
A PROPOSAL OF A WORKFLOW-BASED CBR FOR
INTERVENTIONAL CDSS
Application to Transcatheter Aortic Valve Implantation (TAVI)
Andres El-Fakdi, Joaquim Mel
´
endez and Roberto Petite
Control Engineering and Intelligent Systems Group eXIT, University of Girona
Campus Montilivi Building PIV, 17071 Girona, Spain
Keywords:
Clinical decision support systems, Case-based reasoning, TAVI, Clinical workflow.
Abstract:
A Clinical Decision Support System (CDSS) is an interactive software designed to assist physicians, and
other health professionals, with health decision-making tasks through an inference process that associates
observations with conclusions supported by objective and expert knowledge on a specific application domain.
As complexity of surgical processes arises, there is a demand from the clinicians to extend the capabilities
from a pure research database towards a clinically integrated decision support system. The work presented
in this paper details a proposal of a CDSS designed to to assess clinicians during interventions by retrieving
and reusing past similar cases. Following an operative workflow, the designed software will use a Case-Based
Reasoning (CBR) methodology to retrieve similar past cases from a case base to give case-specific advice
at any particular point of the process, specially during preoperative and intraoperative stages. The proposal
intends to develop a monitoring mechanism capable to recognize relevant data to every stage in the intervention
workflow. Thus, measures and observations generated during the intervention will be used to retrieve the most
similar cases occurred in previous occasions. The paper proposes an example application of the CBR strategy,
where it is adapted to a recent complex minimally invasive intervention which is receiving growing attention
lately, the Transcatheter Aortic Valve Implantation (TAVI).
1 INTRODUCTION
In a general term, CDSSs comprise a large spectrum
of systems which provide clinicians, staff, patients,
and other individuals with knowledge and person-
specific information, intelligently filtered and pre-
sented at appropriate times, to enhance health and
health care (Berner, 2009). CDSSs have been used
in clinical practice since 1970, but despite several
individual success since then, their impact on rou-
tine clinical practice has not been as strong as ex-
pected, specially due to the barriers to their im-
plementation, which still remain in place. CDSSs
should form an important part of the field of clin-
ical knowledge management technologies through
their capacity to support the clinical process and use
of knowledge,including knowledge maintenance and
continuous learning, from diagnosis and investigation
through surgery, treatment and long-term care. Argu-
ments for and against the value of CDSSs have been
discussed over the years. Among its potential ben-
efits, as stated in (Coiera, 2003), CDSSs could im-
prove patient safety through reduced medication er-
rors and adverse events. Also, they should improve
quality of care by increasing pathways, guidelines and
documentation available for patients. Another advan-
tage is that CDSSs may improve efficiency in health
care delivery, reducing costs through faster order pro-
cessing and avoiding test duplication. As drawbacks,
clinicians may see CDSSs as a threat to clinical judg-
ment and sometimes too inflexible, with difficulties
to depart from ordered, pre-prepared paths. Also,
computer-supported decision systems promote over-
reliance on software decisions which may limit clin-
icians’ freedom to think at some point. In the same
way, bad designed systems can create extra work or
extend clinical procedures more than necessary. Fi-
nally, maintenance costs, professional support and
training needed by the medical staff in order to use
the software properly could also be seen as arguments
against the utilization of CDSSs.
Decision support can be provided at various stages
in the care process, from preventive care through di-
agnosis and treatment to monitoring and follow-up.
As detailed in (Perreault and Metzger, 1999), com-
puter CDSSs can be designed to support four ba-
201
El-Fakdi A., Meléndez J. and Petite R..
A PROPOSAL OF A WORKFLOW-BASED CBR FOR INTERVENTIONAL CDSS - Application to Transcatheter Aortic Valve Implantation (TAVI).
DOI: 10.5220/0003771302010206
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2012), pages 201-206
ISBN: 978-989-8425-88-1
Copyright
c
2012 SCITEPRESS (Science and Technology Publications, Lda.)

sic clinical functions. First, giving administrative
support, aiding in clinical coding and documenta-
tion, authorization of procedures, and referrals. Sec-
ond, managing clinical complexity, keeping patients
on research and chemotherapy protocols, tracking or-
ders, referrals follow-up, and preventive care. The
third function deals with cost control, programming
CDSSs to monitor medication orders with the objec-
tive of avoiding duplicate or unnecessary tests. A
fourth stage of application, which represents the fo-
cus of this work, involves CDSSs with low level de-
cision support, helping in clinical diagnosis and treat-
ment plan processes, giving case-specific support in
highly complex surgery operations or Minimally In-
vasive Surgerys (MISs), promoting use of best prac-
tices and guidelines based on population case man-
agement.
The work presented in this paper details a proposal
of a CDSS designed to give case-specific assessment
to clinicians during complex surgery or minimally in-
vasive interventions. Following a perioperative work-
flow, the designed software will use a Case-Based
Reasoning (CBR) methodology (see Figure 2) to re-
trieve similar past cases from a case base to give case-
specific advice at any particular point of the process,
specially during preoperative and intraoperative steps.
This support will be presented in the form of 2D/3D
images, numerical data or decisions taken based on
past similar cases. The intervention will be moni-
torized and used to recognize similar previous cases
at any time during the intervention. The paper pro-
poses an example application of the method, adapted
to assist a recent complex minimally invasive surgery
which is receiving growing attention lately, the Tran-
scatheter Aortic Valve Implantation (TAVI). This pa-
per is structured as follows. In Section 2 recent appli-
cations of CDSS for surgical processes are reviewed.
Also, a description of the workflow management dur-
ing an intervention is detailed. Section 3 describes
the proposed workflow-based CBR for assessment in
complex surgical procedures. In Section 4, the pro-
posed support system is exemplified with its applica-
tion to a minimally invasive surgical procedure, TAVI.
Finally, conclusions and the future work to be done
are included in Section 5.
2 CDSS INTEGRATION WITH
CLINICIAN WORKFLOW
Over the past few years, significant research in the
area of medical informatics points to the importance
of understanding workflow processes to support the
development of CDSSs for complex workspaces (Sit-
tig et al., 2008; Patel et al., 2001). Nowadays there is a
demand from the clinicians to extend the capabilities
from a pure research database towards a clinically in-
tegrated decision support system. Recent introduction
of new clinical techniques such as Minimally Invasive
Surgery (MIS) has led to several technological inno-
vations inside the Operation Room (OR). All these
advances, however, create new difficulties, such as
inadequate information transparency, limited access,
and poor visualization. Therefore, clinicians must
rely on advancements in medical imaging technology
(Dugas et al., 2002). These limitations in MIS are
constantly giving rise to new research and develop-
ment in the area of decision support systems. Such
systems are providing realtime image guidance and
task automation support while the clinician is per-
forming the intra-operative tasks (Wood et al., 2007).
Empirical studies demonstrate the benefits of includ-
ing decision support into complex workspace scenar-
ios, which lead to safer working environments and
prevention of errors (Durieux et al., 2000). Some
examples of successful applications of CDSSs into
clinical workflows comprise computer based patient
record systems (Patel et al., 2000), knowledge man-
agement systems for biomedical engineering (Rinkus
et al., 2004) and computer based training systems in
pathology (Crowley et al., 2003). Although multiple
factors are believed to affect the success or failure of
CDSS intervention implementation, a helpful CDSS
is dependent on the completeness and accuracy of the
evidence base used to support it. Also, from the suc-
cessful applications mentioned before it can be ex-
tracted that integration with workflow is key to suc-
cess. How to integrate the CDSS with clinician work-
flow, however, remains a challenge, in part because
there are no current standards for clinical workflow
(Das and Eichner, 2010).
In order to implement a workflow-based CDSS,
timing and involved subprocesses must by identified
first. Figure 1 shows a schematic workflow of an ex-
emplified operative process. Although the main in-
formation and support will be given during the intra-
operative phase, some important aspects belonging
to the pre and post-operative phases can also be in-
cluded. As Figure 1 shows, the whole procedure has
been split into tasks, a task being any particular step
taken e.g. apply anesthesia, initial puncture location
or valve final placement. Each task has a different
number of distinguishable items or attributes associ-
ated. These attributes can be described as numerical
data, text data or boolean data. During the interven-
tion execution, and according to the information be-
ing generated, the CDSS has to be capable to identify
current task in the workflow and search similar cases
HEALTHINF 2012 - International Conference on Health Informatics
202
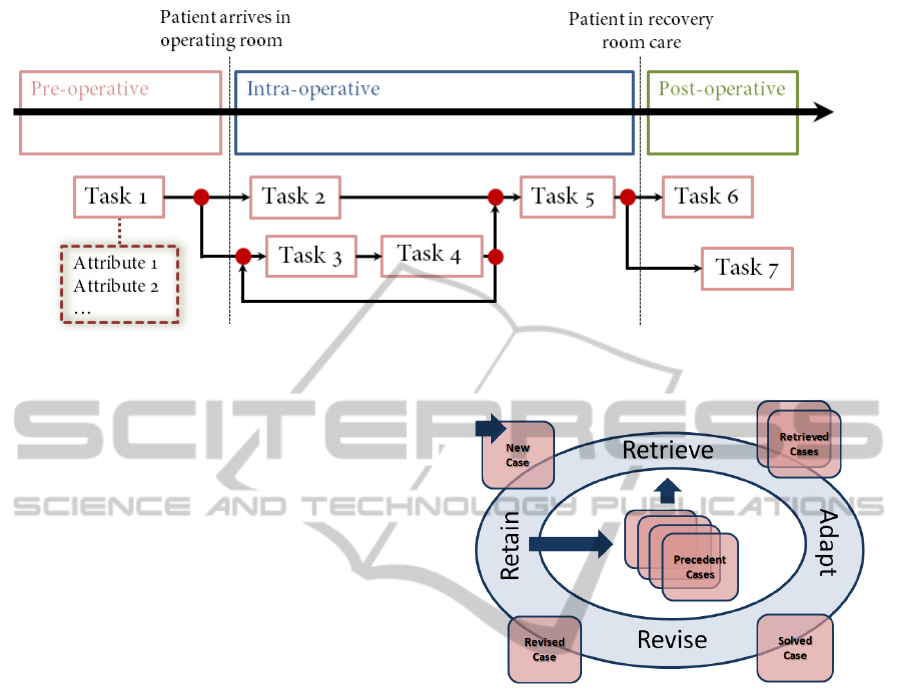
Figure 1: Schematic workflow showing an exemplified operative process.
in the case base.
The main idea of the proposed computer CDSS
is to define a case structure for every intervention
based on the operation workflow we want to give sup-
port to. With a case base of indexed past interven-
tions (organized as cases), clinicians would be able
to retrieve on-line any similar case, task or attribute
at any point along the surgical intervention together
with a formed new solution, by adapting/combining
solutions of the retrieved cases, for each of the simi-
lar cases which may help them to select the next step
properly. Also, new, revised cases will be added to the
case base for future use. The designed software will
use a CBR methodology and to give case-specific ad-
vice at any particular point of the intervention work-
flow, specially focused along preoperative and intra-
operative phases.
3 WORKFLOW-BASED CBR FOR
DECISION SUPPORT
CBR is a technique of artificial intelligence that at-
tempts to solve a given problem within a specific
domain by adapting established solutions to similar
problems (Aamodt and Plaza, 1994). As can be seen
in Figure 2, CBR has been formalized for purposes
of reasoning and learning based on the exploitation of
existing similar historical records as humans do. A
basic four-steps procedure is defined: retrieve, reuse,
revise and retain. Given a target problem, during the
retrieve step, cases from memory that are relevant to
solving it are recovered. A case is a whole although
usually two parts can be identified according to the
problem to be solved: problem and solution space.
Problem space can incorporate specific case informa-
Figure 2: Four-step process of Case-Based Reasoning.
tion and also contextual information useful for solv-
ing the problem whereas solution space incorporates
information directly related with the solution for solv-
ing the problem. While in the reuse phase, solutions
from previous cases are mapped to target the current
problem. This may involve adapting the solution as
needed to fit the new situation. Having mapped the
previous solution to the target situation, during the re-
vise step the new solution is tested and, if necessary,
checked by clinicians. After the solution has been
successfully adapted to the target problem, the retain
last step concerns with storing the resulting experi-
ence as a new case in the case base. These features
make CBR a good contender for any decision support
system (Watson, 2002). CBR has been used in other
medical decision support systems. An integration of
CBR and rule-based reasoning was used in systems
for the planning of ongoing care of Alzheimer’s pa-
tients (Marling and Whitehouse, 2001) and for the
management of Diabetes patients (Bellazi et al., 1999)
In order to design a case-based system adapted
to an operation workflow like the one described in
Section 2, we should determine a case model, case
A PROPOSAL OF A WORKFLOW-BASED CBR FOR INTERVENTIONAL CDSS - Application to Transcatheter Aortic
Valve Implantation (TAVI)
203
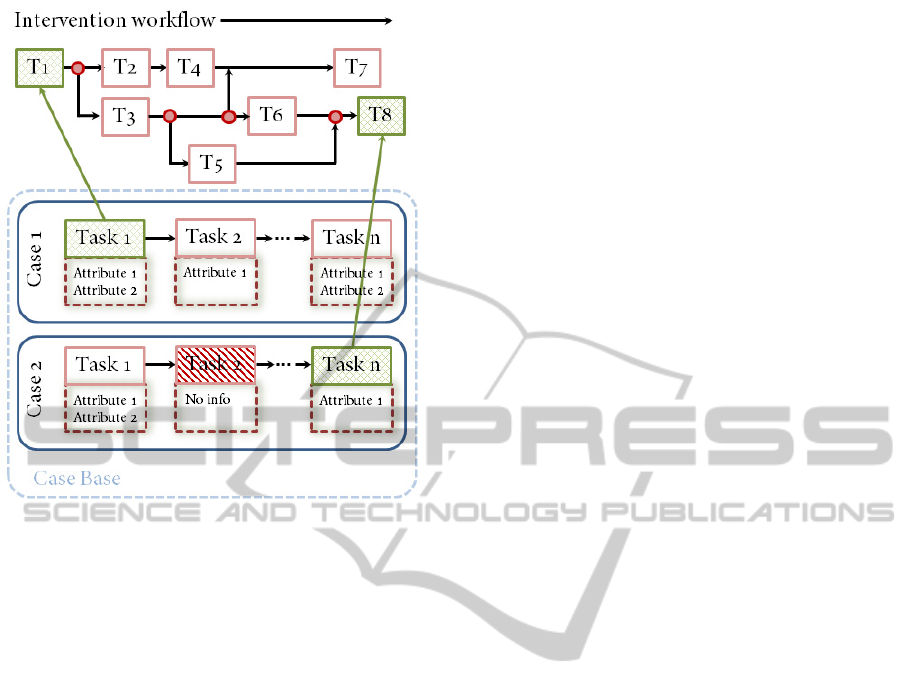
Figure 3: Case structure and retrieval process along the op-
erative workflow.
indexing and a similarity metric. As illustrated in
Figure 3, every case of the case base is defined as a
set of attributes classified among the different tasks
which compound the whole operative workflow. The
stored cases do not need to contain the same number
of attributes, as it will depend on the amount of infor-
mation available when storing each case. Therefore,
some cases will be richly filled with useful informa-
tion concerning all the tasks of the workflow while
others can be poorly defined with missing informa-
tion in certain tasks or even non-existent tasks at all,
as not all of them are mandatory and depend on each
patient.
When the intervention begins, parallel to the
workflow progression described in Figure 3, the CBR
mechanism retrieves specific and contextual problem
information of similar past cases. Such assessment
step determines which cases address problems most
similar to the current problem, to identify them as
starting points for solving the new problem. Next,
the CBR gives the clinicians information about the
solution for solving the problem by case adaptation,
which forms a new solution by adapting/combining
solutions of the retrieved problems. Once the oper-
ation ends, clinicians proceed with the new case re-
vision, which evaluates and adjusts the adapted solu-
tions and, if suitable, the new case will be retained
with the system learning from the situation by storing
the result as a new case for future use.
4 EXAMPLE OF APPLICATION:
TRANSCATHETER VALVE
IMPLANTATION
In Transcatheter Aortic Valve Implantation (TAVI)
(Webb and Cribier, 2011), a synthetic valve is trans-
ported to the heart through a small hole made in groin.
This procedure can be compared to that performed
when placing a stent, or performing balloon angio-
plasty. This technique was first developed in Europe,
where it was initially performed in 2002. Since then,
more than 10000 patients have benefit from it and the
results have shown the procedure to be effective in im-
proving functioning in the patients with severe aortic
stenosis. In the recent years TAVI is assuming a major
role in the routine management of patients with aortic
stenosis and now TAVI is considered the standard in
patients who are not candidates for conventional sur-
gical Aortic Valve Replacement (AVR). On the basis
of almost 10 years of experience TAVI also appears
to be a reasonable option for some operable, but high-
risk patients. Nevertheless considerable work needs
to be done before TAVI is expanded into lower risk
groups.
Figure 4 shows the specific workflow for the TAVI
example. As can be appreciated, the procedure (from
pre-operative to post-operative treatment) is subdi-
vided in 8 different tasks, starting with a study of pa-
tient suitability for TAVI in Task 0, to Task 7 where
the patient is finally transferred to the Intensive Care
Unit (ICU). As illustrated in Figure 4, the work-
flow does not evolve only in a forward direction but
it also turns backward if necessary, specially along
the preoperative phase, where some contraindications
could arise during the study which may turn the pa-
tient not eligible for TAVI. Parallel to the workflow
progress, as can be seen along the bottom section of
Figure 4, all the tasks are linked with the different in-
formation sources which will provide the necessary
attribute data required for defining the patient case
model. For the particular case of a MIS like TAVI,
most of the information is acquired through imaging
system devices.
As shown in Table 1, every attribute of the case
model is matched to a task or group of tasks where
clinicians consider it to be relevant or critic for the
correct development of the operative process. Also,
the attributes are linked with the source images or
monitoring sensors used to assign them a value. As
sources of different accuracy can be used to obtain
the same attribute, the information will always be pre-
sented together with its origin so the clinicians have
the last word to decide which source data is more re-
liable.
HEALTHINF 2012 - International Conference on Health Informatics
204
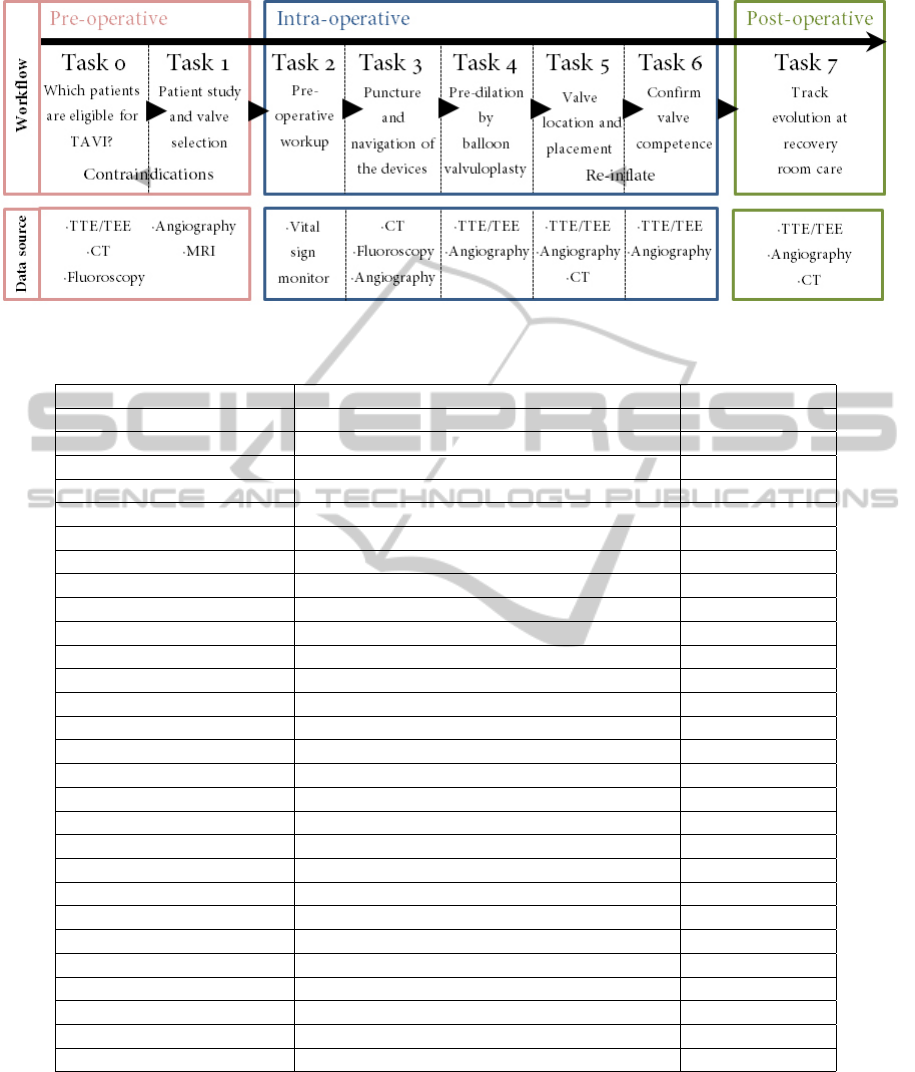
Figure 4: TAVI workflow showing tasks and data source where attributes are extracted from.
Table 1: Attributes obtained from source data and linked to the workflow tasks.
Attribute Name Task Number Data Source
Euroscore Task 0 -
Mitral regurgitation Task 0 US, A, CT, MRI
Other pathologies Task 0 US, A, CT, MRI
Vascular diameters Task 1, Task 3 CT, US, F, MRI
Calcifications Task 1, Task 3 US, F, CT, MRI
Tortuosity Task 1, Task 3 US, F, CT, MRI
Atherosclerosis Task 1, Task 3 US, F, CT, MRI
Porcelain aorta Task 1, Task 3 US, F, CT, MRI
Uncoiled aorta Task 1, Task 3 US, F, CT, MRI
Iliac stenosis Task 1 US, F, CT, MRI
Annular diameter Task 1 US, A, CT, MRI
Sinus of Valsalva diameter Task 1 US, A, CT, MRI
Ascending aorta diameter Task 1 US, A, CT, MRI
Height of coronary arteries Task 1 US, A, CT, MRI
Blood Count Task 2, Task 3, Task 4, Task 5, Task 6, Task 7 Sensor
Blood Pressure Task 2, Task 3, Task 4, Task 5, Task 6, Task 7 Sensor
Coagulation Task 2, Task 3, Task 4, Task 5, Task 6, Task 7 Sensor
Electrolytes Task 2, Task 3, Task 4, Task 5, Task 6, Task 7 Sensor
Vessel Rocked Task 3 US, F, A
Cardiac pacing value Task 4, Task 5 US, A
Inflate volume 1 Task 4 US, A
Inflate volume 2 Task 5 US, A
Valve planes Task 5, Task 6 US, A, CT
Valve leak Task 6, Task 7 US, A
Coronary flow Task 6, Task 7 US, A
Aortic/Iliac injury Task 6, Task 7 US, F
Femoral flow Task 6, Task 7 US, F
Valve completely open Task 6, Task 7 US, F
5 CONCLUSIONS AND FUTURE
WORK
The work presented in this paper details a proposal of
a CDSS designed to give case-specific assessment to
clinicians during complex surgery or minimally inva-
sive interventions.
The work progress is solid and consistent and, up
to this point, the workflow has been structured and
a case model defined together with specialized clini-
A PROPOSAL OF A WORKFLOW-BASED CBR FOR INTERVENTIONAL CDSS - Application to Transcatheter Aortic
Valve Implantation (TAVI)
205

cians. Therefore, our efforts are currently centered on
building an initial case base. For this purpose, past
cases from collaborating hospitals and medical cen-
ters have been collected and they are being translated
to match the case model previously defined. First sim-
ulated results are expected to be obtained soon be-
fore the end of the year. Also, more medical centers
have been contacted in order to spread the case base
along different hospitals within a cluster, and thus al-
lowing clinicians from different teams to consult case
problems and solutions from colleagues of other in-
stitutions. To finish, it is important to remark that the
feedback received from the numerous physicians con-
sulted has been very positive and the interest showed
in this project is encouraging. Clinicians agree that
CDSS are of high value specially in recently grow-
ing MIS like TAVI where the number of interventions
per year is still low compared to common surgery and
which also require expert hands due to its complex
procedure.
ACKNOWLEDGEMENTS
We would like to give our special thanks to the Hos-
pital Clinic of Barcelona for helping us with the case
model definition and giving us example cases of TAVI
patients. This work has been financed by the Span-
ish Government Commission Ministerio de Indus-
tria, Turismo y Comercio (MITyC) under the project
PLAN AVANZA 2 labeled by Information Technol-
ogy for European Advancement 2 (ITEA2).
REFERENCES
Aamodt, A. and Plaza, E. (1994). Case-based reasoning:
Foundational issues, methodological variations, and
system approaches. Artificial Intelligence Communi-
cations, 7:39–52.
Bellazi, R., Montani, S., Portinale, L., and Riva, A. (1999).
Integrating rule-based and case- based decision mak-
ing in diabetic patient management. In 3rd Inter-
national Conference in Case-Based Reasoning IC-
CBR’99, pages 386–400, Seeon Monastery, Bavaria,
Germany.
Berner, E. (2009). Clinical decision support systems:
State of the art. AHQR publication no. 09-0069-EF,
Agency for Healthcare Research and Quality.
Coiera, E. (October 2003). The Guide to Health Informatics
(2nd Edition). Arnold, London, UK.
Crowley, R., Naus, G., and Friedman, C. (2003). Develop-
ment of visual diagnostic expertise in pathology: An
information processing study. Journal of American
Medical Informatics Association, 10(1):39–51.
Das, M. and Eichner, J. (2010). Challenges and barriers
to clinical decision support design and implementa-
tion experienced in the agency for healthcare research
and quality cds demonstrations. AHQR publication
no. 10-0064-EF, Agency for Healthcare Research and
Quality.
Dugas, M., Schauer, R., Volk, A., and Rau, H. (2002). In-
teractive decision support in hepatic surgery. BMC
Medical Informatics and Decision Making, 2.
Durieux, P., Nizard, R., Ravaud, P., Mounier, N., and Lep-
age, E. (2000). A clinical decision support system
for prevention of venous thromboembolism: effect on
physician behavior. Journal of the American Medical
Association, 283(21):2816–21.
Marling, C. and Whitehouse, P. (2001). Case-based rea-
soning in the care of alzheimer’s disease patients. In
4th International Conference in Case-Based Reason-
ing ICCBR’01, pages 702–715, Vancouver, Canada.
Patel, V., Arocha, J., and Kaufman, D. (2001). Primer on
aspects of cognition for medical informatics. Journal
of American Medical Informatics Association, 8:324–
343.
Patel, V., Kushniruk, A., Yang, S., and Yale, J. (2000). Im-
pact of a computer-based patient record system on
data collection,knowledge organisation, and reason-
ing. Journal of American Medical Informatics Asso-
ciation, 7(6):569–85.
Perreault, L. and Metzger, J. (1999). A pragmatic frame-
work for understanding clinical decision support.
Journal of the Healthcare Information and Manage-
ment Systems Society, 13(2):5–21.
Rinkus, S., Walji, M., Johnson-Throop, K., Malin, J., Tur-
ley, J., and Smith, J. (2004). Human-centerd design of
a distributed knowledge management system. Journal
of Biomedical Informatics, 38:4–17.
Sittig, D., Wright, A., Osheroff, J., Middleton, B., Teich, J.,
Ash, J., Campbell, E., and Bates, D. (2008). Grand
challenges in clinical decision support. Journal of
Biomedical Informatics, 41(2):387–392.
Watson, I. (2002). Applying knowledge management:
Techniques for building organisational memories. In
6th European Conference in Advances in Case-Based
Reasoning ECCBR’02, pages 6–12, Aberdeen, Scot-
land, UK.
Webb, J. and Cribier, A. (2011). Percutaneous transarterial
aortic valve implantation: what do we know? Euro-
pean Heart Journal, 32:140–147.
Wood, B., Locklin, R., Viswanathan, A., Kruecker, J.,
Haemmerich, D., and Cebral, J. (2007). Technolo-
gies for guidance of radiology ablation in the multi-
modality interventional suite of the future. Journal of
Vascular Interventional Radiology, 18:9–24.
HEALTHINF 2012 - International Conference on Health Informatics
206
