
CONTINUOUS CLINICAL PATHWAYS EVALUATION
BY USING AUTOMATIC LEARNING ALGORITHMS
Carlos Fern
´
andez-Llatas
1
, Teresa Meneu
1
, Jose Miguel Bened
´
ı
2
and Vicente Traver
1
1
ITACA, Universidad Polit
´
ecnica de Valencia, Valencia, Spain
2
DSIC, Universidad Polit
´
ecnica de Valencia, Valencia, Spain
Keywords:
Process mining, Clinical pathways, Pattern recognition, e-Health, Decision support systems, Process standard-
ization.
Abstract:
The standardization of care processes in medicine, like Clinical pathways, is becoming more and more a
common practice in health care organizations. Nevertheless, their design is not an easy task. Some approaches
in the literature are based on using Workflow technology for defining Clinical Pathways. These approaches
allow the creation of unambiguous, complete and automatically executable protocols. In addition to this, the
use of Process Mining technology can help the design using information from real executions of Clinical
Pathways cases. Nevertheless, to ensure a correct continuous evaluation and improvement of care processes,
the creation of a tool that allows to know the current status of the Clinical Pathway execution it’s mandatory. In
this paper, we present a tool able to compare the designed Clinical Pathways with the real implantation cases
in order to detect their differences. This allows Clinical Pathways designers to improve the care protocols
making them more adequate to real cases.
1 INTRODUCTION
Nowadays, current trends on process management are
focused in the standardization of processes in order
to evaluate and improve the strategy to achieve bet-
ter quality and efficiency in most common actions. In
Health environments, the care processes standardiza-
tion is becoming more and more present. The use
of standardized protocols, for normalizing the care
process, like Clinical Pathways (Audimoolan et al.,
2005) is more and more adopted by health profession-
als in order to improve the quality of care of patients.
The use of Clinical Pathways for Health Care stan-
dardization is a difficult task. Clinical Pathways are
usually multidisciplinary complex documents that co-
ordinate the actions of patients, doctors and the rest of
involved care process stakeholders. In order to create
efficient care protocols it’s necessary to avoid ambi-
guity, describe completely the whole problem and fa-
cilitate the use of ICT (Information and Communica-
tion Technologies) to make the system usable.
The use of Workflow Technology (WfMC, 1999)
can help doctors to design formal, non ambiguous and
automatically executable care protocols to describe
complete Clinical Pathways. In addition, the Process
Mining technology can be used to automatically infer
workflows to facilitate the design of the processes in
a formal way (Fern
´
andez-Llatas et al., 2010).
Nevertheless, the control of the implantation of
Clinical Pathways requires a high level view that sup-
ports the detection of inefficient processes and bottle-
necks. This paper presents a tool created to facilitate
this management and to evaluate the fitness of execut-
ing Clinical pathways by automatically comparing the
real execution care protocols cases with the designed
Clinical Pathway. This tool uses Pattern Recognition
techniques to detect and quantify exceptions occurred
in real cases. These exceptions are divergences from
the ’expected’ path that was designed and the real per-
formance that can be later analyzed by the healthcare
organizations and corrected if needed and possible.
The paper is structured in the following way.
Firstly the solution to Clinical Pathway design us-
ing Workflow languages in described. The following
section explains how process Mining techniques can
be used to help the design of Workflow based Clin-
ical Pathways. Following this, a tool for the contin-
uous evaluation of ongoing Clinical Pathways is pre-
sented. The last part summarized the conclusions of
this work.
228
Fernández-Llatas C., Meneu T., Benedí J. and Traver V..
CONTINUOUS CLINICAL PATHWAYS EVALUATION BY USING AUTOMATIC LEARNING ALGORITHMS.
DOI: 10.5220/0003153902280234
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2011), pages 228-234
ISBN: 978-989-8425-34-8
Copyright
c
2011 SCITEPRESS (Science and Technology Publications, Lda.)

2 CLINICAL PATHWAYS AS
HEALTH CARE
STANDARDIZATION MODELS
Since the appearance of the Evidence Based
Medicine(EBM) paradigm (Elstein, 2004) that was
born in the early 90’s, the works focused on ap-
plying the scientific method to medical research are
each year growing significantly. The idea of stan-
dardizing health care processes is more and more
adopted to improve daily actions of nurses, doctors
and the rest of stakeholders. In some of the most
commons medical knowledge public repositories, like
COCHRANE (The Cochrane Collaboration, 2010) or
PubMed (PubMed Library, 2010), it’s possible to find
detailed care protocols to address the management of
almost any disease. These standardized health care
protocols, also known as Clinical Pathways (Audi-
moolan et al., 2005), deeply describe all the steps that
patients, doctors, nurses and the rest of the stakehold-
ers must follow to perform the care process efficiently
and efficaciously.
These protocols are usually described in natural
language. This is due to the high expressivity needed
by Health professionals to describe care protocols.
The situations that a Clinical Pathway can express
are very complex. However, this use of natural lan-
guage supposes a big problem when moving to Clini-
cal Pathways interpretation. Natural language models
have clear ambiguity problems. Different health pro-
fessionals can understand the same phrase in totally
different way. This situation can lead to an erroneous
interpretation of a Clinical Pathway that might affect
the patient’s quality of care. In addition to this, defin-
ing Clinical Pathways using natural language does not
allow to ensure that the process is completely defined.
In that case, it’s possible that the process has unde-
fined states that must be lucubrated by health profes-
sionals.
Other reason to avoid natural language in Clinical
Pathways design it’s the impossibility that this bring
to the automatic execution of guidelines. Currently,
the healthcare organizations are more and more com-
puterized and the data is each time more available
in digital way. The use of dynamic systems that al-
low the computerized guidance of the health profes-
sional in the care process following the Clinical Path-
ways description will suppose a crucial help to the
deployment of those protocols. This is important be-
cause, in some cases like multidisciplinary protocols,
the high bureaucratic load and the required coordina-
tion of specific teams demands the use of computer
systems in order to allow the standardization of pro-
tocols. Natural language is not understood by com-
puters. For that reason, in order to create systems en-
abling the guidance of health professionals with auto-
matic guidelines it’s necessary to translate the process
definition to a formal language that could be executed
automatically.
There are some efforts in literature focused in ad-
dressing this problem. Some high level languages
have been defined to formally describe Clinical Path-
ways: GLIF language (Peleg et al., 2001) was de-
fined to describe and evaluate health care protocols;
In Carepaths project (Naranjo et al., 2006) an ontol-
ogy for describing and automatically executing Heart
Failure Clinical Pathways was developed. Other
works are purely based on Workflow technology to
describe general purpose and high expressivity lan-
guages for Clinical Pathways definition (Dominguez
et al., 2008).
Workflow Technology is a research field focused
on the creation of process specification languages and
its dynamic execution. A Workflow is defined as the
automation of a business process, in whole or part,
during which documents, information or tasks are
passed from one participant to another for action, ac-
cording to a set of procedural rules (WfMC, 1999).
A Workflow is a formal description of a process de-
signed to be automated. A Workflow language is a
formalism that allows the definition of Workflows. A
formal Workflow can be automatically executed in a
computerized system by using a Workflow Engine.
This will allow the automatic execution of standard-
ized protocols and the guidance of processes in com-
puterized environments.
The advantages of the use of Workflow technology
over other techniques in Clinical Pathways definition
are several. In the literature, we can find available
some Workflow engines for automatic execution of
processes like jBPM from jBoss or Workflow Foun-
dation from Microsoft. Workflow languages have a
great understandability. The majority of Workflow
Languages have a graphical view and it’s possible to
design the execution of processes. A graphical defini-
tion of a Workflow can be seen on Figure 2. In addi-
tion, there is the possibility to measure the expressiv-
ity of a Workflow language according to the Workflow
Patterns (van der Aalst et al., 2003a) to decide the
most adequate language to be used in the formal de-
scription. Workflow Patterns are flow structures that
describe the state change rules in a process. Examples
of Workflow Patterns are sequences, choices, paral-
lel actions... etc. The more Workflow Patterns a lan-
guage is able to define, the better expressivity it has.
CONTINUOUS CLINICAL PATHWAYS EVALUATION BY USING AUTOMATIC LEARNING ALGORITHMS
229

07/05/2010 10:22:59 => i:1 BeginAction: Admission
07/05/2010 10:34:01 => i:1 EndAction: Admission Res: OK
07/05/2010 10:35:03 => i:1 BeginAction: Triage
07/05/2010 10:46:06 => i:1 EndAction: Triage Res: InHospital
07/05/2010 10:56:07 => i:1 BeginAction: TNS
07/05/2010 10:56:08 => i:1 BeginAction: TMP
07/05/2010 11:23:10 => i:1 EndAction: TNS Res: OK
07/05/2010 11:33:12 => i:1 EndAction: TMP Res: Fever
07/05/2010 11:43:19 => i:1 BeginAction: TMP
07/05/2010 11:50:19 => i:1 EndAction: TMP Res: OK
07/05/2010 11:51:24 => i:1 BeginAction: QualityTest
07/05/2010 12:00:28 => i:1 EndAction: QualityTest Res: OK
07/05/2010 12:15:29 => i:1 BeginAction: Discharge
07/05/2010 12:20:30 => i:1 EndAction: Discharge Res: OK
Figure 1: Example of Clinical Pathway case log.
3 PATTERN RECOGNITION
TECHNIQUES FOR CLINICAL
PATHWAYS AUTOMATIC
LEARNING
The use of Clinical Pathways does not ensure that the
processes was always executed in the same way. In
this line, it’s very common that the care process of a
patient is changed during execution. This change can
be motivated by the daily problems in the care process
(like administrative errors, malfunctioning or unavail-
ability of devices to perform medical tests described
on the care protocol, etc) and the variability of the
patient illnesses. For example, a pluripathologic pa-
tient can suffer changes in his treatment protocol due
to an allergy or due to contraindications of the pro-
tocol with the recommendations for other illness not
documented on that Clinical Pathway.
These exceptions to the care protocol can be
very useful to detect design problems in the Clin-
ical Pathway or underperformance of the care pro-
cesses. Knowing that information would enable the
correction and fine-tuning of the Clinical Pathways in
an iterative process. The correction could be done
in the design or in the real execution problem, de-
pending on the cause for the divergences but the im-
portant touch-point would be to know when, how
and under which conditions those divergences hap-
pen. Using this model on each iteration the errors
detected will be used to correct the Clinical Path-
way that will be changed for the next iteration. This
problem can be approached in an automatic way us-
ing Process Mining Technology. The Process Min-
ing idea (also known as Workflow Mining) (van der
Aalst et al., 2003b) is the automatic learning of Work-
flows for business process inference. Process Min-
ing algorithms use the execution samples to infer the
Workflow that describe the real process. Using this
technique the logs of care protocols actions applied to
each patient can be used to learn Workflows that for-
mally represent those Clinical Pathways. This helps
Clinical Pathways designers to modify previous iter-
ation processes according to the real deployment in-
corporating the new exceptions and correcting design
errors.
In (Fern
´
andez-Llatas et al., 2010) a Process Min-
ing algorithm (called PALIA) has been proposed to
discover the execution model of the Clinical Pathway
from the data gathered about the actions executed of
the patient past cases. This algorithm takes as en-
try data information about the activities performed by
Clinical Pathways stakeholders in a case assigned to
a patient.
Figure 1 shows an example of the logs of activities
in a case. This log is composed by a set of events that
represents begin action and end action events. The be-
gin action event has the identification of the case, the
name of the action and the time when the action was
started. The end action event has the identification of
the case, the name of the action, the time when the
action was finished and the result of this activity.
Analyzing a set of samples like the shown in Fig-
ure 1, using Pattern recognition techniques, PALIA
algorithm is able to infer automatically a Workflow
like the shown in Figure 2. This Workflow repre-
sents a model that resumes graphically all the possible
flows that the log samples can follow. This formally
defined Workflow can be used by Clinical Pathway
designers as the basis for the description of a formally
defined care protocols that explains all the situations
that can occur in reality in a concrete scenario.
Nevertheless, these techniques can be used not
only for helping design of Clinical Pathways but also
to support the continuous evaluation of them. This
allows comparing formal protocols to detect differ-
ences between the designed and the executed one and
facilitate the detection of problems in individual or
HEALTHINF 2011 - International Conference on Health Informatics
230
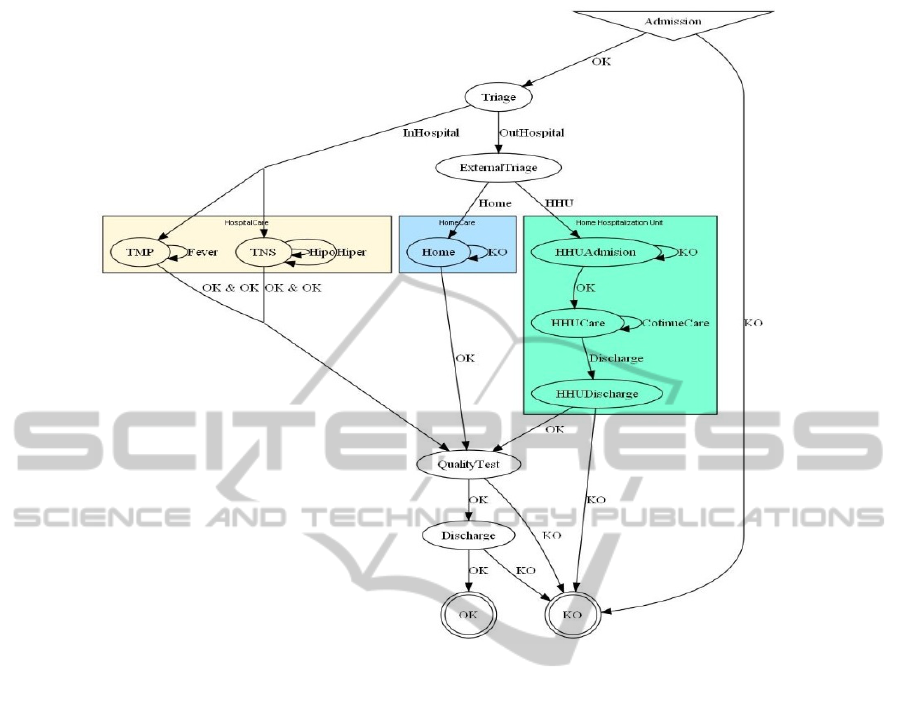
Figure 2: Original Clinical Pathway deployed.
population cases to improve the efficiency. Further-
more, it provides a guideline for managers to under-
stand the reasons for incompliance to protocols and
evaluate if the compliance support strategies put in
place are followed. This is also an important achieve-
ment as compliance of health professionals to care
processes whenever is possible is highly desirable.
Consequently, to allow the use of the described tech-
niques in Clinical Pathways Evaluation, it’s necessary
to create a software tool that incorporate those tech-
niques to allow the inference and evaluation of ongo-
ing Clinical Pathways.
4 USING PROCESS MINING
TECHNIQUES IN CLINICAL
PATHWAYS EVALUATION
In this paper, a tool for Process Mining use in Clini-
cal pathways Evaluation is presented. This prototype
was developed in the framework of the Heart Cycle
European project (Heart Cycle Consortium, 2008).
This tool has some mining algorithms to allow
Clinical Pathway designers to detect errors on execu-
tion time and helps the refinement and redesign of the
process in order to improve the efficiency and efficacy
of the systems.
Basically, the tool has two kinds of algorithms im-
plemented.
• An Activity-Based Process Mining algorithm was
implemented to discover the whole process that
is occurring in its real execution. The algo-
rithm implemented is based on Parallel Activity-
based Log Inference Algorithm(PALIA) defini-
tion (Fern
´
andez and Bened
´
ı, 2008).
• Two algorithms able to compare the original pro-
tocols with the inferred one were implemented.
The first algorithm is able to compare two work-
flows to detect differences between them. This
algorithm is based in classical Error Correct-
ing techniques (Rulot and Vidal, 1987) based on
grammar inference theory. The Second algorithm
is able to compare a workflow with a individual
case. This algorithm will allow the systems to
show the path followed by the case in the Clini-
cal Pathway flow.
To allow the interaction of the tool with other
Workflow management systems the tool admits dif-
CONTINUOUS CLINICAL PATHWAYS EVALUATION BY USING AUTOMATIC LEARNING ALGORITHMS
231
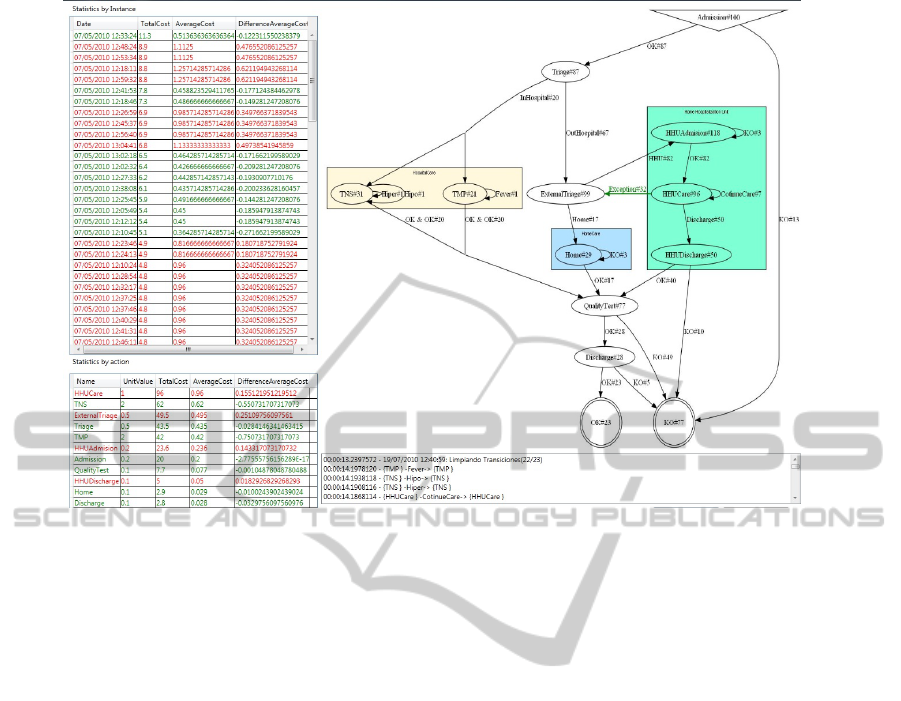
Figure 3: Clinical Pathway Inferred compared with the Designed one.
ferent input and output formats. The tool imple-
mented accepts log process samples codified in plain
Activity-based Log Format (Fern
´
andez and Bened
´
ı,
2008) or in extended MXML format (van Dongen
et al., 2005) for Activity-Based Logs. The graphi-
cal flows inferred can be exported to dot format (Ell-
son et al., 2004), TPA format (Fern
´
andez and Bened
´
ı,
2008) and, as a Petri Net, to PNML format (Billing-
ton et al., 2003).
To explain the functionality of the tool, a Clin-
ical Pathway and some evaluation samples will be
used. This example will be widely explained to show
how the application uses Process Mining techniques
to evaluate the execution of Clinical Pathways.
For this experiment a simplification of a general
triage process in a Hospital was used. The formal
care protocol used in the experiment is shown in Fig-
ure 2. This protocol was specifically selected because
resumes the most complex Workflow Patterns that are
used in Workflow Patterns according the experience
acquired in Heart Cycle Project (Heart Cycle Con-
sortium, 2008). This Protocol combines the use of
action sequences, parallel activities and joins as well
as complex multichoice Workflow Patterns (van der
Aalst et al., 2003a).
The Clinical Pathway of the Figure 2 shows a
triage process in a hospital A modification of that pro-
tocol has been used to simulate 100 samples using a
Workflow simulation engine (Fern
´
andez et al., 2008).
Each one of these samples represent a real execution
of the designed protocol. In order to be more realis-
tic in the simulation, the Clinical Pathway simulated
is not exactly equal to base. This allows to represent
how the system detects cases in which the patient does
not follow exactly the same path in the Clinical Path-
way. In this way, in our experiment, on one hand the
protocol will represent the Clinical Pathway designed
to be evaluated, and in the other hand the 100 cases
will represent 100 patients assigned to the protocol.
The first step to follow for Evaluating a Clinical
Pathway using the Heart Cycle Pathway Evaluation
tool is to discover the Clinical Pathway that repre-
sents the real protocol described by the 100 patients
assigned to the protocol. In order to do that, the 100
samples are used to infer the real Workflow to be com-
pared with the designed one. The Workflow algorithm
implemented in the tool allows do that.
Figure 3 shows the results offered by the tool. At
the right of the screen it’s possible to see the compar-
ison between the original workflow and the inferred
one. In that image, the transitions and states are la-
belled with numbers. This represents how many times
this state or transition has been accessed. This allows
Clinical Pathways designers to discover bottle necks
and unused actions to make more efficient and sim-
plify the Clinical Pathway’s Design. In this case, it’s
easily detected that only the 23% of samples complete
the care protocol until the end. Other important data
that can be deduced of this example is that the major-
ity of patients are derived to HHU (63 of 87).
HEALTHINF 2011 - International Conference on Health Informatics
232
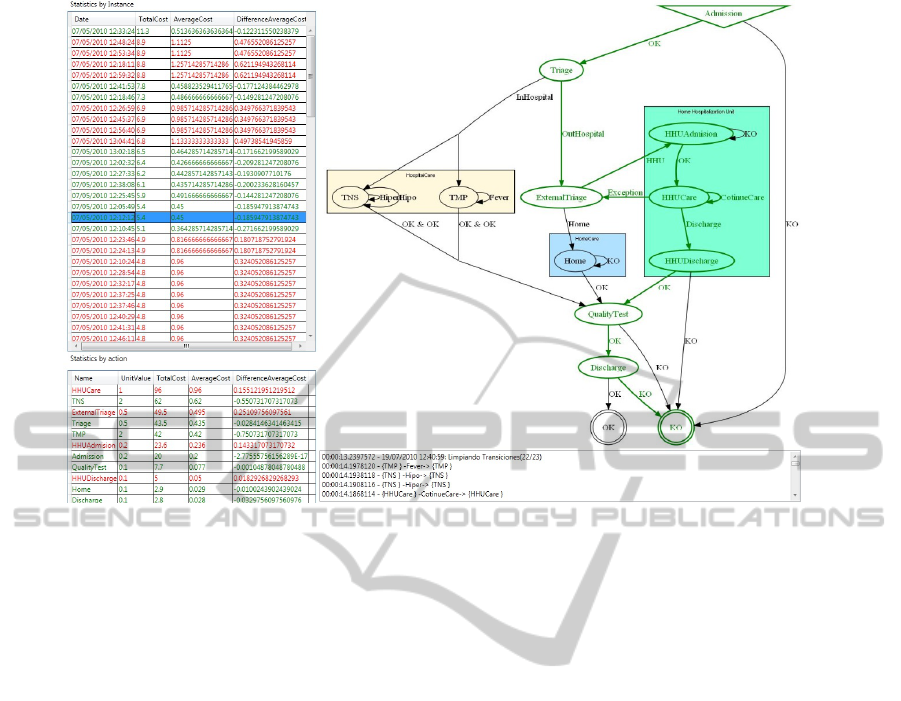
Figure 4: Clinical Pathway Instance path view.
In this example, it is shown how Clinical Pathways
exceptions affect the Protocol execution. In the exam-
ple, 32 executions of the 82 cases that are assigned for
HHU Care are returned to External Triage. This step,
not covered by the original Workflow, is shown in the
example as a green arrow. With this information, the
Clinical Pathways designer can deduce that there is
an error on External Triage or HHU Admission pro-
cess that makes inefficient the HHU Unit producing
an high percentage of exceptions in the HHU Care
process. Then will be the role of the manager of the
process to find the best solution for this divergence,
but the proposed tools has highlighted where it hap-
pens and can reproduce and analyze the conditions in
which it happened: typology of patients, time or date
frames, specific teams or professionals, etc.
In the left part of the screen some statistical in-
formation can offer more data about the efficiency
level of the Clinical Pathway execution. The upper
part shows information about the 100 execution cases.
Each one of the actions of the Clinical Pathway has
assigned a relative cost. Using that information the
system can calculate the total cost of each case and
shown they ordered. In addition, the average of cost
by action made in a case is also show. This allow to
detect the kind actions that has a bigger relative per-
centage cost. To make easier the detection of groups
of deficitary cases, the application shows in red the
cases that has an average cost below the mean, and
marks in green those that has an average cost over the
mean.
The lower part shows statistical information about
the actions executed in all the cases. In that case, it
is shown the relative cost of an action executed in all
the cases, and the average cost by case. In the same
way, the application shows in red the actions that has
an average cost below the mean, and marks in green
those that has an average cost over the mean. This
information allows detecting which actions are more
used and its usual cost in their global execution.
In order to facilitate the detection of inefficient
cases, the application allows to Clinical Pathways de-
signers the single view of a patient case. In this case,
selecting a case from the left instances list with the
mouse, the correspondent flow is shown on the right
Figure 4 shows an example of how a Clinical Path-
way execution is displayed in the application. The
Workflow shows in green the states and arrows that
are followed by the selected case. This allows health
professionals to detect punctual errors in individual
cases and how those errors affect patients. In this
example, the case does not follow exactly the Clini-
cal Pathway originally designed and provokes an ex-
ception in HHU care process returning to External
triage process and, after that, returning other time to
HHU Admission process. In the example, a simu-
lated administrative error provokes the exception that
throws out the patient from HHU that finally was de-
tected and corrected by External Triage process. In
that case, the health professionals can revise the HHU
Care process rejection protocol to detect possible er-
rors.
CONTINUOUS CLINICAL PATHWAYS EVALUATION BY USING AUTOMATIC LEARNING ALGORITHMS
233

5 CONCLUSIONS
In this paper, a tool for the continuous evaluation
of Clinical Pathway deployment is presented. This
tool is able to compare real execution cases with the
theoretical designed Clinical Pathways. This allow
to easily discover the differences between the care
protocols predefined and how they are actually ap-
plied. This allows Health professionals detect inef-
ficient processes, exceptions, inconsistencies and bot-
tlenecks in the designed Clinical Pathways or to iden-
tify possible problems in the organization that prevent
the efficient work of the care teams. In addition to
this, the application offers the possibility to associate
cost measurements to the actions and have a view of
the process relative costs in order to quantify the inef-
ficiency of the system.
The tool has been tested in laboratory conditions
using a simulated Clinical Pathway and a set of cases
to achieve a first evaluation of the system capabilities.
This tool is currently in evaluation and it is
planned to be validated in real systems in Hearth
Cycle (Heart Cycle Consortium, 2008) European
project.
REFERENCES
Audimoolan, S., Nair, M., Gaikward, R., and Qing, C.
(2005). The role of clinical pathways. Improving Pa-
tient Outcomes, February:–.
Billington, J., Christensen, S., Van Hee, K., Kindler, E.,
Kummer, O., Petrucci, L., Post, R., Stehno, C., and
Weber, M. (2003). The petri net markup language:
concepts, technology, and tools. In ICATPN’03: Pro-
ceedings of the 24th international conference on Ap-
plications and theory of Petri nets, pages 483–505,
Berlin, Heidelberg. Springer-Verlag.
Dominguez, D., Fern
´
andez, C., Meneu, T., Mocholi, J. B.,
and Seraffin, R. (2008). Medical guidelines for the
patient: Introducing the life assistance protocols. In
Computer-based Medical Guidelines and Protocols:
A Primer and Current Trends, volume 139, pages
282–293. IOS Press.
Ellson, J., Gansner, E., Koutsofios, E., North, S., and Wood-
hull, G. (2004). Graphviz and dynagraph – static
and dynamic graph drawing tools. In Junger, M. and
Mutzel, P., editors, Graph Drawing Software, Math-
ematics and Visualization, pages 127–148. Springer-
Verlag, Berlin/Heidelberg.
Elstein, A. (2004). On the origins and development of
evidence-based medicine and medical decision mak-
ing. Springer, ago 2004:184–189.
Fern
´
andez, C. and Bened
´
ı, J. M. (2008). Timed parallel
automaton learning in workflow mining problems. In
Ciencia y Tecnolog
´
ıa en la Frontera, number special
2008, pages 181–187.
Fern
´
andez, C., Sanchez, C., Traver, V., and Bened
´
ı, J. M.
(2008). Tpaengine: Un motor de workflows basado
en tpas. In Ciencia y Tecnolog
´
ıa en la Frontera
ISSN:1665-9775.
Fern
´
andez-Llatas, C., Meneu, T., Bened
´
ı, J. M., and Traver,
V. (2010). Activity-based process mining for clinical
pathways computer aided design. In Proceeding of
the 32nd Annual International Conference of the IEEE
Engineering in Medicine and Biology Society.
Heart Cycle Consortium (2008). Vii framework program
ist project 216695:compliance and effectiveness in hf
and chd closed-loop management 2008-2011.
Naranjo, J. C., Fernandez, C., Pomes, S., and Valdivieso, B.
(2006). Care-paths: Searching the way to implement
pathways. Computers in Cardiology, 33:285–288.
Peleg, M., Boxwala, A. A., Bernstam, E., Tu, S. W.,
Greenes, R. A., and Shortliffe, E. H. (2001). Sharable
representation of clinical guidelines in glif: Relation-
ship to the arden syntax. Journal of Biomedical Infor-
matics, 34(3):170–181.
PubMed Library (2010). National library of medicine
and the national institutes of health pubmed library:
http://www.pubmed.gov.
Rulot, H. and Vidal, E. (1987). Modelling (sub)string-
length based constraints through a grammatical infer-
ence method. In Proc. of the NATO Advanced Study
Institute on Pattern recognition theory and applica-
tions, pages 451–459, London, UK. Springer-Verlag.
The Cochrane Collaboration (2010). Cochrane library:
http://www.cochrane.org/index.htm.
Van der Aalst, W. M. P., Barros, A. P., ter Hofstede, A.
H. M., and Kiepuszewski, B. (2003a). Workflow pat-
terns. Distributed and Parallel Databases, page 70.
Van der Aalst, W. M. P., van Dongen, B. F., Herbst, J.,
Maruster, L., Schimm, G., and Weijters, A. J. M. M.
(2003b). Workflow mining: A survey of issues and
aproaches. Data and Knowledge Engineering 47
2003, pages 237–267.
Van Dongen, B. F., de Medeiros, A. K. A., Verbeek, H.
M. W., Weijters, A. J. M. M., and van der Aalst, W.
M. P. (2005). The prom framework: A new era in pro-
cess mining tool support. In ICATPN, pages 444–454.
WfMC (1999). Workflow Management Coalition Terminol-
ogy Glossary. WFMC-TC-1011, Document Status Is-
sue 3.0.
HEALTHINF 2011 - International Conference on Health Informatics
234
