information incurs
critical urgency conditions, the smartphone sends an
emergency notification message to the UMS. Then,
the UMS sends an emergency notification message
to the HL7-based medical application after its
message is converted to HL7 CDA format. The
HL7-based medical application requests the
measured certain bio-data on a smartphone via the
UMS. Finally, the measured bio-data on the Zigbee-
based module arrives in the HL7-based medical
application.
Figure 5: Display view on smartphone.
Figure 6: Display view of HL7-based medical application.
4.3 Implementation Results
Figure 5-Figure 8 show the implementation results
of the policy-based urgency healthcare monitoring
system. Figure 5 shows an ECG graph and SpO2
graph on a smartphone. The bio-data information in
these graphs is received by the Zigbee-based ECG
and SpO2 measurement modules in real-time in
IEEE 11073 message format. The bio-data
information is monitored, and the urgency status of
the data is determined.
Figure 6 shows the HL7-based medical
application. ECG and SpO2 bio-data in the HL7-
based medical application are received from the
UMS in HL7 CDA message format.
Figure 7 and Figure 8 show the emergency
notification message that is received from the HL7-
based medical application in the UMS along with
the emergency notification message that is received
from the UMS in the HL7-based medical application,
respectively. This emergency message is generated
by the HL7 v2.1 engine.
HEALTHINF2013-InternationalConferenceonHealthInformatics
172
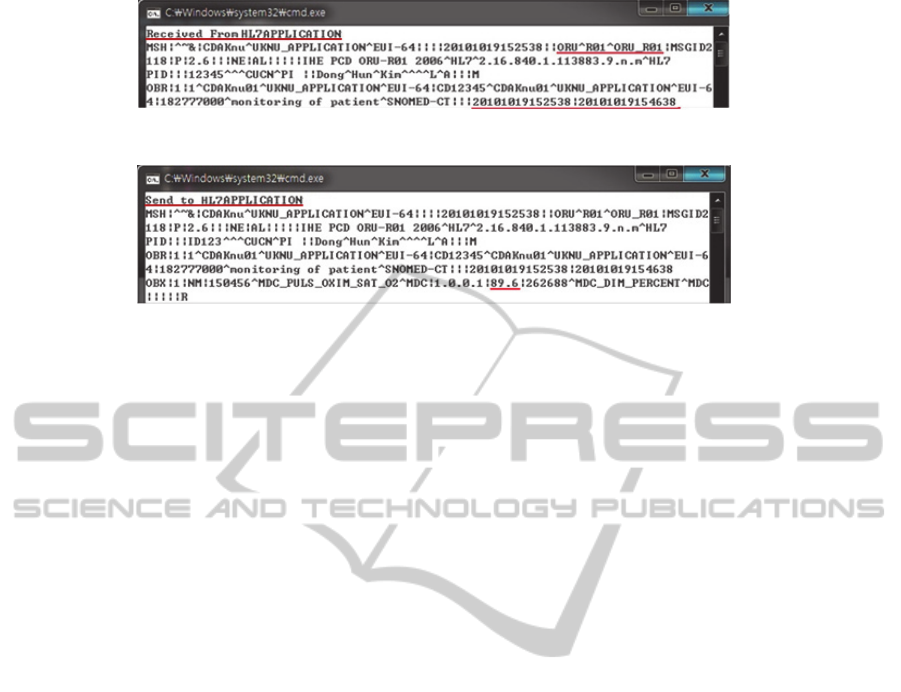
Figure 7: Emergency notification message received from HL7-based medical application in UMS.
Figure 8: Emergency notification message received from UMS in HL7-based medical application.
5 CONCLUSIONS
In this paper, we presented a policy-based
emergency bio-data transmission architecture for
smart healthcare service. Since various healthcare
standards have been researched by international
standard organizations such as IETF, ISO, Continua,
HL7, etc., these international standards should be
interworked. For this, we designed an interworking
architecture of the IEEE 11073 PHD and HL7 CDA
standards. In addition, we presented a policy-based
transmission architecture in order to increase the
reliability of transmission. The details of the
proposed system architecture have been
implemented.
ACKNOWLEDGEMENTS
This research was supported by the MKE (The
Ministry of Knowledge Economy), Korea, under the
ITRC (Information Technology Research Center)
support program supervised by the NIPA (National
IT Industry Promotion Agency) (NIPA-2012-
(C1090-1121-0002)), second stage BK21 Project
and Kyungpook National University Research Fund.
REFERENCES
Huang Y. M. et al, 2009. “Pervasive, Secure Access to a
Hierarchical Sensor-Based Healthcare Monitoring
Architecture in Wireless Heterogeneous Networks,”
IEEE journal on Selected Areas in Comm., vol. 27, no.
4, May 2009, pp. 400-411.
The Institute of Electrical and Electronics Engineers, 2008,
ISO/IEEE 11073-20601 Standard for Health
Informatics - Personal health device communication -
Application profile - Optimized exchange protocol.
ISO/IEEE 11073-20601.
HL7 – Healthcare Level 7 at http://www.hl7.org/, 2012.
Kim, W. S., Lim, S., So. J., Ahn, J., Nah, N., 2010.
"Integration of IEEE 1451 and HL7 Exchanging
Information for Patients' Sensor Data," Journal of
Medical System, vol. 34, no. 6.
Trigo, J. D., Chiarugi, F., Alesanco, Á., et. al., 2009.
“Standard-Compliant Real-Time Transmission of
ECGs: Harmonization of ISO/IEEE 11073-PHD and
SCP-ECG,” 31st Annual International Conference of
the IEEE EMBS, Minneapolis, Minnesota, USA, Sept.
2-6, 2009.
Yao, J., Warren, S., 2006. “Applying The ISO/IEEE
11073 Standards to Wearable home Health Monitoring
Systems,” Journal of Clinical Monitoring and
Computing, vol. 19, pp. 427-436.
Shnayder, V. Chen, B. et al, 2005. “Sensor Networks for
Medical Care,” Harvard Univ., Tech. Rep. Technical
Report TR-08-05, April 2005.
Viruete, E. A., J. Navarro, M. Ruiz, Fernandez J., C.
Navajas, A. Pena, 2006. “Performance of a 3G-Based
Mobile Telemedicine System,” In proc. IEEE CCNC
2006, Jan. 8-10, 2006, pp. 1023-1027.
Pantelopoulos, A., ourbakis, G. 2010. “A Survey on
Wearable Sensor-Based Systems for Health
Monitoring and Prognosis,” IEEE Trans. On System,
MAN and Cybernetics, vol. 40, no. 1, pp. 1-12.
Li, M., Lou, W., 2010. “Data Security and Privacy in
Wireless body Area Networks,” IEEE Wireless
Communications, vol. 17, Iss. 1, Feb. 2010, pp. 51-58.
Dolin, R. H., Alschuler, L., Boyer, S., Beebe, C., Behlen,
F. M. et al., 2005. "HL7 Clinical Document
Architecture, release 2," J. Am. Med. Inform. Assoc.,
13(1), pp. 30-39, 2005.
11073-10404 and 11073-10406, The Institute of Electrical
and Electronics Engineers, 2008, ISO/IEEE 11073-
20601 Standard for Health Informatics - Personal
health device communication - Device Specialization -
Pulse Oximeter, ISO/IEEE 11073-10404.
Policy-basedEmergencyBio-dataTransmissionArchitectureforSmartHealthcareService
173
